No funding support and authors have nothing to disclose
Abstract
Spreader grafts are harvested pieces of cartilage placed between the upper lateral cartilage and dorsal septum. In functional nasal valve surgery or cosmetic rhinoplasty placement of these grafts can be accomplished in an endonasal submucosal pocket created between the dorsal septum and the upper lateral cartilage. This approach can allow for improvement in the internal nasal valve, aesthetic middle vault refinements, and prevention of inverted-v deformity. Although technically challenging, the endonasal approach can avoid the increased operative time and recovery associated with the open approach for spreader graft placement.
1. Introduction:
Nasal spreader grafts were described by Sheen in 1984 to widen a collapsed or narrowed internal nasal valve. This improves nasal airflow by lateralizing the lateral nasal wall from the septum and widens the middle vault. The internal nasal valve has been described as the most problematic area for decreased nasal patency 1,2. Since the original publication, spreader grafts have become widely adopted in the treatment of the internal nasal valve. Additionally, the culture and paradigm of rhinoplasty has changed from an essentially reductive approach to an augmentation-focused approach with increased use of grafting. Patient preference for less downtime, decreased invasiveness and scarring has helped to drive a recent shift toward more endonasal rhinoplasty procedures. In 2005, Pontius and Williams published an article describing the placement of spreader grafts through an endonasal approach3. The advantages of an endonasal rhinoplasty were described, including avoidance of an external scar, less retraction of the skin and soft tissue envelope, and potential for decreased operative time. In addition, endonasal rhinoplasty can be a useful adjunct to a functional breathing operation.
2. Use of spreader grafts in open septorhinoplasty
While not the focus of this chapter, open septorhinoplasty affords the surgeon clear exposure and facilitates secure placement of the spreader grafts with sutures. However, this comes at the cost of separating the upper lateral cartilages. Spreader grafts may be useful in cosmetic septorhinoplasty to address inverted-v deformities or significant convex deformities of the middle third of the nose.
3. Use of spreader grafts in endonasal septorhinoplasty
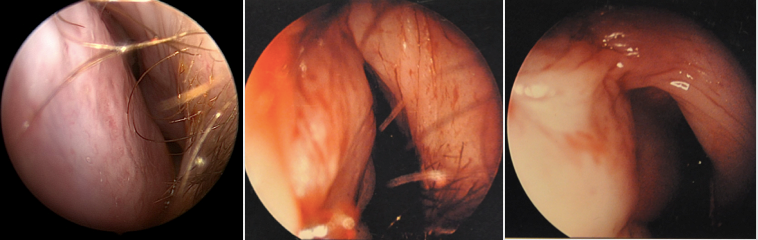
A recent prospective study objectively measured improvement in the internal nasal valve after endonasal spreader graft placement in combination with septoplasty and turbinate reduction. The study used dynamic video nasal endoscopy, acoustic rhinometry, and the subjective NOSE questionnaire to assess outcomes4. The authors found significant improvements in nasal valve patency grades.



4. Techniques
As described, we typically perform the placement of spreader grafts coupled with complementary functional nasal procedures, including a septoplasty and bilateral inferior turbinate reduction, which is performed in a stepwise fashion (Figure 2).
When anatomy permits, the use of autologous septal cartilage is the author’s preferred grafting material, though in revision cases conchal or rarely costal cartilage can be used. In our practice, use of harvested septal bone has been attempted, but does not slide into the pockets well and should be avoided.
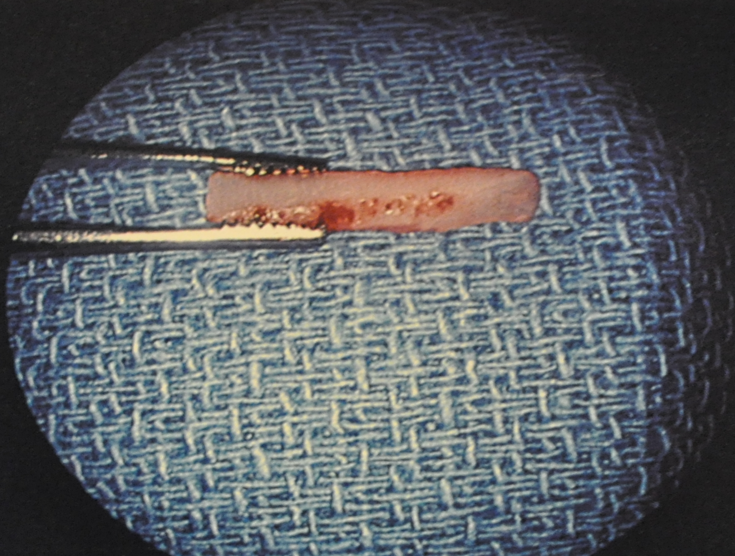
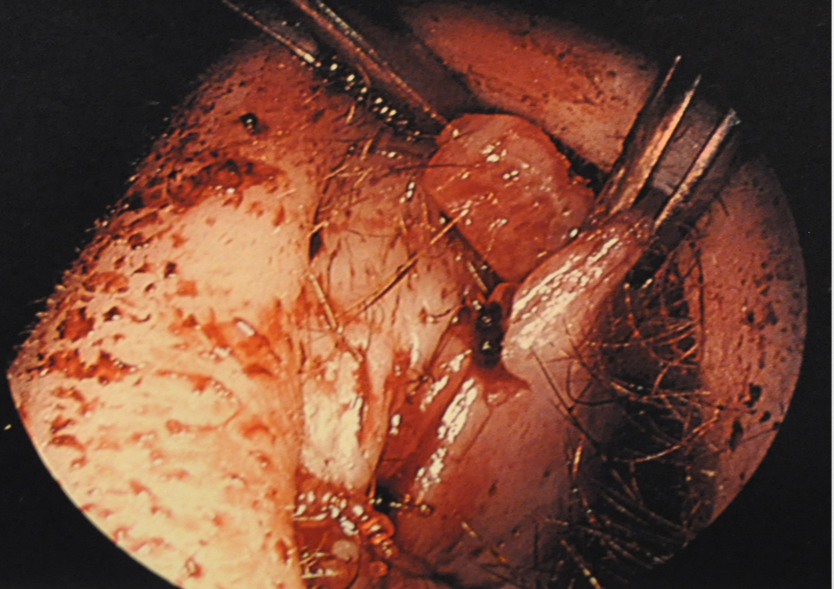
