Abstract
Injection rhinoplasty is very popular in Asian countries for its minimally invasive nature and versatility in making minor changes in the nasal contour. Hyaluronic acid can be used for dorsal augmentation and for fixing a dorsal hump, deviated nasal dorsum, asymmetrical lateral nasal wall and prominent nasal implant. Injectors must make an accurate diagnosis of the defects and know the nasal anatomy well so that they can inject to the right level and position and avoid potentially serious complications. Patients should be followed up closely.
Introduction
Augmentation rhinoplasty is the most commonly performed rhinoplasty in Asian patients and is in very high demand in Asian countries.1,2 This high demand is attributable to the anatomical characteristics of the Asian nose. Asians have a relatively poorly developed nasal bone compared with Caucasians, resulting in a low radix and weak and small upper and lower lateral cartilages that result in a low dorsum and nasal tip. In addition, the skin and soft tissue envelope of the Asian nose are relatively thick. All of these anatomical factors result in a relatively flat and small nose. To achieve an aesthetically pleasing nose, augmentation rhinoplasty has become the most popular cosmetic surgery in Asian countries. Nose augmentation using autologous grafts or implants needs a long recovery time and may involve surgical complications.
Rhinoplasty in the Chinese population mainly focuses on raising the nasal dorsum and excludes the correction of other parts of the nose such as the nasal tip or alar according to the well-known gold standard of noses considered in Chinese face reading. In Chinese face reading, it is believed that our noses govern our financial luck. A high nasal dorsum means higher self-esteem and a greater likelihood of becoming famous. Further, a fleshy nasal tip means you are kind and wealthy, and invisible nostrils signify that you can save money. Therefore, most Chinese people are not keen on correcting their tip volume and rotation. Dermal filler is capable of precisely smoothing out irregularities and asymmetries in the nose post rhinoplasty. Therefore, injection rhinoplasty using dermal filler has become more popular and has replaced many surgical augmentation rhinoplasty procedures in the recent decades. In our centre, we use dermal filler not only for augmentation but also as an enhancer in rhinoplasty.
Selection of dermal filler materials
Several types of dermal filler materials are available for injection rhinoplasty.3 While selecting the filler material, it is important to consider its texture after injection, duration, reversibility and safety. Hyaluronic acid (HA) derivatives and calcium hydroxylapatite gels have recently gained popularity over other filler materials.
In our centre, HA fillers are generally used for injection rhinoplasty because they are relatively safe and reversible and provide a natural texture to the nose. HA is a main component of normal skin, forming the largest part of the extracellular matrix of the dermis. Its chemical structure is identical across species, and this uniformity minimises the likelihood of immunogenicity. Further, in cases of serious complications of vascular compromise that may lead to skin necrosis or blindness, hyaluronidase, an enzyme that degrades HA and is widely available, can be administered to reduce arterial insufficiency or venous congestion.
To reduce the risks of nasal vascular compromise, we generally use HA products with relatively smaller particle size such as Restylane (Medicis Aesthetics, Scottsdale, AZ). The risk of nasal vascular compromise increases when large amounts of HA (more than 0.5 ml) are placed in the nose, particularly HA products with larger particles such as Perlane (Medicis Aesthetics, Scottsdale, AZ) or Juvederm Ultra Plus (Allergan, Irvine, CA.).4 In addition, HA can be easily removed in revision surgery compared with other filler materials such as calcium hydroxyapatite, which tends to cause fibrosis in the surrounding tissues.
However, limited longevity is a limitation of HA. In most patients, the longevity of the injected HA is approximately 6 months, but this is highly variable depending on the molecular size and cross-linking of HA. The durability of HA is shorter in areas with more movement,5 if it is located in the more superficial dermis,6 and if monophasic polydensified cross-linked HA is used.7 However, one study reported an HA longevity of 18 months in some patients.4 We also experienced a patient in whom the HA filler injected to the dorsum for augmentation lasted for 18 months. In highly selected cases, we offer injection of longer lasting materials such as polyacrylamide hydrogel Aquamid® (Contura International, Soeborg, Denmark) when the post-rhinoplasty patients return for repeat injection. This material is widely resistant to enzymatic degradation and phagocytosis. However, despite the long lasting nature of the material, we do not use it widely because of its reported risk of infection, which may present early or late. This material has an exceedingly biocompatible nature and thus is an excellent growth medium for bacteria.8 Nevertheless, we have been using it in our centre for over 10 years and have not reported a case of early or late infection to date. Therefore, now we let the patients choose between HA or polyacrylamide hydrogel for repeat injection.
