Introduction
Central position of the nose on human face is an obvious fact frequently pointed out in rhinoplasty literature. Nasal tip, being the most prominent part of the nose, attracts the eye, making any imperfection in this region potential concern for a rhinoplasty patient. Broad, bulbous tip with its’ disproportion in width between the nasal dorsum has been a surgical challenge since the first rhinoplasty was performed. Correction of this deformity demands understanding of the etiology, thorough diagnosing of the causes, and very often requires a large palette of surgical techniques, sometimes its’ variations, apart from artistic skills to achieve a desirable result.
As rhinoplasty remains the most challenging of all aesthetic operations, no two procedures are ever identical. This makes each rhinoplasty unique, dependable from individual nasal configuration, requiring humility even from a master surgeon who should be prepared for the varied anatomic patterns encountered, especially in the nasal tip region.
Deformity
Bulbous tip is particular appearance of a wide nasal tip most often disproportional in width with the nasal dorsum. This may result from poorly defined, hypertrophic lower lateral cartilages, with round shape of the domes, skin quality and thickness, cartilage strength (Fig. 1,2). 20
 |  |
| A | B |
Figure 1. Bulbous nasal tip of the same patient (A, B). B: intra-op picture of poorly defined, hypertrophied lower lateral cartilages.
Generally various abnormalities falls under the umbrella of a bulbous tip such as: broad, boxy, bifid, bulbous, trapezoid, amorphous.
Diagnosis & analysis
Before analyzing the deformity major aesthetic components of the face should be considered, especially eyes, lips, forehead and chin, to plan a surgical strategy that will allow to achieve the most balanced and harmonious position of the nasal tip possible. Thorough examination, containing palpation and inspection, evaluation of tip support (tip recoil), shape and size of alar cartilages, is the first step on a pathway to the patients’ desires. Next very important step is standardized photographic documentation, usually consisting of at least 9 standard views.
Most frequently bulbous nasal tip has strong lower lateral cartilages with thin skin and soft tissue envelope sometimes resulting in distinctive bifidity, especially visible on a three quarter pre-op pictures as a light shadow in between the domes (Fig. 2).

Figure 2. Three quarters view of the bifid bulbous tip.
From the basal view it forms a trapezoidal or rectangular configuration. This does not allow to delineate the tip on an equilateral triangle (Fig. 3). Additionally picture analysis shows increase in both angles of definition and divergence (Fig. 5).
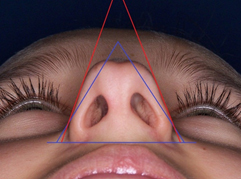
Figure 3. Basal view of the bulbous tip with triangles used in nasal analysis. Equilateral triangle (blue) and triangle drawn on the existing shape of the tip (red).
The reverse situation – weak cartilages and thick skin is usually common in patients of Asian and African descent and is very difficult to correct. Sometimes the bulbous nasal tip is formed by combination of thick nasal tip skin/soft tissue cover and strong cartilages.
On the frontal view base of the broad tip is most often wider than standard vertical 1/5 of the face (Fig. 4), which at times requires some adjunctive surgical maneuvers.

Figure 4. Broad base of the bulbous tip. Nasal alae extending outside vertical 1/5 of the face.
Most commonly bulbous nasal tip has an increase in distance between tip defining points greater than 4mm and/or angle of divergence over 30 degrees º (Fig. 5).
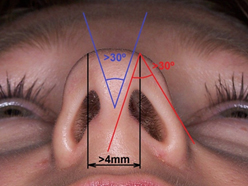
Figure 5. Distance between tip defining points (black), angle of definition (red) and angle of divergence (blue).
Surgical strategy
Each tip anatomy needs individual strategy. There is no universal rule but there are at least a few guiding principles:
- tip supporting mechanisms and tip dynamics should be considered in the operating plan
- correction should be done in the least traumatic and at the same time the most predictable way
- anatomical structure of the tip should be maintained or surgical anatomy created should mimic the nature
- tissue preservation, remodeling and reorientation is much better solution than resection
Tip supporting mechanisms are crucial in preserving structural integrity of the tip. Being aware of them surgeon can influence the shape of the tip, creating a long lasting result, both esthetically and functionally optimal.
Surgical treatment
There might be no adequate distinction between incisional “approach” and surgical “technique” in the rhinoplasty literature. It is, however, of a less importance what approach has been used but what technique has been utilized to modify nasal tip cartilages. Probably each surgeon develops preferred incisional approaches in which he may gain dexterity and excellence. In the author’s opinion most convenient approach in seriously bulbous tip is external. Although mild bulbosity might be approached endonasaly through transcartilaginous (cartilage splitting, intracartilaginous) incision, intercartilaginous or infracartilaginous incision1. In selected cases conservative, limited cephalic reduction of the lateral crus can give a desirable result by weakening the cartilage and allowing it to bend.
(movie 1)
As it has been said: “it is not important how much has been taken but what is left behind” – this sentence is very good representation of one of the open questions in rhinoplasty– how much cartilage of the lateral crurae should be preserved. It seems that if there is no abnormal weakness of the cartilage, 6-8 mm should be enough to maintain support of the external valve and resist contractile healing forces. Nonetheless each case should be judged individually.
