Adjunctive Cosmetic Procedures During Rhinoplasty and Sinus Surgery
Daniel G. Becker, MD, FACS
Department of Otorhinolaryngology-Head and Neck Surgery, University of Pennsylvania Hospital, Philadelphia, Pennsylvania
Address all correspondence to Dr. Daniel G. Becker, Dept. of Otorhinolaryngology-Head and Neck Surgery, Univ. of Pennsylvania Hospital, 3400 Spruce Street, 7 Silverstein, Philadelphia PA 19104; beckermailbox@aol.com
ABSTRACT: A number of patients undergoing nasal surgery such as endoscopic sinus surgery and rhinoplasty request whether facial cosmetic procedures can be performed at the same time. This report outlines some of the more common adjunctive procedures.
KEYWORDS: rhinoplasty, endoscopic sinus surgery, blepharoplasty, browlift, otoplasty, botox
Document ID# JLT1303-247-257(191)
1050-6934/03 $5.00 © 2003 by Begell House, Inc.
I. INTRODUCTION
At times, patients undergoing rhinoplasty and/or sinus surgery request other changes to their facial appearance. Perhaps the patient is bothered by eyelid bags, or perhaps they want to address a double chin. Perhaps the patient is bothered by poor facial skin quality, or has some other concern. Often, it is possible to address this other request at the same time as the sinus surgery or rhinoplasty. In this report we review some of the more common “adjunctive” procedures in rhinoplasty and endoscopic sinus surgery.
II. ADJUNCTIVE PROCEDURES
II.A. Botox
Botulinum toxin, or Botox, is a neurotoxin produced by the bacteria clostridia botulinum. When small doses of botox are injected into a muscle, it weakens or “paralyzes” that muscle. It has been used for many years in the treatment of muscle spasm disorders. Doctors and patients noticed early on in its use that it also caused lines and wrinkles to soften and even disappear for a period of time. As a result, the use of botox for the treatment of lines and wrinkles is now very common. Botox is now FDA approved for cosmetic use for specific facial wrinkles.
Botox works best on the wrinkles between the eyes, the crow’s feet or “laugh lines” that form with aging, and the furrows or forehead wrinkles that may give one a frowning or worried look (Fig. 1).
When administered in appropriate doses, Botox does not make the face expressionless. It simply softens over-exaggerated furrows. Its effects typically last about 4-6 months, and after that patients can be retreated. If patients like the effect of Botox, they may wish to discuss with their facial plastic surgeon the surgical options that can provide a more lasting solution.
There may be some mild discomfort associated with a Botox injection that can be treated with Tylenol. There will be some temporary swelling that usually requires no treatment. However, if a patient wishes, they can apply ice in the first 24 hours. There is usually no bruising. If a patient should develop a small bruise, it should dissipate over a period of a few days.
II. ADJUNCTIVE PROCEDURES
II.B. Blepharoplasty
The eyes are typically the first place to show signs of aging. The upper eyelid skin begins to droop as early as age 30, making the eyes appear smaller and tired. By age 40, fine wrinkling and unattractive pouching may appear below the eyes, and “crow’s feet” (or, more optimistically, “laugh lines”) begin to form. The eyebrows may droop along with the eyelid skin, which also makes the eyes appear smaller. The aging process continues and these changes progress into the 50s and beyond.
Blepharoplasty is the cosmetic surgical treatment of aging changes around the eyes. One of the reasons that cosmetic eyelid surgery is so popular is that the eyes are often a person’s most attractive feature, and the most often noticed. It is therefore unfortunate that the first signs of aging appear around the eyes. Happily, a number of conservative procedures are available that can address these inevitable changes.
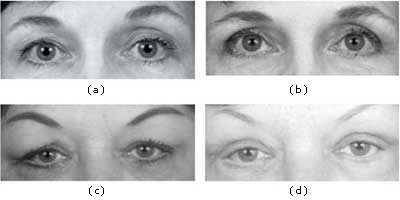
As with any patient concern, the first step is to learn from the patient what specific aspects of the aging changes are of greatest concern. Then, the facial plastic surgeon performs a careful examination to determine the exact reasons the patient’s eyes look as they do. If, as is most common, there is simply excess upper eyelid skin, then this can be removed in an operation called an upper eyelid blepharoplasty (Fig. 2). If, there is sagging or puffiness of the lower eyelids, a lower eyelid blepharoplasty may be offered (Fig. 3).
