ABSTRACT
Objective: To review the described surgical techniques for addressing nasal tip bulbosity and present a novel application of a previously described technique.
Study design: Review.
Surgical Methods: Cephalic resection, suture techniques, grafting techniques, techniques involving transection of the dome or lateral crura, and lateral crura repositioning techniques.
Conclusion: The surgical treatment of nasal tip bulbosity requires a thorough knowledge of complex etiology of the problem and the appropriate application specific surgical techniques.
INTRODUCTION
A nose that is considered “ideal” is one that is harmonious with the patient’s other favorable facial features. Our perception of beauty helps define what makes an ideal shape for a female or male nose. While the aesthetic quality of the face cannot be distilled to simple lines and numbers alone, the study of faces that are universally thought to be beautiful can provide guidelines or proportions that represent an aesthetic ideal. Artists have long made studies of beauty and aesthetic proportions. Similarly facial plastic surgeons have objectively studied the human face in order surgically apply this knowledge to enhance their patients’ beauty. While perhaps more appropriately called an aesthetic guideline, aesthetic ideals for nasal appearance have been thoroughly described in the facial plastic surgery literature [1-3].
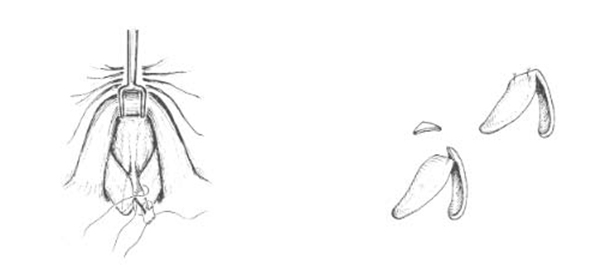
The anatomy of the “ideal” normal nasal tip has been described as having a domal arch of 4 mm, a 30 degrees divergence between intermediate crura, and roughly 5 mm between the two tip-defining points [4][Rohrich RJ. Plast Reconstr Surg 2001] (Figure 1). Toriumi has offered another way of think about the ideal tip contour. In his concept, the ideal tip has some width in the horizontal plane created by the two tip-defining points that are continuous laterally with the alar rim. This transition is smooth without any shadows along this line. The supratip area should have a slight shadow that continues into the supra-alar area [5][Toriumi DM. Facial Plast Surg Clin N Am 2009].
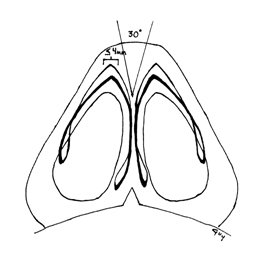
Figure 1. Base view showing the relationship of ideal nasal tip. (Rohrich RJ. Plast Reconstr Surg 2001)
In contrast, the bulbous nasal tip is wide and poorly defined. Vertical and horizontal aspects of bulbosity should be recognized when present. For example, bifidity of the nasal tip contributes to a horizontally bulbous appearance while, vertical malposition of the lower lateral cartilages (LLC) create a vertically bulbous appearance. Vertical bulbosity results in excessive supratip fullness and disrupts the brow-tip line. Although the terms boxy and bulbous are often used interchangeably, the term boxy tip is generally used to describe a tip which has a more squared appearance on the base view. Rohrich classified 3 types of boxy tip [4][Rohrich RJ. Plast Reconstr Surg 2001]: type I, with a wider intercrural angle (greater than 30 degrees); type II, with a wider domal arch (greater than 4 mm); and type III, which is a combination of both types I and II (Figure 2). One sees all of these types of deformities in the bulbous tip.
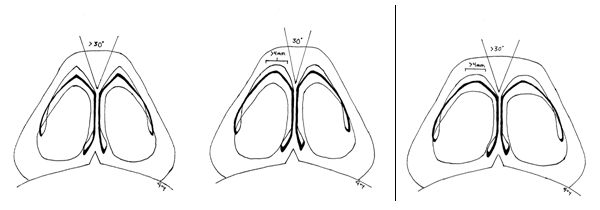
Figure 2. Three common anatomic causes of nasal tip bulbosity. A. Type I Anatomy Divergence Angle > 30degrees, domal width <4mm B. Type II Anatomy Divergence angle normal, domal width > 4mm. C. Type 3 Anatomy Divergence Angle >30 degrees, Domal width > 4mm. (Rohrich RJ. Plast Reconstr Surg 2001)
Bulbosity can be a deceptively complex and challenging deformity to correct [6][McKinney P. Ann Plast Surg 1981]. The first step to correct the bulbous tip is to make a precise identification of the anatomic origin for the deformity. The anatomic contributors to tip bulbosity include: Thick skin with excess subcutaneous fat/soft tissue, bifidity of the tip cartilages, vertical convexity of the lateral crus, horizontal convexity of the lateral crus, excessive lateral crural length, and vertical malposition of the lateral crura. The thickness of the skin plays an important role in the choice of technique. Thick skin may require more aggressive techniques to achieve the desired improvement, while in a patient with thin skin, the surgeon may favor approaches that avoid the creation of sharp edges that would be more prominent under thin skin.
