Introduction
While septoplasty is a commonly performed operation in adults, its use in children is less frequent and controversial. Pediatric Septoplasty is also performed by a pediatric ENT specialist with unique training and equipped to handle an array of issues that arise when treating babies, children, and teens. Pediatric septoplasty was described as early as 1902.1 However, results were less than promising with many children developing deformities such as a saddle nose deformity and maxillary retrusion post-operatively.2 In the 1950s, surgeons warned against performing septoplasty in the pediatric population as resection of the quadrilateral cartilage was thought to negatively affect the growth of the nose.3 They felt that the quadrangular cartilage was the keystone in the development of the cartilaginous vault and therefore should not be disrupted. This theory was further supported by Farrior and Connolly in the 1970s, who believed that nasal surgery should be delayed until growth of the nose was complete.4 However, it was also in this same decade that pediatric septoplasty started to be more widely performed. This sparked a variety of animal and clinical studies to evaluate outcomes after performing surgery on the growing nose. Over time pediatric septoplasty has evolved based on clinical evidence. This chapter will outline the history, indications, and technique of pediatric septoplasty.
Animal and Human Studies
One of the first studies performed that evaluated the effect of septoplasty on the growing nose was done by Sarnat. In this study, large sections of cartilage were resected in young rabbits without preservation of the mucoperichondrium. As a result, these rabbits were noted to have underdevelopment of their maxilla and saddling of the nasal dorsum as they matured. In contrast, when this resection was performed on adult rabbits, the same underdevelopment was not seen, indicating that the changes in nasal appearance were not due to lack of support from the missing cartilage, but rather changes in growth patterns. This supported the idea that the septovomeral region was a critical growth center for development and its resection could drastically affect the growth potential of the nose and other adjacent structures.5 However, a criticism of this paper is that the mucoperichondrium was not preserved and that through-and-through resections were performed. Therefore, to evaluate the implication of preservation versus resection of the mucoperichondrium with the septal cartilage, additional studies were performed. Hartshorn et al. found poor midface growth after resection of septal cartilage and mucoperichondrium.6 However, when Bernstein et al. performed the same septal cartilage resection with preservation of the mucoperichondrium, there did not appear to be any growth disturbance of the midface.7 This provided evidence supporting the importance of mucoperichondrium preservation and its role in growth potential of the developing nose.
Cupero et al. used cephalometric analysis to objectively analyze how septoplasty could affect the growing nose in ferrets. Nine week old ferrets were divided into three treatment groups; the first with bilateral mucoperichondrial flaps raised, a second with bilateral mucoperichondrial flaps and partial septal cartilage excision, and a third with bilateral mucoperichondrial flaps and excision of a portion of the vomer. Cephalometric analysis showed that there was no difference in the growth of the nose between the three groups. This led the authors to believe that functional septoplasty would not lead to disturbance in facial growth.8
Beginning in the 1990s, human studies were performed to validate the results seen in these animal models, confirming the lack of impact of septoplasty on craniofacial growth. Jugo and Triglia et al. were two of the first to provide evidence and advocate for performing pediatric external septoplasty when indicated without adverse subjective anthropometric effects.9,10 Later, a more objective anthropometric analysis using 12 specific anatomic landmarks to analyze outcomes was performed. Twenty eight children were evaluated with average follow up time of 3.4 years. While nasal dorsal length appeared to be shortened in those patients who had undergone septoplasty, other facial and nasal measurements showed similar metrics to normal averages.11 El-Hakim et al. also performed anthropometric analysis on 26 pediatric patients after septoplasty using an external approach with similar average follow up time of 3.1 years. This study also found a decreased nasal dorsum length and tip protrusion, however these values were not statistically significant.12 An additional anthropometric study was then performed, evaluating the long term effects of external septoplasty with findings showing no effect on the growth of the nasal or facial skeleton.13
The endonasal technique for pediatric septoplasty was not evaluated until 2011 when Tasca et al. performed a retrospective review of 44 patients with an average follow up time of 12.2 years. This study not only evaluated the endonasal approach, but also allowed for anthropometric analysis after long term follow up. Based on these results, it was found that there was a reduced nasolabial angle compared with controls for patients who underwent external septoplasty. However, nasolabial values were similar to controls for patients who underwent endonasal septoplasty. Additionally, nasal dorsum length was found to be reduced in female patients when compared to controls, but not reduced for male patients.14
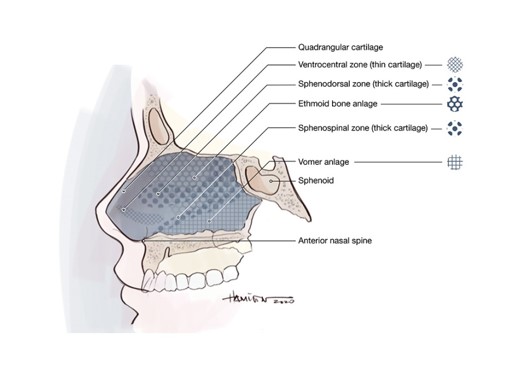
In summary, animal research has been helpful to elucidate that the septum and mucoperichonrdium are important for the development of the bony nasal skeleton. There are specific growth zones of the cartilaginous septum that contribute to the nasal dorsum form and midface lengthening.