Selection of patients for injection rhinoplasty
We consider the following indications to perform injection rhinoplasty using dermal fillers:
- Inadequate radix projection
- Dorsal hump and other irregularities
- Deviated nasal dorsum (C or S shape)
- Asymmetric lateral nasal wall
- Prominent or deviated nasal implant
Inadequate radix projection
Injection to the radix can be a primary procedure or secondary to a surgical rhinoplasty for inadequate radix projection. Injection to the radix is relatively straightforward, but the filler material needs to be kept within the height of the supratarsal creases9 because a higher placement of the filler material would create a straight frontonasal angle and an unnatural ‘surgical look’ or ‘Avatar-look’. For Asians, we usually recommend keeping the upper limit of the injection at the supratarsal crease or 5–8 mm from the ciliary margin in cases of single eyelid to retain much of the natural ethnic appearance. We usually fill the area between the new radix and supratip area instead of the nasal tip to avoid the creation of a bulbous nasal tip.






[Patient showing low radix before injection of HA: (1a) frontal view, (1b) cephalic view, (1c) left lateral view. Injection of 1.0cc of HA to radix and dorsum: (1d) frontal view, (1e) cephalic view, (1f) left lateral view.]
Dorsal hump and other irregularities
Nasal dorsal hump can be easily camouflaged by injecting dermal filler above the hump. This is an especially useful technique in Asian people when they do not want to reduce the hump in rhinoplasty, which could otherwise make the dorsum look lower than the pre-treatment condition. In addition, some patients may present with minor dorsum irregularities such as callous formation in the nasal bone secondary to nasal trauma such as bone fracture. Such minor dorsum irregularities can also be managed by injecting dermal filler to camouflage the irregularities with good results. The treatment involves injecting filler from the superior extent of the hump upwards to the radix. The upper limit of injection should not exceed the supratarsal crease as the resulting dorsal augmentation may give an unnatural look. This technique is suitable for small dorsal humps, whereas a large dorsal hump may need to be corrected by surgical rhinoplasty.


[Patient with a dorsum hump before injection (fig 2a). Injection of 0.3cc of HA to the radix above the hump performed (fig 2b)]
Deviated nasal dorsum (C or S shape)
Some patients present with a C- or S-shaped nasal dorsum due to grossly deviated nasal septum. When they are not keen on surgical correction or an aesthetic problem was not addressed during the functional rhinoplasty, dermal filler injection is performed. A lady presented to us with a grossly deviated nasal septum and dorsal profile and requested aesthetic improvement with much less downtime than a rhinoplasty. Dermal filler injection was performed to correct her nasal profile. She experienced only mild nasal skin swelling, which subsided totally in 3 days.


[Patient with a S-shape deviation of nasal dorsum. Before injection of HA (3a) and injection of 1.2cc of HA performed to radix and right side of lateral nasal wall (3b)]
Asymmetric lateral nasal wall
Hafezi reported that facial asymmetry is very common although some facial asymmetry is less obvious than others.10 The cause of asymmetric lateral nasal wall is unknown. Hafezi further studied 5822 patients who underwent rhinoplasty and found that most of the patients had a significant growth retardation of the midface and orbit on the concave side of the nose. He suggested that the midface growth retardation was the cause of the asymmetry in the lateral nasal bone. 11
An asymmetric lateral nasal wall usually involves a concavity on one side with or without convexity on the other side. We can inject a small amount of filler to the concave side to straighten the nose. The key to success is again accurate assessment of the defect and injection to the appropriate region under good lighting.
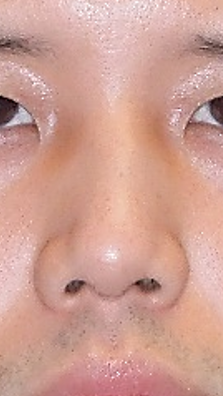


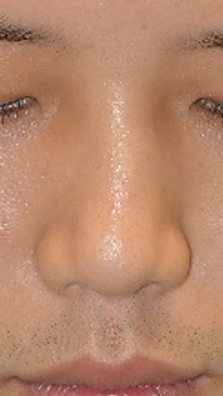
[Patient with asymmetrical lateral nasal wall. Pre-treatment photos: (4a) frontal view, (4b) cephalic view. Injection of 1.0 cc of HA performed to right side lateral nasal wall and radix: (4c) frontal view, (4d) cephalic view.]