Several different techniques have been described to correct the bulbous tip. The approach to thick skin and excessive subcutaneous tissue includes removal of some of this excessive subcutaneous tissue. The surgical approaches to addressing the cartilaginous contribution to tip bulbosity can be roughly divided into cephalic resection, suture techniques, grafting techniques, techniques involving transection of the dome or lateral crura, and lateral crura repositioning techniques. In this article we will review the many described techniques, with an explanation of their use depending upon the specific anatomic finding and present a novel approach which has been applied by the senior author.
SURGICAL METHODS
Cephalic resection
Most authors perform a cephalic resection of the lateral crus of the lower lateral cartilage as a first step. This will produce conservative narrowing of the nasal tip. The line of incision parallels the caudal margin of the LLC. This preserves an intact strip of cartilage from the feet of the medial crura to the most lateral part of the lateral crus. It is important in this technique to leave at least 7 mm to 10 mm of intact cartilage. The decision of how much cartilage to leave depends on the surgeon’s judgment of the strength of cartilage. If the cartilage is strong, then complete strip on the narrower end of the range may be tolerated. If a patient has weak cartilages, then a wider complete strip must be left. In some cases, the surgeon may consider avoiding cephalic resection altogether.
Cephalic resection can be undertaken via an endonasal or external rhinoplasty approach. To undertake a cephalic resection of the lower lateral cartilage, the surgeon identifies the scroll region – the cephalic border of the LLC which overlies the upper lateral cartilage (ULC). The surgeon may then excise the cephalic portion of the LLC by making an incision parallel to the caudal margin with the 15 blade or other suitable blade and then peeling off the cephalic portion, leaving the vestibular skin behind (Figure 3).

Figure 3. Caphalic resection showing the dissection of the excised cartilage off of the vestibular skin.
The senior author [D.B.] has noted that overresection of the lateral crus is perhaps the most common problem seen in his revision rhinoplasty referral practice. Overresection of the lateral crus leads to the predictable changes of alar retraction, pinching, bossae, and tip asymmetry (Figure 4). Excision of vestibular mucosa in primary rhinoplasty also may contribute to scar contracture with alar retraction.
It is important to note however, that the senior author has also found, in a significant number of revision cases, that the amount of lateral crus remaining appeared ample. It is possible that in these cases, the scar contracture caused by healing overpowered the remnant cartilage. It has become clear that if the tip cartilages are soft and weak and if the scar contracture is profound undesirable changes can occur.
In some cases, this situation can be anticipated. In an anatomic study of the alar base, Becker et al. recognized that in a normal patient population, 20% of patients had a thin alar rim [7]. This anatomic variation must be recognized, and cephalic resection should probably be avoided in these patients to minimize the risk of alar retraction or external nasal valve collapse.

Figure 4. Overresection of the nasal tip cartilages in this patient resulted in predictable, unfavorable changes. Reconstruction included bilateral alar batten grafts, a columellar strut, and a tip graft to provide some increased length. (A,B,C) Preoperative and (D,E,F) 2 year postoperative photos. Understanding that the healing forces are not completely predictable, it is important to take a conservative approach when undertaking cephalic resection. Risk cannot be eliminated but can be reduced in this manner.
Suture Techniques
The proponents of the suture techniques point out that, unlike the scoring, morselization and transection techniques, suture techniques avoid disruption of the cartilaginous integrity, leaving less room for unpredictable post-operative wound contraction forces to act and distort the nasal tip. Moreover, the suture techniques are said to be reversible [4-5].
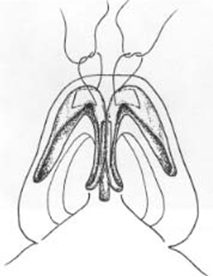
For domal sutures (Figure 5), a mattress suture of 5-0 polydioxanone suture (PDS) or other appropriate suture is passed through each dome, and the knot of each mattress suture is tied between the domes. As the sutures are secured, narrowing of the tip is accomplished. An interdomal suture sets the width between the domes. If stiff nasal-tip cartilages are en-countered, the surgeon should use 5-0 clear nylon instead of PDS [7-9].