Sometimes, the only part of the lower eyelid that is sagging or bulging is the fat that surrounds the eye. In this situation, the incision may be hidden inside the eyelid, where it is not visible to any observer. This is the so-called “incision-less” eyelid surgery.
However, when the skin and muscle of the eyelid are sagging as well, some of it must be removed, so an incision may be made just beneath the eyelid. This incision allows the surgeon to tighten the eyelid skin to achieve a refreshened, smoother appearance. The incision is hidden in a natural crease just 1-2 mm beneath the eyelid, and is typically extremely difficult to see.
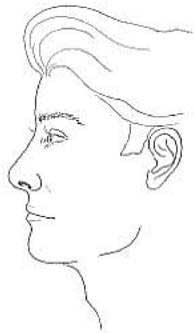
Many patients do not realize that with aging, the eyebrows sag along with the eyelids. Therefore, the eyebrows may also require a lift. In some patients, this is the main problem, while in other patients this is a secondary problem whose correction is therefore optional.³ Browlifting elevates the skin above the eyebrow and the eyelid skin beneath the eyebrow, so after a browlift less skin needs to be removed from the upper eyelid. For this reason, the patient needs to decide before the blepharoplasty whether a browlift is also desired (see Fig. 5 below).2
When patients state that their eyes get tired at the end of the day, there are several medical problems that should be checked for with the family doctor, optometrist, or opthamalogist. However, sometimes heavy excess skin can weigh down the patient’s eyelids and put extra strain on them, and hence cause them to tire by the end of the day.
The most common patient worry during the initial visit is that they have heard that cosmetic eyelid surgery can cause them to be permanently unable to close their eyes. The technical term for this is lagophthalmos, which means “inability to close the eyelids.” If too much skin is removed from the upper eyelid, itwill not be able to close. There are a number of special precautions that the wise surgeon undertakes before and during surgery to minimize this risk. There are other risks of this surgery that are not common, but that the surgeon should discuss in detail during the presurgical office visit.
II. ADJUNCTIVE PROCEDURES
II.C. Laser Resurfacing
Cosmetic eyelid surgery does not correct or improve the fine wrinkling that can occur with aging. In this situation, laser resurfacing (or some other resurfacing procedure) may be the best option (Fig. 4).4 Skin is a living organ. Every day, thousands of cells die, fall off , and are replaced by new cells from below. This is a haphazard process that does not allow the skin to shed dark spots, sun damage, or a dull lifeless complexion.
Laser resurfacing is a procedure in which a carbon dioxide laser (as well as some other types of lasers) is used to remove the outer layers of skin. The purpose of laser resurfacing is to cause the even, controlled removal of several layers of damaged cells. This allows a new fresh layer of skin to grow, with a more even texture and color. Before the laser resurfacing procedure, the surgeon should prescribe a skin cream for the patient to begin at least 2 weeks before the procedure to prepare the skin. All patients should be prescribed an antibiotic and an oral antiviral medication to begin prior to surgery. This is to prevent the outbreak of bacterial infection or cold sores/fever blisters during the healing phase. On the day of the procedure, patients are instructed to wear clothing that fastens in front or back. Patients are asked to avoid slipover sweaters, T-shirts, and turtlenecks and are instructed not to wear any earrings, makeup, or facial creams. Men should be closely shaven.

The patient is brought into the procedure room and placed in a reclining medical chair or table. Local anesthesia and intravenous sedation or general anesthesia are used as determined prior to the procedure. The patient’s face is cleansed to improve uniform uptake. The laser procedure is then performed. At the completion of the procedure, ointment is applied. Immediately after laser resurfacing, the resurfaced area will feel swollen, numb, and look slightly pink. It is normal to have significant swelling the night and morning after the procedure. This can be lessened by sleeping with the head elevated.
During days 7-30 after laser resurfacing, a patient’s skin will look sunburned. It may take up to 3 months for the redness to completely disappear, but after 7 days a patient should look socially acceptable with makeup. Patients may now resume their normal activities with the exception of sun exposure.