Prominent or deviated nasal implant
Occasionally, some patients with nasal dorsal implants, either autologous costal cartilage or synthetic material, show a prominent para-implant sulcus after skin swelling subsides at 3–4 months post-operatively. The aesthetic result is suboptimal because the implant shape is prominent at the dorsum. In such cases, we inject a limited amount of dermal filler at the sulcus around the implant to fill up the sulcus.
Another indication is deviation of the dorsal implant. This can occur when the subperiosteal pocket is not adequately tight to hold the implant in the revision case. In addition, a costal cartilage may result in a warped or curved look. In such cases, dermal filler is injected to an appropriate site around the implant to balance the curvatures. Again, it is crucial to accurately assess the curvatures under adequate lighting and put the filler material at appropriate sites to create a balanced look.
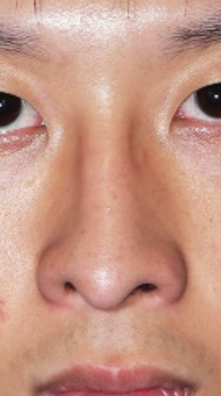



[Patient showing a prominent dorsal implant 6 months after augmentation rhinoplasty. Pre-injection photos: (5a) frontal view, (5b) cephalic view. Injection of 1.0cc of HA to para-implant sulcus performed: (5c) frontal view, (5d) cephalic view.]
Some surgeons advise not to add filler material on the nasal implant because the vascular anatomy of the nose changes after surgical rhinoplasty and filler injection may increase the risk of vascular complications. The risk is higher in patients with a silicone implant because of the avascular capsule around the implant, which greatly increases the risk of infection and subsequent implant extrusion. In our centre, we usually use expanded polytetrafluoroethylene (GoreTex soft tissue block) or costal cartilage to augment the dorsum in surgical rhinoplasty. In the past 15 years, no case of implant infection after the injection at the para-implant sulcus has been reported. Patients are usually very satisfied after this simple office procedure.
Although filler injection has versatile use in rhinoplasty, some cases cannot be managed easily and need to be further managed with a revision surgery.
Practical tips for the procedure
Patients should have a formal photo documentation of the frontal, basal, helicopter and left and right lateral and oblique views before the rhinoplasty procedure. Before the procedure, the patients sign an informed consent form that provides a clear explanation of the possible intra-operative and post-operative complications. The patients are then informed that touch up is usually done in 2 weeks’ time. We also explain that we prefer to avoid over-injection to prevent an unnatural look, so to avoid over-injection, we stop injection once skin swelling starts.
Good lighting and set up are crucial during the procedure of injection rhinoplasty. We perform it in our treatment room. Patients are required to remove all make up before the procedure. Local anaesthetic (lidocaine 2.5% and prilocaine 2.5% topical cream) is applied to the nasal skin for 45 minutes. Subsequently, the patients are asked to sit on the examination chair, which is then reclined to the flat horizontal position. Two surgical lights are shone on the nose from the left and right sides. These two lights allow the surgeons to clearly see the contour of the nose, e.g. in case of dorsum irregularities or asymmetric lateral nasal wall, the defect can be observed accurately and fixed.

During the procedures, aseptic practices are strictly followed. We use 2% chlorhexidine gluconate in 70% isopropyl alcohol to clean the entire nose and forehead skin. Chlorhexidine-based antiseptic agents have become popular because they offer the quick-acting ability of alcohol with much longer durability and higher efficacy.12 However, it is important to prevent the solution from entering the eyes because of the risk of keratitis and ocular injury. In addition, we put a sterile towel on the patient’s forehead and chest to create a sterile field. We wear sterile gloves for the procedure. We use a 27-gauge needle to inject the filler to the deep fatty layer immediately above the periosteum or perichondrium. The safety of injecting at this level is supported by Tansatit and colleagues who performed a histological analysis of nasal arteries and found that most of the nasal arteries found in the midline are in the subcutaneous layer. They also suggested several areas unsafe for injection, namely the infratip, rhinion and supratip.13 Some opinions support the use of cannulas for filler injection due to the lower risk of penetrating the vessels, bruising and vascular complications. However, many facial plastic surgeons14 do not agree that cannulas are safer than needles because aspiration may not be reliable when the bevel of the needle may be suctioned against the vessel wall, which could prevent aspiration. Furthermore, a large deposition of filler material can externally collapse a vessel even if it does not embolize it. In contrast, the use of needle allows precise placement of a small amount of filler to correct defects in small areas. In addition, the injectors who know the anatomy of nasal vasculature well can easily gauge the level of placement when using a needle, thus increasing the safety of the procedure.