The Changing Anatomy of the Nasal Skeleton
During development, the dimensions and composition of the nasal skeleton and septum will change. The external characteristics of a pediatric nose are summarized by a larger nasolabial angle and shorter nasal dorsum with less projection.15 Additionally, a pediatric nasal tip is often more flat with a short columella and round nares15. The septum itself will have a higher cartilage to bone ratio. At birth, the septal cartilage extends from the sphenoid bone at the skull base to the columella and nasal tip. Progressive ossification occurs at the cartilaginous septum and the perpendicular plate expands in a caudoventral direction. After expansion of the perpendicular plate, the septal cartilage is separated from the sphenoid and is firmly connected to the premaxilla by the spinoseptal ligament (decussating fibers). The cartilaginous dimensions of the septum reach a maximum at 2 years of age. Growth past this point is due to growth of the perpendicular plate by continued ossification of septal cartilage at the septoethmoidal junction. Loss of cartilage by ossification is balanced by the formation of new cartilage through mitotic activity and expansion of the intracellular matrix.16
Other differences between pediatric and adult noses are that the upper lateral cartilages extend under the length of the nasal bones in children, while they only extend 3 to 5 mm under the nasal bones in adults. This change occurs due to regression of the upper lateral cartilages as the child grows. Additionally, many of the normal bony structures in adults are underdeveloped in pediatric patients, including the vomer. Around age 6 to 8 years old, the perpendicular plate and vomer will be fully developed and merge.15
It is thought that there are two periods of significant nasal growth. The first is during the first two years of life, as previously described. The second period occurs during puberty and ends between ages 12 to 16 years for girls and 15 to 18 years for boys.15 Therefore, elective surgery was historically delayed until age 14 for girls and 17 for boys, allowing for complete development of the nose prior to surgery. The two growth centers of the nose have been identified as the sphenodorsal zone, between the sphenoid and dorsum, and sphenospinal zone, between the sphenoid and anterior nasal spine. The sphenodorsal zone will increase length and height of the nasal bones while the sphenospinal angle is responsible for forward growth of the maxilla.17 Grymer et al. performed an observational study of a pair of monozygotic twins in which these two zones and their effect on nasal development were evaluated. Trauma to these growth zones led to growth inhibition in one twin, with subsequent development of nasal deformities including upward displacement of the anterior maxilla, diminished vertical height of the nasal cavity, and a retrognathic maxilla secondary to decreased anteroposterior maxillary growth.2
Timing
There is currently no general consensus based on published data as to the minimum age at which performing a septoplasty would be reasonable. However, septal deviation can be present as early as birth. The act of passing through the birth canal can be traumatic and lead to nasoseptal deformity. There is an approximate septal deformation rate of 22% in children born by spontaneous birth vs. 3.9% in those born by cesarean section.18 If left untreated, nasoseptal deformity in these patients can lead to respiratory distress, due to their preferential nasal breathing, and failure to thrive. Despite the fact that septal deviation can present at a very young age, many authors advocate waiting until the age of 5 or 6 years old before performing surgical intervention for nasal obstruction. If other indications for septoplasty are present, then the operation may be necessary at ages younger than five years age. Closed reduction is advocated as the method of treatment for nasal septal deviation in the neonatal period. This includes digital compression on the dorsum for 10 to 15 minutes or the use intranasal instrumentation. Elective nasal surgery should be delayed until completion of nasal development.