As with all surgical procedures, there are potential side effects and complications associated with laser resurfacing. Pigmentary changes after laser resurfacing can cause areas of increased or decreased pigmentation. This is more common in darker skinned individuals or those with a history of pigmented scars. The use of sunscreens and lightening gels will decrease the risk of these problems. Close follow-up and keeping all appointments with the doctor is important so that these problems can be treated early when they occur.
Some redness may last for up to 3 months. This is managed with skin care regimens and strict sun avoidance. Also, makeup can be used to camouflage any redness during this time. Infection may occur as a result of herpes simplex or bacteria. Preventative medications are routinely prescribed for this and are generally quite effective. Any signs of infection should be recognized early and treated with additional therapy as indicated. Scarring is a rare complication of the wound created by the laser resurfacing procedure, but it remains a potential complication of any procedure that wounds the skin. Close follow-up and keeping all appointments with the physician is important so that these problems can be treated early when they occur.
Patients may occasionally require more than one resurfacing procedure to achieve their best improvement. For most skin types, one procedure is enough to achieve the desired improvements, but some skin problems, such as excessive pigmentation from pregnancy or birth control pills, may require multiple procedures for maximum improvement. Everyone’s skin is different, so each program is tailored to the individual’s needs.
In the average resurfacing procedure, it takes 6-9 days to achieve complete re-epithelialization (growth of new, “revitalized” skin). During this time, the treated area will leak a straw-colored fluid. This is normal and typically stops within a week. It is most important during this phase for the patient to keep the area moist and avoid crusting.
Crusting delays healing, so the patient is instructed to apply liberal amounts of plain Vaseline. Using Vase-line that has been refrigerated may help further ease the discomfort or swelling. Patients may wash their face gently with a mild soap, but must not rub. Patients are instructed to gently pat their face with lather and splash with water. Any crusts should be gently soaked away with water or hydrogen peroxide on a gauze sponge. Patients should not rub or pick crusts. After washing, Vaseline may be liberally reapplied. Patients should avoid strenuous activity and sweating during the first week.
During healing, any pain can be easily controlled with medication. In most cases, ibuprofen, Tylenol, or Tylenol with codeine should be adequate to control any discomfort. Most people feel they look “strange” during the early healing phase, but if this is not a concern they can go out. However, they will not be able to be in the sun or do anything that would cause them to perspire heavily. It is of utmost importance for patients to wear sunscreen and strictly avoid the sun. Damage from UV rays can occur in winter, through car windows, and on cloudy days. For the best possible results, daily sunblock should be used for 6 months.
II. ADJUNCTIVE PROCEDURES
II.D. Browlift
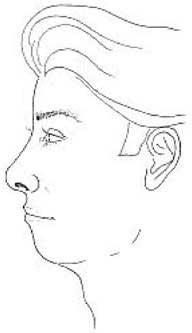
The eyes and eyebrows are among the most expressive parts of the face. An individual can express anger, worry, surprise, and other emotions by the position of his or her brows alone. The effects of time cause fur-rows in the brow and drooping of the eyebrows, which can cause an individual to appear tired or worried. A browlift is a procedure that repositions the brows to a more favorable position (Fig. 5).5
There are many ways to perform a browlift; the best approach varies with each patient. Each approach generally carries relative advantages and disadvantages that will be explained by the facial plastic surgeon. In general, browlifts are done through incisions that are hidden either in or behind the hairline. Sometimes, especially in male patients, the incision is hidden in a prominent forehead crease. A precise amount of skin is removed and the incision or incisions are stitched closed, thereby elevating the brows as desired.
By matching the advantages and disadvantages of each type of browlift with a patient’s anatomy, it usually becomes clear to patients that one particular browlift is the right one for them. Browlifting is commonly performed under sedation or general anesthesia. After the operation, a dressing and elastic bandage are typically applied, which remain in place for a few days.
FIGURE 5. Endoscopic browlift and upper eyelid blepharoplasty (a,c) preoperative, (b,d) postoperative.