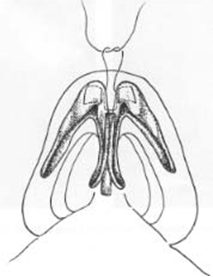
Alternatively, a single transdomal suture that traverses both domes may be placed, in lieu of two individual domal sutures and an interdomal suture (Figure 6) [4-6]. The caudal pass should be slightly longer than the cephalic pass of the mattress suture. When the mattress suture is placed in this fashion, the caudal edge will tend to lead the cephalic edge as the suture is tightened. This creates a more favorable tip-supratip relation. If the cephalic edge leads the caudal edge of the lateral crus despite proper placement of the domal suture, a small cephalic wedge of the cartilage may be excised and the edges sutured, which reposi tions the cephalic edge lower in relation to the caudal edge (Figure 7).
In addition to narrowing the domal angle, the suture techniques effectively address a wide inter-crural distance. Specifically, the interdomal component brings the two domes together and narrows the inerdomal distance. Tardy [8][Tardy ME Jr. Facial Plast Surg 1993] has described the importance of recognizing a common triad of “thin skin, strong cartilage, and bifidity,”, the treatment of which is suture techniques that include an interdomal component (ie a “dome binding suture.”)
 |  |
 | |
| Figure 5. Individual horizontal mattress domal sutures. The caudal pass is slightly longer than the cephalic pass of the mattress suture. As the sutures are secured, narrowing of the tip is accomplished. An interdomal suture is placed between the two domes, securing the interdomal distance.. |
 |
| Figure 6. A single transdomal suture may be placed in lieu of two individual domal sutures and an interdomal suture.. |
Nasal tip suture techniques have evolved over time with multiple authors contributing their own refinements addressing various deformities including tip bulbosity. Papel [9][Papel ID. Arch Facial Plast Surg 2005] has described his suture technique for dome sutures and an interdomal suture. Becker [10][Corrado A. Arch Facial Plast Surg 2009] has described a “dome stabilitzation suture” to help maintain stability and symmetry of the nasal tip complex. Gruber [11][Gruber RP. Plast Reconstr Surg 2002] has proposed a step-wise suture algorithm. Following cephalic resection, transdomal and interdomal sutures are placed, a lateral crura mattress suture and a columella-septal suture are then placed to create tip contour and address bulbosity. Rohrich [4][Rohrich RJ. Plast Reconstr Surg 2001] also employs a suture algorithm based on the anatomy of the LLC in relation to the angle of divergence between crura, the domal arc and skin thickness. Tebbetts [12][Tebbetts JB. Plast Reconstr Surg 1994] proposes the use of lateral crura spanning sutures, which can reduce the crural convexity and the angle of divergence with an increase in tip projection. Daniel [13,14][Daniel RK. Plast Reconstr Surg 1999] described the use of the ‘three-stitch’ technique, which he states allows the surgeon to avoid the need to transect the alar rim.
Grafting Techniques
Gunter and Friedman [15][Gunter JP. Plast Reconstr Surg 1997] have described a lateral crural strut graft to address a bulbous tip. In this technique, a pocket is dissected between the lateral crus and the vestibular mucosa. Following a cephalic trim, the vestibular skin is dissected from the LLC in a cranial to caudal direction, preserving the attachment on the caudal border of the cartilage. A cartilage graft is placed in this pocket between the lateral crus and the vestibular mucosa. It is fashioned from the nasal septum most commonly or from auricular concha or rib cartilage. When appropriately positioned, it is then sutured to the lateral crus and acts as a “splinting graft”, flattening the convex lateral crus cartilage, which is weaker than the graft. The lateral end of the graft can be at the level of or over the pyriform aperture, depending on whether or not correction of an external nasal valve insufficiency is desired. In the treatment of nasal tip bulbosity, this graft can be a solution to decrease the lateral crura convexity, especially after dome sutures, and to reposition a vertically oriented crus.
McKinney [16-17][McKinney P. Plast Reconstr Surg 2000] described a stepwise approach to the bulbous tip. He advocates cephalic resection and transdomal sutures as a first measure for reducing bulbosity, followed by the insertion of lateral crura strut graft to straighten this segment if necessary. When those maneuvers fail to adequately correct the deformity he employs a technique detailed in the following section, involving vertical transection of the lateral crura [16-17][McKinney P. Ann Plast Surg 1983].