Indications
While delaying septoplasty until after completion of nasal development is the generally accepted recommendation, there are several indications for performing the surgery prior to this. Table 1 outlines the absolute and relative indications for performing pediatric septoplasty. Absolute indications for performing pediatric septoplasty include septal abscess with cartilage destruction, severe nasal deformity secondary to acute nasal fracture, nasoseptal deformity secondary to a cleft, nasal malignancy, and severe nasal obstruction resulting in sleep apnea.15,19 These indications are widely accepted due to the potential for progressive functional deficits, anatomic deformity, and psychosocial effects of delaying repair. Severe uncorrected deformities have been shown to lead to malocclusion, palatal asymmetry, and other various deformities of the midface and dental anatomy.
With regard to septal abscess, initial management involves incision and drainage as well as antibiotics. However, septoplasty does play a role in reconstruction of infected or necrotic cartilage. By performing immediate reconstruction of the cartilage, correcting the deformity early, one is able to prevent long term adverse effects on the growth of the midface. Alshaikh et al. evaluated the role of septoplasty in cartilage reconstruction after nasal septal abscess by reviewing results from 81 articles, finding that early reconstruction resulted in normal nasal development and function.20
Nasal airway obstruction is a relative indication for performing septoplasty, and the most common indication for performing the procedure in children. While many studies have shown that septoplasty itself does not appear to cause an effect on the growth of the craniofacial skeleton, other studies have shown that untreated nasal respiratory obstruction can lead to the development of dental malocclusion, sinusitis, and disturbances of the growth of the midface and nose.21 Specifically, children who are obligate mouth breathers due to nasal obstruction are shown to develop increased upper and lower anterior facial height, larger gonial angle, and retrognathic position of the maxilla and mandible.21 Additionally, neonates are commonly preferential nasal breathers until the age of 6 months, so severe septal deviation can lead to significant respiratory distress. Septal deviation has also been shown to be associated with increased incidence of snoring, viral upper respiratory infections, bronchitis, and sinusitis in children.22 Chronic partial airway obstruction has also been shown to result in systemic complications such as pulmonary hypertension. When evaluating a patient to determine if they are a candidate for septoplasty based on the indication of nasal airway obstruction, it is important to do a thorough evaluation of the entire upper airway. It is rare for nasal septal deviation to be significant enough to be the sole cause of obstructive breathing, although it is possible. If nasal airway obstruction is the indication for performing septoplasty, it is important to rule out other causes of nasal obstruction such as nasal masses, choanal atresia, and hypertrophic adenoids.
Although uncommon, pediatric patients may also present with skull base pathologies and treatment with endoscopic endonasal skull base surgery may require concomitant septoplasty for access to the skull base.
Finally, a recent study by Levi et al. showed promising results when septoplasty is used for the treatment of recalcitrant idiopathic epistaxis in children.23 In this study, 20 patients were treated with either traditional septoplasty or modified septoplasty in which bilateral mucoperichondrial flaps are elevated but no septal cartilage is resected. Eighteen of the 20 patients had complete resolution of their epistaxis symptoms at their 1 month follow up. The pathophysiology of this treatment approach is thought to be related to the scarring of the causative vasculature on the elevated mucoperichondrial flaps as well as a decrease in turbulent airflow if septal deviation is addressed with traditional septoplasty techniques.23
| Table 1: Absolute and Relative Indications for Pediatric Septoplasty | |
| Absolute Indications | Relative Indications |
| Septal abscess with cartilage necrosis | Nasal airway obstruction |
| Recalcitrant idiopathic epistaxis | |
| Severe nasal deformity secondary to acute nasal fracture | Access for endonasal skull base surgery |
| Septal deformity secondary to a cleft | |
| Severe nasal obstruction resulting in sleep apnea | |
| Dermoid cyst Nasal mass |
Technique
The goal of surgery should be to restore normal anatomy, improve function, and promote normal nasal development. When performing a septoplasty in a pediatric patient, a preservation surgery is favored. Verwoerd and Verwoerd-Verhoef have published guidelines for technique when performing pediatric septoplasty based on experimental evidence and clinical observations. These guidelines indicate that elevating the mucoperichondrium for access to the cartilaginous septum, unilateral or bilateral elevation does not interfere with normal nasal development. The mucosa of the nasal floor should not be elevated to protect the incisive nerves and incisions through the key growth and support zones should also be avoided with particular attention paid to the sphenodorsal zone. As previously mentioned, damage to this zone may result in inhibited growth of the nasal dorsum in length and