II. ADJUNCTIVE PROCEDURES
II.D. Browlift
2. Coronal Browlift
A coronal browlift is performed by making a long incision in the scalp behind the hairline. An exact amount of scalp tissue is removed, the forehead tissue is lifted, and the incision is sewn together. This repositions the brow upward, causing the “lift.” The coronal browlift is a reliable approach for achieving browlift and is a commonly used approach. In a female patient without any thinning of hair, it is a nice way to address moderate to major brow drooping, as long as the patient understands that she will have some numbness from just behind the incision to the top of her scalp. This is usually temporary, resolving over a period of several months, but in some cases it can be longer lasting or even permanent.
In men, the coronal browlift is not commonly used because of the likelihood of balding. With balding, the scar would become exposed. In men, the coronal browlift is only considered if they have a thick head of hair with no family history of balding, and if they meet other criterion for coronal browlift. The coronal browlift will raise the hairline, so if a patient already has a high hairline, another approach may be prefer-able.
3. In-Front-of-the-Hairline Browlift
An “in-front-of-the-hairline” browlift, known by surgeons as a pre-trichophytic lift, is the approach used in women who would be candidates for a coronal brow-lift, except for the fact that they have a high hairline. The incision typically heals well, is extremely well hidden, and is rarely a problem for the patient. The same considerations regarding numbness and balding apply here as for the coronal browlift.
4. Midforehead Browlift
A midforehead browlift is especially effective in male patients with a prominent forehead crease and is in women with prominent forehead creases as long as they understand that they will have scars on their forehead that will be hidden within the crease but that will be a little more prominent while they are healing (a period of several months). Women who can accept this are actually good patients, because they are more likely than males to camouflage the scars with makeup during this normal healing process.
In this approach a precise amount of skin is re-moved and the incisions are stitched closed, thereby elevating the brows as desired. At times, absorbable “suspension sutures” are placed deep beneath the skin to provide additional support during the healing process. The midforehead browlift is easily performed under light sedation and even local anesthesia. The numbness described in some of the other lifts is not typically a consideration. The main drawback of this approach is the incisions, which becomes a nonissue if the patient has forehead creases and understands and accepts the placement of incisions in these creases.
Most browlifts are performed under sedation anesthesia or general anesthesia. In an occasional patient undergoing a mid-forehead browlift, the surgeon may use local anesthesia only. It is generally not necessary to cut any of the patient’s hair. Some swelling and bruising are normally present after browlifts, but the degree of each varies widely from patient to patient. Generally, most patients appear quite sociably accept-able within 10-14 days after surgery.
II. ADJUNCTIVE PROCEDURES
I.E. Double Chin
Fat accumulation that occurs beneath the chin (the “double chin”) is often a major source of distress. Significant improvement in a patient’s profile can be achieved by removing this fat (Fig. 6).” Liposuction of the double chin is performed under local anesthesia or under local anesthesia plus sedation. Patients who undergo this procedure in conjunction with rhinoplasty may have sedation or general anesthesia.
After the operation, a dressing and elastic bandage are typically applied to remain in place for a few days. The surgeon or his/her assistant will typically see the patient the day after surgery, at which time this bandage is removed and replaced with a smaller removable one. The patient is asked to wear this bandage for another full day, and then only at night for 3 days thereafter. The patient may gently shampoo the hair 24 hours after surgery.
Some swelling and bruising are normally present after liposuction. Generally, most patients appear quite sociably acceptable within a few days after surgery. The patient’s head should be elevated on at least two pillows during sleep for the first 14 days, in order to keep the head higher than the heart to help facilitate the resolution of swelling. Patients may be up and around the day after surgery, but some naturalfatigue may persist for 2-3 days as a result of the normal effects of the anesthesia and surgical procedure. In general, the patient should restrict normal activities, exercise regimens, and any activity requiring lifting or straining for approximately 14 days. It is acceptable to do some light walking 72 hours after surgery. Jogging and light noncontact exercises should not be resumed for 3 weeks, and strenuous sports require 6 weeks of healing before being safely resumed.