The grafts are harvested via a standard septoplasty approach, leaving an adequate L-strut along the dorsum and caudal septum. Once a reasonable amount of cartilage is harvested, the grafts can be shaped. The size and width of the grafts varies based on the length of the nasal bones and upper lateral cartilages. In general, the preferred thickness is about 2mm – 3mm and the length is generally about 1.5cm – 2cm, with the cephalic end tapered to facilitate easier insertion. (Figure 3). A Woodson elevator used to dissect our pocket, without separation of the upper lateral cartilages (ULC), and it is crucial to feel the end of the instrument contacting the dorsal septum until the keystone area is reached (Video 1). It should be noted that some surgeons do advocate for separation of the ULC as it permits lateralization and prevents inherent recoil of the ULC5. It is imperative to keep a pocket separate from the larger flap from which the donor site is harvested. If a convexity in the harvested cartilage exists, this is preferred if one side has a concave-appearing middle vault. We have found that if a pocket is appropriately snug for the graft, no further sutures are often needed (Figure 4). If the graft appears to sag somewhat, we have placed through-and-through mattressing plain gut sutures just inferior to the grafts. Some groups have advocated the use of 2-Cyanobutylacrylate Glue or a transcutaneous suture to facilitate fixation or a suture attaching the two grafts ex-vivo, with the sutures laid over the dorsal septum.6-7
5. Complications
Inherent in any rhinoplasty operation are established risks and the potential need for revision. Specific to spreader grafts in the senior author’s experience, there may be some visible nasal widening that occurs with spreader graft placement, endonasal or open. Because the grafts are essentially placed blindly into a mucoperichondrial pocket, there is also the risk of malposition. The pocket must be just snug enough to accommodate the graft, without gaping, which would permit graft migration into the nasal airway, thus potentially worsening the patient’s breathing. Often during the learning phase of this operation, the pocket will get extended just a few millimeters, which is enough to separate the mucosal attachments and let the graft inferiorly migrate. Furthermore, surgeons must be careful not to over elevate the mucoperichondrial flap during the septoplasty portion of the procedure, so as to keep the pockets for spreader graft placement separate. Like any cartilage grafting procedure, there is the risk of cartilage resorption over time, though historically less with autogenous grafts8.
6. Conclusion
We feel that with experience, the addition of endonasal spreader grafts can lead to an impressive benefit to nasal patency and to address functional airway narrowing. When coupled with routine functional nasal procedures, such as bilateral inferior turbinate reduction and septoplasty, it adds very little risk in terms of additional operative time or reductive maneuvers and repurposes harvested cartilage. Furthermore, even in a cosmetic setting, we believe this is a technique that improves nasal breathing and will address asymmetries in the mid-vault after a hump removal to prevent an inverted-v deformity.
References:
- Sheen JH. Spreader graft: A method of reconstructing the roof of the middle nasal vault following rhinoplasty. Plast Reconstr Surg. 1984 Feb;73(2):230-9.
- Constantian MB, Clardy RB. The relative importance of septal and nasal valvular surgery in correcting airway obstruction in primary and secondary rhinoplasty. Plast Reconstr Surg. 1996 Jul;98(1):38,54; discussion 55-8.
- Pontius AT, Williams EF,3rd. Endonasal placement of spreader grafts in rhinoplasty. Ear Nose Throat J. 2005 Mar;84(3):135-6.
- Erickson B, Hurowitz R, Cote DW et al. Acoustic rhinometry and video endoscopic scoring to evaluate postoperative outcomes in endonasal spreader graft surgery with septoplasty and turbinoplasty for nasal valve collapse. J Otolaryngol Head Neck Surg. 2016 Jan 12;45:2,016-0115-9.
- Yoo DB, Jen A. Endonasal placement of spreader grafts: Experience in 41 consecutive patients. Arch Facial Plast Surg. 2012 Sep-Oct;14(5):318-22.
- Andre RF, Paun SH, Vuyk HD. Endonasal spreader graft placement as treatment for internal nasal valve insufficiency: No need to divide the upper lateral cartilages from the septum. Arch Facial Plast Surg. 2004 Jan-Feb;6(1):36-40.
- Manavbasi I, Agaoglu G. Endonasal placement of spreader grafts. Plast Reconstr Surg. 2007 May; 119(6): 1961-1962.
- Staffel G, Shockley W. Nasal implants. Otolaryngol Clin North Am. 1995 Apr;28(2):295-308.