Vast majority of wide tips can be successfully treated through the external approach. Endonasal approach utilizing intercartilaginous and marginal incisions and delivering of the lower lateral cartilages within domal regions is, in some hands, very elegant alternative for the open approach5. However such approach demands at least a bit of pressure on the cartilages and skin/soft tissue envelope during the procedure, making the anatomy distorted from its’ natural position at the time of sculpturing cartilaginous framework. Opening the tip gives the opportunity to see the pathology in its’ genuine configuration. This also allows to observe immediate effect of all surgical maneuvers on the tip shape and position7.
There are generally four ways to treat bulbous tip surgically:
- volume reduction
- suture control
- transection/partial excision (interrupted strip)
- grafting
Tip fullness is decreased by cephalic trim as shown on the movie, which at the same time rotates the tip upward (depending on the amount of cartilage resected).
(movie 2)
Surgeon should be aware that resection of the cephalic part of the lateral cartilage will induce upward rotation not only of the tip alone but also of the rim of the nostrils, increasing columellar show, which at times should be addressed simultaneously. Volume reduction alone, however, being effective in mildly bulbous tips and mainly achieved by influencing two of the main tip supporting mechanisms (1-contour, size and strength of the lower lateral cartilages and 2-scroll region), should rarely be a target maneuver in external rhinoplasty in more severely bulbous tips. This requires multiple surgical techniques and ability to use a number of them in combination is critical6,7. Besides lateral crurae can be successfully trimmed endonasaly with less trauma, as described above. Sometimes bulging of the remaining lateral crus may tempt to use weakening procedures (scoring or morselization). In the authors’ opinion these techniques are difficult to control intraoperatively and they rely too much on healing unpredictability.
At times skin thickness may require some fine thinning as shown on the movie.
(movie 3)
Surgeon should be aware that blood supply runs right beneath the tissue which is trimmed during this procedure. It is extremely important to preserve the blood flow. Being too aggressive may end up with skin necrosis. In selected cases examining the skin with ultrasound (USG) may be helpful.
Conservative cephalic trim with horizontal-mattress suture technique is probably one of the most popular ways to appropriate correction of the bulbous nasal tip. This can be done with a nonabsorbable (Prolene, Gore-Tex) or slow absorbable (PDS) sutures, usually of 5.0 gauge. Sutures are placed to narrow the dome area, separately on each dome, starting medially and progressively tightened until the desired configuration is achieved. Care is taken to place them symmetrically.
(movie 4)
As shown on the movie, stitches should be left long on each side so they can be finally tied together, narrowing distance between tip-defining points and decreasing angle of divergence. Knots should be buried between the domes. In majority of bulbous tips there is poor or almost no definition within the domes so these sutures are often used to create new domes. Binding the domes usually increases projection about 0.5-1.5 mm. Placing the sutures slightly lateral, in a “lateral crural steal” manner8 may also rotate the tip upward. Alternatively, a single interdomal stitch can be used in case of acceptable symmetry and weaker cartilage.
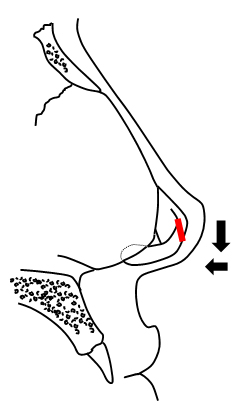
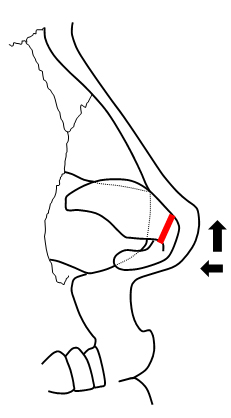
Interrupting the continuity of lower lateral cartilage brakes the spring of the cartilage and results in immediate narrowing the tip by repositioning of the lateral crus. Transection can be located within the domes or lateral to them. Vertical dome division (techniques described by Goldman or Simons)2,3,4 can be done endonasaly. However limited stability of transected elements of the lower lateral cartilages may sometimes result with possible asymmetrical healing, loss of support and increased rotation caused by scar contracture in the long term follow-up. Suture reconstitution of the divided segments can be done in various fashion such as end to end or by overlapping elements and provides improved control of healing and improved stability of long-term structure, modifying the location of the domes and altering tip projection and rotation at the same time10. The “tripod concept” is probably the best model for simple description of tip dynamics in such circumstances – dividing the cartilage medially from the dome will deproject and rotate the tip down (Fig. 6, A), dividing it laterally will also deproject but at the same time rotate the tip up (Fig. 6, B).
 |  |
| A | B |
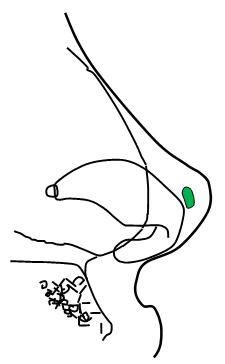
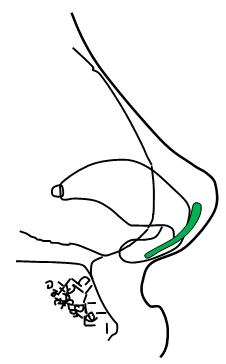
Figure 6. Interruption of the cartilage strip (red) medially from the dome (A) and laterally from the dome (B).