In case of bleeding during the procedure, we compress the skin for few minutes using sterile gauze with light pressure to prevent bruising of the skin. After slowing injecting the filler material to the desired position, we apply digital pressure with a sterile gauze to mould the shape into position to create a natural look.
After the procedure, we instruct the patients to keep the nasal skin clean and avoid using old make-up pads on the face to prevent wound contamination. We tend to avoid over-injecting the filler material during the first procedure because whether an appropriate amount of filler material is used cannot be accurately judged when the skin is oedematous after the procedure due to repeated punctures of the skin. Usually, we follow up the patients 2 weeks after the procedure, which is when we assess the shape and decide whether further touch up is required. Some clinicians may worry about the sterility of stored dermal filler for later use. Alharbi reviewed nine studies on this subject and concluded that there is no risk of biofilm formation in stored fillers.15 Nevertheless, he recommended some precautions to minimise the risk of contamination, including the use of long-lasting germicidal such as both alcohol and povidone iodine for skin preparation, storing syringes in a refrigerator, immediately replacing needles used in injection with a sterile substitute before storage, and squeezing out tiny drops of stored filler before use to reduce the risk of retrograde contamination.15
Complications of injectable fillers
Injection rhinoplasty is a relatively safe office-based procedure compared with surgical rhinoplasty, but it is not without risks. Fortunately, severe complications of vascular compromise leading to tissue necrosis and blindness are rare. Other complications include swelling, bruising, mild asymmetry, inflammation, infection and vascular compromise.
Swelling occurs in almost every patient with varying severity after injection rhinoplasty. Most cases of swelling are transient and subside in 2 to 3 days.
Bruising occurs due to vascular damage by a needle. Although it subsides by itself in 2 weeks and does not affect the aesthetic result, it is better to prevent it from occurring. Patients are advised to stop anticoagulants (preferably after formal consultation with a physician) or herbs that can cause blood thinning 7–10 days prior to treatment.16,17 In addition, injecting in the right plane is essential to avoid vascular puncture. Further, if bleeding occurs during the procedure, sterile gauze should be used to apply pressure on the bleeding site for a few minutes.

Mild asymmetry can be due to undercorrection or overcorrection. This can be prevented by proper assessment of the nasal defects and precise placement of the needle tip before slowly injecting the filler. Undercorrection can be easily fixed with filler touch-up, but overcorrection is better avoided. Occasionally, asymmetry is an illusion caused by asymmetry of the facial bones, and it is important to point this out to the patient before the procedure.
Inflammation that causes persistent erythema usually responds well to a short-term medium-strength topical steroid therapy. However, the use of high-potency topical steroids should be avoided to prevent hypopigmentation and telangiectasia.
Infection can occur due to inadequate sterilisation during injection or contamination of needle puncture sites after the procedure. It can present as localised skin infection, a deeper cellulitis or abscess formation. If cellulitis is not controlled early with oral antibiotics, it may progress to abscess formation that needs more vigorous wound care and intravenous antibiotics. In such cases, there is a risk of hypertrophic scar formation after the infection and abscess are resolved. Herpes prophylaxis with an antiviral agent is recommended in patients with a history of herpes infection. A panel of experts recommended valaciclovir 1 g/24 h 1 day before and 3 days after filler injection.18
A lady who underwent injection rhinoplasty with polyacrylamide gel in another centre presented 1 week later at our centre with a pustular abscess and swelling over the nasal dorsum and tip. She was admitted to our hospital for intravenous antibiotic administration and wound dressing. Fortunately, acute infection and inflammation subsided in 4 weeks. Telangiectasia occurred on the nasal skin with mild hypertrophic scar formation after 3 months. We arranged three sessions of fractional CO2 laser for skin resurfacing. The nasal skin has remained in good condition without hypertrophic scarring or discoloration for 2 years.




[(Fig 8a): Post injection of filler infection presented with abscess pustule formation on nasal dorsum. (Fig 8b): After 4 weeks’ treatment of antibiotics and daily dressing. (Fig 8c): Dorsal skin showed telangiectasia and mild hypertrophic scar after 3 months. (Fig 8d): Given 3 sections of fractional CO2 laser to nasal skin, it showed good cosmetic result.]