Morselization and Cartilage Cutting Techniques
McCollough [18][McCollough EG. Arch Otolaryngol 1985] describes the use of cartilage morselization in addition to suture techniques to decrease the tension in the cartilage and provide a more acute angle between the crura, thereby decreasing tip bulbosity. If greater acuity is desired that achieved using morselization then vertical dome division can be employed.
Complications that have been attributed in the literature to dome division include bossae formation and other tip abnormalities. However, Simons et al have described the routine use of dome division in tip rhinoplasty in over 1000 patients and reports no greater incidence of complications with long term followup in his hands compared to the complication rate of other techniques as described in the literature.[19] The senior author often divides the lateral crura in the treatment of tip bulbosity (see below) but divides the domes infrequently, and most commonly in the thick- skinned patient. When dividing the domes, the senior author always preserves the vestibular skin and always suture reconstitutes the divided cartilage with interrupted sutures. The placement of sutures to reapproximate the divided cartilages after dome division secures the position of the cartilage and preserves tip stability. Simple interrupted sutures are preferred to a mattress suture, because a mattress suture may excessively narrow the tip (Figure 8).
 |
| Figure 7. Excising a small cephalic wedge of cartilage from the dome can help reposition the cephalic margin lower in relation to the caudal edge. |
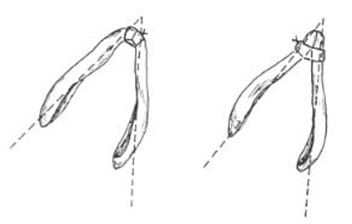
Figure 8. Divide the dome by vertical incision. Reapproximate the divided cartilages with suture (e.g., 6-0 PDS) to secure the position of the cartilage and reconstitute the intact strip.Suture reapproximation of divided lower lateral cartilages is undertaken with simple interrupted stitches. Mattress stitches in this situation may result in overnarrowing as illustrated in the second diagram.
In McKinney’s stepwise approach, when cephalic resection, suture techniques, and a strut graft fail to satisfactorily address bulbosity, a complete vertical transection of the lateral crura is undertaken 2 to 3 mm laterally to the dome [16-17][McKinney P. Ann Plast Surg 1983]. This is a modification of the technique described by Goldman [20][Goldman IB. Arch Otolaryngol 1957], where the LLC is divided just laterally to the domes and subsequently sutured to approximate the crura. The Goldman technique has been reported to have a higher risk of creating pinching and single tip-defining point or “unitip.”
Techniques Addressing Vertical Malposition
Frequently the lateral crura of the LLC will present in a more vertical position contributing to vertical bulbosity and supratip fullness. In this situation the above described techniques will not fully address the problem. For those cases, Sheen [3][Sheen JH. AestheticRhinoplasty 2nd Ed 1987] and Hamra [21][Hamra ST. Plast Reconstr Surg 1993] each have described techniques for repositioning the lateral crura into a more horizontal position. Sheen describes making an incision along the vestibular skin and rotating the cartilage-skin complex into a more caudal position on the ala, while Hamra dissects the cartilage free from skin and reposition it into a pocket created on the ala.
Lateral Crural Division and Overlay
The lateral crural overlay technique has been well described for the patient whose anatomy calls for rotation and deprojection, (Figure 9) (22). In this technique, the lateral crura are incised lateral to the domes. The vestibular mucosa is elevated from the undersurface of the lateral crus, and the medial por tion is overlapped over the lateral and secured in place with sutures. When undertaking this maneuver, great care must be taken to perform it symmetrically.
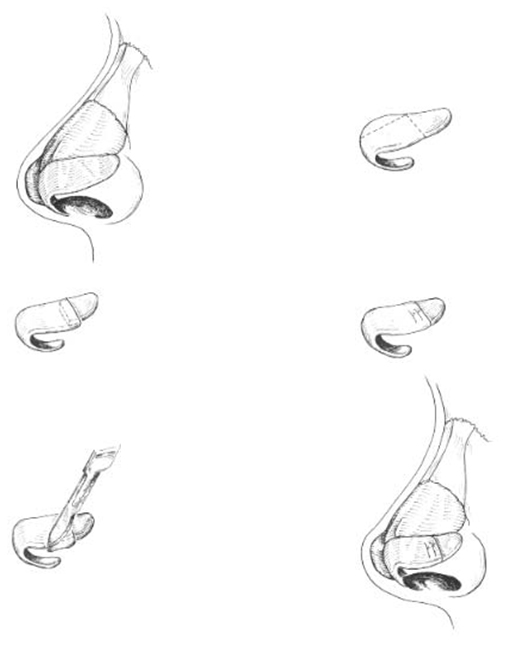
Figure 9. The lateral crural overlay techniques as described to effect tip projection and rotation.