At times a small amount of cartilage can be resected from the lateral crurae in order to further decrease tip volume and projection. Suture reconstitution is necessary in each case. Resection can be positioned at the domes (movie 4) or just lateral from them.
(movie 5)
Both locations are of a similar effectiveness but they have also got their “dark sides”. Domal position of resection may potentially create visible stigma – sharp edges of the cartilage can show up through the skin in the long term follow up. Fine sculpturing of sutured cartilage edges and optionally covering the tip region with crushed cartilage onlay graft may prevent such complication. Although resecting part of the lateral crus laterally from the dome leaves the dome intact but at the same time weakens the spring of the lateral crural cartilage. Thus may impair external valve strength if put too much laterally and sutured end to end. Lateral crural overlay with the medial portion of the lower lateral crus overlapping lateral aspect of the cartilage which is then sutured together can minimize consequences of the above dilemma8. Vestibular mucosa must be elevated from the undersurface of the lower lateral crura and preserved. Care must be taken in performing this technique because symmetry is crucial.
Grafting is one of the ways to create an illusion of narrowed tip and to improve definition. A preferred grafting material in the nasal tip is autologous cartilage. Septal cartilage is most commonly used because of availability and mechanical and plastic values – strength, ease of cut and sculpture. Conchal and rib cartilage are the material of choice if septal cartilage is unavailable. Irradiated rib cartilage is nonautologus alternative for the above, nonetheless surgeon should be aware of its’ higher resorbtion rate and tendency to warp. Alloplastic materials are generally avoided because of being exposed to a certain mobility of the nasal tip and related decreased tolerance for the artificial materials. Cartilage grafts in a bulbous tip can be applied as:
- tip onlay grafts, also in a multi-layer fashion if needed, to narrow the tip and improve projection,
- shield- or heart- shaped grafts to refine tip definition,
- lateral crural strut grafts, placed beneath the lateral crus, to flatten bulging cartilage.
All these grafts are ideally applied through the external rhinoplasty approach which allows for precise placement and securing with sutures. Extreme care must be taken to shape tip grafts reducing and rounding all the sharp edges that may become visible post-op9,11. This is especially true in thin skin patients.
 |  |
| A | B |
Figure 7. Tip grafts (green) placement. Tip onlay graft (A) and shield-shaped tip graft (B).
Complications
Most common complications in correction of bulbous tip are bossa formation and tip asymmetries. Some of them may happen even if surgery itself is superb and is caused by contractile healing forces. Although suture extrusion is rare, surgeon should carefully bury the knots deep in the tissues, avoiding exposure on the external cartilage surface or in the nasal vestibule. Patient satisfaction can be ruined by external nasal valve collapse which may occur with excessive resection of lateral crurae and with all adjunctive maneuvers narrowing the tip and potentially compromising airway passage. The functional aspect of narrowing bulbous nasal tip should always be carefully considered.
References:
1. Tebbetts JB. Shaping and positioning the nasal tip without structural disruption: a new, systematic approach. Plast Reconstr Surg. Jul 1994;94(1):61-77.
2. Goldman IB. Surgical tips on the nasal tip. Eye Ear Nose Throat Mon. 1954; 33: 583-591.
3. Simons RL. Vertical dome division in rhinoplasty. Otolaryngol Clin North Am. Nov 1987;20(4):785-96.
4. Davis AM, Simons RL, Rhee JS. Evaluation of the Goldman Tip Procedure in Modern-Day Rhinoplasty. Arch Facial Plast Surg. 2004; 6: 301-308.
5. Perkins S, Patel A. Endonasal Suture Techniques in Tip Rhinoplasty. Facial Plastic Surgery Clinics Of North America, 2009; 17(1): 41-54
6. Lo S, Rowe-Jones J. Suture techniques in nasal tip sculpture: current concepts. J Laryngol Otol. Aug 2007;121(8):e10
7. Adamson PA. Nasal tip surgery in open rhinoplasty. Facial Plast Surg Clin North Am. 1993;1:39-52.
8. Foda HM, Kridel RW. Lateral crural steal and lateral crural overlay: an objective evaluation. Arch Otolaryngol Head Neck Surg. 1999; 125(12): 1365-1370.
9. Sheen JH. Tip graft: a 20-year retrospective. Plast Reconstr Surg. Jan 1993;91(1):48-63
10. Burget G. Reconstruction of the Alar Cartilage Arches. Operative Technique and Plastic Surgery. 1998;5:76
11. Zijlker TD, Vuyk H. Cartilage grafts for the nasal tip. Clin Otolaryngol Allied Sci. 1993 Dec;18(6):446-58.