II. ADJUNCTIVE PROCEDURES
II.F. Chin Implant
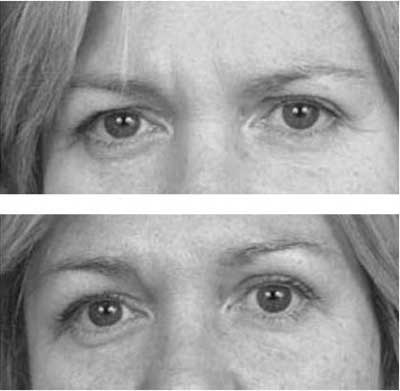
In some patients seeking rhinoplasty, a deficient or underdeveloped chin contributes to the undesirable nasal appearance. Specifically, a smaller chin can make a nose appear bigger (Fig. 7). Some patients already recognize this, while some patients are surprised to learn of this relationship between the nose and the chin. Rather than making the nose too small, in some situations the rhinoplasty surgeon may talk to the patient about making their nose just a bit smaller and at the same time augmenting their chin to achieve facial balance.
FIGURE 7. A small chin can make a nose appear bigger. This diagram (a) preoperative, (b) postoperative illustrates the effect on facial proportions of a change to the chin alone.
II. ADJUNCTIVE PROCEDURES
II.G. Otoplasty
Ears that protrude prominently draw attention to themselves and may be a cause of distress. Otoplasty is an operation that repositions the ears to a less prominent position (Fig. 8).¹0 Otoplasty is often performed in patients when they are children, before they begin school, because their young classmates can be quite merciless in their teasing or taunting. Adults with prominent ears occasionally choose to have their ears repositioned as well.
Commonly referred to as “pinning back the ears,” otoplasty involves an incision on the back side of the ear with removal of some skin. The cartilage of the ear is repositioned by weakening it, removing some of it, and/or suturing it, depending upon what’s best for that patient’s ears. Some swelling and bruising around the ears is normally present after otoplasty. Generally, most patients appear quite sociably acceptable within 1-2 days after surgery because the incision is hidden behind the ear. In fact, the ears may be completely hidden if the patient’s hair is long.
III. CONCLUSION
Botox injections, blepharoplasty, laser resurfacing, browlift, liposuction of the neckline, and chin implant may be performed at the same time as rhinoplasty and/or endoscopic sinus surgery. These adjunctive cosmetic procedures allow the interested patient to address both their nasal problem as well as any concerns with their facial appearance at the same time.
References
- Blitzer A, Binder WJ, Brin MF. Botulinum exotoxin A (Botox) for facial wrinkles. In: Papel et al., editors. Facial Plastic and Reconstructive Surgery. 2 ed. New York: Thieme, 2002.
- Pastorek NJ. Upper lid blepharoplasty. In: Papel et al., editors. Facial Plastic and Reconstructive Sur‑gery. 2 ed. New York: Thieme, 2002.
- Rankin BS, Arden RL, Crumley RL. Lower lid blepharoplasty. In: Papel et al., editors. Facial Plastic and Reconstructive Surgery. 2 ed. New York: Thieme, 2002.
- Carniol PJ, Harmon CB. Laser facial resurfacing. In: Papel et al., editors. Facial Plastic and Reconstructive Surgery. 2 ed. New York: Thieme, 2002.
- Quatela VC, Graham HD, Sabini P. Rejuvenation of the brow and midface. In: Papel et al., editors. Facial Plastic and Reconstructive Surgery. 2 ed. New York: Thieme, 2002.
- Keller GS, Endoscopic Facial Plastic Surgery. St. Louis, MO: Mosby-Year Book, 1997.
- Becker DG, Kallman JE, McLaughlin RB. Endo‑scopic techniques and powered instrumentation in facial plastic surgery. Curr Opin Otolaryngol Head Neck Surg 1998:232-237.
- Kridel RWH, Kelly PE. Liposuction of the face and neck. In: Papel et al., editors. Facial Plastic and Reconstructive Surgery. 2 ed. New York: Thieme, 2002.
- Binder WJ, Moelleken B, Tobias GW. Aesthetic fa‑ cial implants. In: Papel et al., editors. Facial Plastic and Reconstructive Surgery. 2 ed. New York: Thieme, 2002.
- Nachlas NE. Otoplasty. In: Papel et al., editors. Fa‑cial Plastic and Reconstructive Surgery. 2 ed. New York: Thieme, 2002.