height. Posterior chondrotomy, or separation of the septum from the perpendicular plate, should be avoided when possible as it is thought this region is important in the development of length and height of the nasal septum and dorsum. However, resection of cartilaginous septum more anteriorly along the floor does not affect the outgrowth of the nasal dorsum. Transection of the septospinal ligament (decussating fibers) should be avoided to prevent unwanted forward growth of the maxilla. If the caudal rim of septal cartilage becomes subluxed, it should be repositioned into a columellar pocket and sutured between the medial crura. If cartilage is resected, it is preferable to replace with autologous septum or cartilage on a scaffold to prevent scarring between the bilateral mucoperichondrial flaps or septal perforation. If the upper lateral cartilages become separated from the septum, they should be re-approximated with sutures to prevent future deviations of the nasal dorsal cartilage. A popular biosynthetic material often now considered for use in the pediatric and adult population is the use of polydioxanone (PDS) plating or foil to prevent recurrent deviations and re-disolcation of grafts.24,25 PDS foil has also shown to stimulate some cartilage regeneration. The use of proplast and gore-tex has largely fallen out of favor due to inflammation, growth inhibition and severe deformities of the nose and midface. Particular attention should be paid to the cranial base when performing pediatric septoplasty as ossification of the septum and cartilaginous cranial base is variable in children, making the cranial base more prone to injury.17
Access to the pediatric septum can be difficult due to the small vestibular area that children have. This can make standard approaches that are used in adults extremely difficult to perform in a subset of the pediatric population. Therefore, in certain cases, a sublabial approach is used to access the septum. For the sublabial approach, an incision is made in the upper gingivolabial sulcus with the length approximating the width of the nasal base. Dissection is performed superiorly until the anterior nasal spine is encountered. The mucoperichondrium of the quadrangular cartilage is then elevated bilaterally26. However, most children do not require a sublabial approach and often their nasal development is sufficient enough for a standard endonasal approach with a Killian or hemitransfixion incision. Care must be taken to avoid placing the incision in the cutaneous portion of the caudal septum to avoid visible scarring and post-operative scar contracture.26 If scar contracture occurs, it may lead to columellar retraction and alteration of the normal nasolabial angle.
Outcomes
Many methods are available to assess whether septoplasty improves quality of life for children, including rhinomanometry, acoustic rhinometry, and quality of life (QOL) questionnaires. A specific QOL instrument that has been validated is the nose obstruction symptom evaluation (NOSE), developed by Stewart et al.27 This scale evaluates a patients symptoms including nasal congestion, nasal obstruction, difficulty breathing, trouble sleeping, and breathing during exercise or exertion. While it was originally developed to monitor outcomes in adult septoplasty, Yilmaz et al. used it to evaluate outcomes in the pediatric population.28 In their cohort of patients, there was a statistically significant improvement in postoperative NOSE scores compared to baseline. Can et al. also evaluated outcomes after pediatric septoplasty using acoustic rhinometry to quantify minimal cross sectional areas (MCSA) and total volume (TV).29 Acoustic rhinometry uses reflections of sound pulses introduced into the nasal cavity through the nares to determine these objective measures. Can et al. found that there was a statistically significant difference in these measures when comparing preoperative and postoperative values in patients that had a subjective improvement in their symptoms.
Conclusion
Septoplasty has a role in the management of pediatric nasal septal deviation and should be performed in cases where indications are met and has been shown to improve quality of life scores. Conservative management of septal deviations may lead to increased facial asymmetry. Importantly, lack of correction of a deviated septum in the developing midface may lead to deformities of both the nose and midface due to traction on important growth centers. More clinical studies are required to determine evidence for best timeline for correction in children younger than 6 years of age. Both the patient and parent should be counseled of the potential benefits of the surgery, and of the rationale to continue a follow-up of the facial growth. Endoscopic septoplasty has not been shown to cause a change in postoperative nasolabial angle.
References
- Freer O. The Correction Of Deflections Of The Nasal Septum With A Minimum Of Traumatism. JAMA. 1902;XXXVIII(10):636.
- Grymer L, Bosch C. The nasal septum and the development of the midface. A longitudinal study of a pair of monozygotic twins. Rhinology. 1997;35(1):6-10.
- Gilbert J, Segal S. Growth of the Nose and the Septorhinoplastic Problem in Youth. Plast Reconstr Surg. 1959;23(3):293.
- Farrior RT, Connolly ME. Septorhinoplasty in Children. Otolaryngol Clin North Am 1970;3:345-64.
- Sarnat B, Wexler M. The Snout After Resection of Nasal Septum in Adult Rabbits. Arch Otolaryngol. 1967;86(4):463-466.
