When a patient requesting rhinoplasty also complains of nasal obstruction, it is critical to accurately diagnose the cause. The author reviews diagnostic procedures, including anterior rhinoscopy, nasal endoscopy, and coronal-sinus computed tomography scan. He discusses technical aspects of septoplasty and turbinate surgery, which address common causes of nasal obstruction, emphasizing traditional and endoscopic septoplasty, septoplasty techniques to address the caudal septum, and a graduated stepwise approach to the inferior turbinates. (Aesthetic Surg J 2003;23:393-403.)
It is not unusual to see patients with concerns about both nasal appearance and function. Therefore the surgeon must have intimate knowledge of both external and intranasal anatomy. The differential diagnosis of conditions causing nasal obstruction is extensive (Table 1). Although patients with these conditions are frequently seen in practices that specialize in nasal function, some also present for treatment in rhinoplasty practices. It is critical that nasal obstruction be correctly diagnosed. Just as aesthetic analysis leads to an appropriate rhinoplasty plan, good functional nasal analysis dictates appropriate medical or surgical treatment.
In my practice, problems causing nasal obstruction in patients seeking rhinoplasty have included deviated septum, chronic sinusitis, sinus polyps, antrochoanal polyp, rhinitis medicamentosa, turbinate hypertrophy, adenoid hypertrophy, tumor (rhinoplasty was deferred in this patient), concha bullosa, choanal stenosis, and internal and external valve collapse.
Diagnosis of Nasal Obstruction
A detailed history is critical in evaluating and treating patients presenting with nasal complaints or requesting nasal surgery. In the history, consider nasal obstruction, chronic or recurrent sinusitis, postnasal drip and cough, facial pressure or pain, ear pressure or pain, hearing loss, loss of sense of smell or taste, halitosis, and other pertinent findings (Table 2). Be sure to ask about environmental allergies and to further evaluate these when appropriate.4 A history of topical nasal-decongestant abuse may cause rhinitis medicamentosa. Note whether there is a history of sinus surgery, rhinoplasty, or other nasal surgery.
Perform anterior rhinoscopy before and after topicalization with a vasoconstricting agent. You may not detect any abnormalities on anterior rhinoscopy, or an anatomic abnormality may be observed but not fully appreciated. Perform a nasal endoscopic examination when indicated by patient history or by anterior rhinoscopy findings.
Abnormalities and physical findings not apparent on rhinoscopy may appear when careful endoscopy is per-formed by a skilled endoscopist.
With the extensive differential diagnosis of nasal obstruction in mind, I will focus here on technical aspects of 2 commonly performed surgical procedures to address nasal obstruction: septoplasty and turbinate surgery.
Technical Considerations in Septoplasty
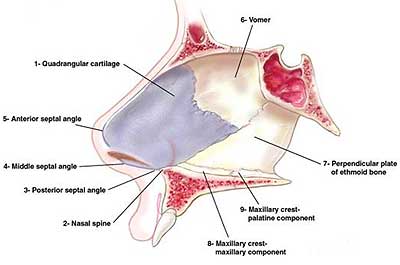
The anatomy of the septum is well recognized by nasal surgeons (Figure 1).8-11 In this section, we will consider traditional septoplasty, endoscopic septoplasty, and septoplasty techniques to address the caudal septum. I prefer the traditional septoplasty approach (as opposed to endoscopic septoplasty) for broad deviations and for primary septoplasty. Endoscopic approaches are less invasive and advantageous for focal deflections and spurs, as well as for revision septoplasty. Caudal septal deflections require special attention.
To perform a traditional septoplasty, I retract the columella with a small nasal speculum, but a columellar retractor, large 2-prong hook, or other suitable instrument may also be used. The purpose is to expose the caudal margin of the septum and to protect the columella from injury. Next I make a hemitransfixion incision extending from the anterior septal angle to the posterior septal angle along the caudal border of the cartilaginous septum with a 15 blade or 15-C blade. I use a modified Killian incision if less exposure is necessary. However, if I need access to the caudal septum or need to separate the upper lateral cartilages from the dorsal septum to place spreader grafts, or if I simply feel that I require the widest possible exposure, I will use a hemitransfixion incision.
Differential diagnosis of nasal obstruction
Table 1. Differential diagnosis of nasal obstruction
| Cause | Example |
| Allergic | Allergic rhinitis |
| Congenital | Encephalocele (iatrogenic or posttraumatic), glioma, teratoma |
| Chronic rhinosinusitis | |
| Endocrine | Pregnancy, hypothyroidism, adrenal insufficiency, menstruation |
| Iatrogenic | Atrophic rhinitis, overresection, overnarrowing after osteotomies |
| Infection | Acute and chronic rhinosinusitis, septal abscess |
| Inflammatory polyposis | |
| Mechanical | Deviated septum, nasal valve collapse, synechiae, nasal polyps, inferior turbinate hypertrophy, middle turbinate hypertrophy (including concha bullosa), adenoid hypertrophy, choanal atresia, septal hematoma |
| Medicinal | Rhinitis medicamentosa |
| Neoplastic | Benign and malignant nasal tumors |
| Foreign body | |
| Nasal cycle | |
| Other |