The senior author has found the lateral crural overlay technique to be a useful tool in specifically treating tip bulbosity. He has found in his revision rhinoplasty practice that excessive horizontal length of the lateral crura is an often overlooked anatomic cause of tip bulbosity. If the horizontal excess is relatively minor, suture techniques and strut graft techniques may be effective in flattening the lateral crus, but for more substantial cases these methods will fail. In these situations, the lateral crura must be shortened. The concept might be likened to a 12 inch piece of rubber in a 10 inch space. The rubber will bend, forming a convexity. One clear solution would be to cut and overlap the rubber by 2 inches, creating a flat appearance (ie reducing the bulbosity).
In this approach, the lateral crura are divided at the point of greatest convexity after the vestibular mucosa has been dissected (Figure 10(A)). They are then overlapped and suture secured with 3 interrupted sutures, a cephalic, a caudal and a central suture (Figure 10(B)). Any further reduction would cause a pull or lift producing rotation, as in the traditionally described lateral crural overlay technique. However, if the overlay is done to the point of reducing the convexity only, then no rotation will occur.
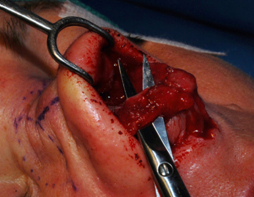

A. B.
Figure 10. Intraoperative photos showing the lateral crural overlay technique. (A) The lateral crus is dissected and transected at the point of greatest convexity. (B) The caudal end is then overlapped on the cephalic end and sutured into place.


A. B.


C. D.










Figure 11. Three patients with nasal tip bulbosity who underwent rhinoplasty including lateral crural overlay. (A,B) Pre op. (C,D) Post op. With the lateral crural overlay, tip bulbosity can be addressed with or without rotation of the nasal tip.
One could alternatively excise a piece of the lateral crural cartilage and suture-reapproximate the edges. However, the senior author has found that the overlapping cartilage appears to provide increased strength (akin to the strength of ply-wood) and has not to date negatively affected the surgical result.
As noted, this concept is not new. A similar technique, with transection of the lateral crura, was described by Kridel [22][Kridel RWH. Arch Otolaryngol Head Neck Surg 1991]. This technique, however, was intended to correct tip ptosis but could also be adapted to reduce tip bulbosity and de-project the nasal tip through removal of a segment of the lateral crura. Its strongest indication is for a tip that is bulbous in appearance, poorly projected and underrotated. Boccieri [23][Boccieri A. Arch Facial Plastic Surg 2008] modified Kridel’s technique to improve tip bulbosity with a stair-step incision in the lateral crura rather than a linear one. This modification allows a more controlled way to reorient the lateral crura to a more horizontal position. Another variation of this technique is a z-plasty of the lateral crura [24][Oktem F. J Plast Reconstr Aesthet Surg 2010]. In this approach, instead of a stair-step incision, an oblique incision at 45° from superior to inferior and anterior to posterior is made. The cartilage is then re-approximated with the superior edge of the anterior segment being secured to the inferior edge of the posterior segment, effectively repositioning the lateral crura to a more horizontal orientation. Some authors expressed concern with transection of the lateral crura and potential problems from this maneuver, specifically visible irregularities, alar pintching and collapse. Peck [25][Peck G. Clin Plast Surg 1977] and Chait [26][Br J Plast Surg 1991] remove the posterior portion of the lateral crura, and subsequently, reposition the remaining cartilage to occupy the posterior space created by the resection. This effectively reduces the angle between medial and lateral crura, and therefore, the tip bulbosity.
Additionally the lateral crura overlay technique effectively flattens the convexity and can mitigate the need for lateral crural repositioning in many cases of vertical malposition. In this situation, small batten grafts are also placed to address the absence of lateral crus more inferiorly. This is felt to be important in the operated nose to provide strength against the healing forces, and thereby avoid alar retraction.