- Hartshorn DF. Facial Growth Effects of Nasal Septal Cartilage Resection in Beagle Pups. Iowa City, IA: University of Iowa Press; 1970.
- Bernstein L. Early submucous resection of nasal septal cartilage: a pilot study in canine pups. Arch Otolaryngol. 1973;97(3):273-278.
- Cupero T, Middleton C, Silva A. Effects of Functional Septoplasty on the Facial Growth of Ferrets. Arch Otolaryngol. 2001;127(11):1367.
- Triglia JM, Cannoni M, Pech A. Septorhinoplasty in children: Benefits of the external approach. J Otolaryngol 19:274-278, 1990.
- Jugo S. Total Septal Reconstruction Through Decortication (External) Approach in Children. Arch Otolaryngol. 1987;113(2):173-178.
- Bejar I, Farkas LG, Messner AH, and Crysdale WS. Nasal growth after external septoplasty in children. Arch Otolaryngol Head Neck Surg 122:816-821, 1996
- El-Hakim H, Crysdale W, Abdollel M, Farkas L. A Study of Anthropometric Measures Before and After External Septoplasty in Children. Arch Otolaryngol. 2001;127(11):1362.
- Walker PJ, Crysdale WS, and Farkas LG. External septorhinoplasty in children: Outcome and effect on growth of septal excision and reimplantation. Arch Otolaryngol Head Neck Surg 119:984–989, 1993.
- Tasca I, and Compadretti GC. Nasal growth after pediatric septoplasty at long-term follow-up. Am J Rhinol Allergy 25:e7–e12, 2011.
- Tatum S. Pediatric Facial And Reconstructive Surgery, An Issue Of Facial Plastic Surgery Clinics Of North America, E-Book.; 2014:503-508.
- Vetter U, Pirsig W, Helbing G, et al. Patterns of growth in human septal cartilage: A review of new approaches. Int J Pediatr Otorhinolaryngol 7:63–74, 1984.
- Verwoerd C, Verwoerd-Verhoef H. Rhinosurgery in Children: Basic Concepts. Facial Plastic Surgery. 2007;23(4):219-230.
- Kawalski H, Śpiewak P. How septum deformations in newborns occur. Int J Pediatr Otorhinolaryngol. 1998;44(1):23-30.
- Christophel JJ, and Gross CW. Pediatric septoplasty. Otolaryngol Clin North Am 42:287–294, ix, 2009.
- Alshaikh N, Lo S. Nasal septal abscess in children: From diagnosis to management and prevention. Int J Pediatr Otorhinolaryngol. 2011;75(6):737-744.
- D’Ascanio L, Lancione C, Pompa G, et al. Craniofacial growth in children with nasal septum deviation: A cephalometric comparative study. Int J Pediatr Otorhinolaryngol 74:1180–1183, 2010.
- Blahova O. Late results of nasal septum injury in children. Int J Pediatr Otorhinolaryngol 10:137–141, 1985.
- Levi J, McKee-Cole K, Barth P, Brody R, Reilly J. Outcomes of recalcitrant idiopathic epistaxis in children: Septoplasty as a surgical treatment. Laryngoscope. 2016;126(12):2833-2837.
- Boenisch M, Tamas H, Nolst Trenite GJ. Influence of polydioxanone foil on growing septal cartilage after surgery in an animal model: new aspects of cartilage healing and regeneration (preliminary results). Arch Facial Plast Surg. 2003 Jul-Aug;5(4):316-9.
- Menger DJ, Tabink IC, Nolst Trenite GJ. Nasal Septal Abscess in Children: Reconstruction with Autologous Cartilage Grafts on Polydioxanone Plate. Arch Otolaryngol Head Neck Surg. 2008 Aug;134(8):842-7. doi: 10.1001/archotol.134.8.842.
- Healy G, Tardy M. Septorhinoplasty in children. Operative Techniques in Otolaryngology-Head and Neck Surgery. 1994;5(1):22-26.
- Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT, Development and validation of the nasal obstruction symptom evaluation (NOSE) scale, Head Neck Surg. 130 (2004) 157–163.
- Yilmaz M, Guven M, Akidil O, Kayabasoglu G, Demir D, Mermer H. Does septoplasty improve the quality of life in children?. Int J Pediatr Otorhinolaryngol. 2014;78(8):1274-1276.
- Can İ, Ceylan K, Bayiz Ü, Ölmez A, Samim E. Acoustic rhinometry in the objective evaluation of childhood septoplasties. Int J Pediatr Otorhinolaryngol. 2005;69(4):445-448.