Conclusion
Nasal tip bulbosity is one of the more complex problems to address in aesthetic nasal surgery. The multitude of surgical techniques which have been described to address this problem reflects its complexity and varied etiology. In general, none of the techniques presented above can be universally applied to every nose with a bulbous tip. Consequently facial plastic surgeon must be prepared to employ various techniques based on the anatomic deformity. We present here the concept of excessive horizontal length of the lateral crura and specifically applying the lateral crural overlay technique to provide the surgeon another tool in achieving the “ideal” nose.
References
- Farkas LG, Hreczko TA, Kolar JC, Munro IR. Vertical and horizontal proportions of the face in young adult North American Caucasians: revision of neoclassical canons. Plast Reconstr Surg. 1985;75(3):328-38.
- Powell N, Humphreys B. Proportions of the Aesthetic face. New York: Thieme-Stratton, 1984.
- Sheen, JH. Aesthetic Rhinoplasty. St. Louis: Mosby, 1987;432-62
- Rohrich RJ, Adams WP. The boxy nasal tip: classification and management based on alar cartilage suturing techniques. Plast Reconstr Surg. 2001;107(7):1849-63.
- Toriumi DM, Checcone MA. New concepts in nasal tip contouring. Facial Plast Surg Clin N Am. 2009;17(1):55-90.
- McKinney P, Cook JQ. A critical evaluation of 200 rhinoplasties. Ann Plast Surg. 1981;7(5):357-61.
- Becker DG, Weinberger MS, Greene BA, Tardy ME. Clinical study of alar anatomy and surgery of the alar base. Arch Otolaryngol Head Neck Surg. 1997;123(8):789-95.
- Tardy ME, Walter MA, Pratt BS. The overprojecting nose: anatomic component analysis and repair. Facial Plast Surg. 1993;9(4):306-16.
- Papel ID. Interlocking transdomal suture technique for the wide interdomal space in rhinoplasty. Arch Facial Plast Surg. 2005;7(6):414-7.
- Corrado A, Bloom JD, Becker DG. Domal stabilization suture in tip rhinoplasty. Arch Facial Plast Surg. 2009;11(3):194-7.
- Gruber RP, Friedman GD. Suture algorithm for the broad or bulbous nasal tip. Plast Reconstr Surg. 2002;110(7):1752-64.
- Tebbetts JB. Shaping and positioning the nasal tip without structural disruption: a new, systematic approach. Plast Reconstr Surg. 1994;94(1):61-77.
- Daniel RK. Rhinoplasty: a simplified, three-stich, open tip suture technique. Part I: primary rhinoplasty. Plast Reconstr Surg. 1999;103(5):1491-502.
- Daniel RK. Rhinoplasty: a simplified, three-stich, open tip suture technique. Part II: secondary rhinoplasty. Plast Reconstr Surg. 1999;103(5):1503-12.
- Gunter JP, Friedman RM. Lateral crural strut graft: technique and clinical applications in rhinoplasty. Plast Reconstr Surg. 1997;99(4):953-5.
- McKinney P. Management of the bulbous nose. Plast Reconstr Surg. 2000;106(4):906-17.
- McKinney P, Stalnecker M. Surgery for the bulbous nasal tip. Ann Plast Surg. 1983;11(2):106-13.
- McCollough EG, English JL. A new twist in nasal tip surgery. An alternative to the Goldman tip for the wide or bulbous lobule. Arch Otolaryngol. 1985;111(8):524-9.
- Simons RL. Vertical dome division in rhinoplasty. Otolaryngol Clin North Am. 1987;20(4):785-96.
- Goldman IB. The importance of the mesial crura in nasal-tip reconstruction. AMA Arch Otolaryngol. 1957;65(2):143-7.
- Hamra ST. Repositioning the lateral alar crus. Plast Reconstr Surg. 1993;92:1244.
- Kridel RW, Konior RJ. Controlled nasal tip rotation via the lateral crural overlay technique. Arch Otolaryngol Head Neck Surg. 1991;117(4):411-5.
- Boccieri A, Raimondi G. The lateral crural stairstep technique: a modification of the Kridel lateral crural overlay technique. Arch Facial Plast Surg. 2008;10(1):56-64.
- Fatih O, Ali TT, Gulsum TM. Cartilage Z plasty on lateral crus for treatment of alar cartilage malposition. J Plast Reconstr Aesthet Surg. 2010;63(5):801-8.
- Peck G. The difficult nasal tip. Clin Plast Surg. 1977;4(1):103-10.
- Chait L. A new approach for the refinement of the very broad nasal tip. Br J Plast Surg. 1991;44(8):572-4.