Vascular compromise is the most severe, major and immediate complication of injection rhinoplasty because it can cause dermal necrosis and blindness. It always results from intravascular injection into an artery, causing an embolus that impedes blood flow. Prompt recognition of the vascular event and aggressive treatment are needed to avoid irreversible complications. The two primary diagnostic symptoms of vascular compromise are pain and changes in the skin colour. Arterial occlusions present with immediate, severe and disproportionate pain and skin colour change.19 Venous occlusions present with less severe, dull, or even no pain. Injecting at the nasal dorsum and lateral nasal wall is relatively safe as it is easy to limit the injection at these sites. However, injection of HA with hydrophilic and expansive properties at the nasal tip may compromise the vascular supply of the tip after post-surgical scar formation.
For the management of vascular compromise, consensus groups of experts18,19 recommend immediate cessation of the injection and facilitation of blood flow to the affected area using hyaluronidase, massage with warm compresses, and applying 2% nitroglycerin paste to promote vasodilatation. Hyaluronidase should be injected immediately and used daily in liberal doses where signs and symptoms are present.
Conclusion
The final results of rhinoplasty depend not only on the surgical technique but also on individual patients’ tissue healing and scar formation. As injectable fillers are very useful for fine touch-ups after rhinoplasty, I always mention their use to patients before rhinoplasty so that later on patients do not think that the dermal filler was used due to a post-operative complication. We usually recommend the use of fillers comprising short-lived materials such as hyaluronic acid for safety reasons. Furthermore, accurate photo documentation of the injection sites and volume should be kept for legal reasons and to obtain reproducible results when performing repeat injections in the future. Lastly, knowing the nasal anatomy well before injection is crucial to avoid serious complications.
References
- Liao WC, Ma H, Lin CH. Balanced rhinoplasty in an oriental population. Aesthetic Plast Surg. 2007;31:636-642
- Tham C, Lai YL, Weng CJ, et al. Silicone augmentation rhinoplasty in an Oriental population. Am Plast Surg. 2005;54:1-5; discussion 6-7
- Jasin ME. Nonsurgical rhinoplasty using dermal fillers. Facial Plast Surg Clin North Am. 2013;21(2):241-252
- Humphrey CD, Arkins JP, Dayan SH. Soft tissue fillers in the nose. Aesthet Surg J. 2009;29(6):477-484
- Matarasso SL, Carruthers JD, Jewell ML, et al. Consensus recommendations for soft-tissue augmentation with nonanimal stablized hyaluronic acid (Restylane). Plast Reconstr Surg. 2006;117 Suppl 3:3S-34S; discussion 35S-43S.
- Arlette JP, Trotter MJ. Anatomic location of hyaluronic acid filler material injected into nasolabial fold: a histologic study. Dermatol Surg. 2008;34 Suppl 1:S56-S62
- de Costa A, Biccigo DGZ, de Souza Weimann, et al. Durability of three different types of hyaluronic acid fillers in skin: Are there differences among biphasic, monophasic monodensified, and monophasic polydensified products? Aesthet Surg. 2017;37(5):573-581
- Zarini E, Supino R, Pratesi G, et al. Biocompatibility and tissue interactions of a new filler material for medical use. Plast Reconst Surg. 2004;114(4):934-942
- Kim P, Ahn JT. Structured nonsurgical Asian rhinoplasty. Aesthetic Plast Surg. 2012;36:698-703
- Hafezi F, Javdani A, Naghibzadeh B, et al. Laterality and left-sidedness in the nose, face, and body: A new finding. Plast Reconstr Surg Glob Open. 2017;5(12):e1590
- Hafezi F, Naghibzadeh B, Nouhi A, et al. Asymmetric facial growth and deviated nose: a new concept. Ann Plast Surg. 2010;64(1):47-51
- Reichel M, Heisig P, Kohlmann T, et al. Alcohols for skin antisepsis at clinically relevant skin sites. Antimicrob Agents Chemother. 2009;53(11):4778-4782
- Tansatit T, Moon HJ, Rungsawang C, et al. Safe planes for injection rhinoplasty: A histological analysis of midline longitudinal sections of the Asian nose. Aesthetic Plast Surg. 2016;40(2):236-244
- Kontis TC, Bunin L, Fitzgerald R. Injectable fillers: Panel discussion, controversies and techniques. Facial Plast Surg Clin North Am. 2018;26(2):225-236
- Alharbi M. Review of sterility of reused stored dermal filler. J Cosmet Dermatol. 2019;18:1202-1205
- Fitzgerald R, Bertucci V, Sykes JM, et al. Adverse reactions to injectable fillers. Facial Plast Surg. 2016;32(5):532-555
- Signorini M, Liew S, Sunderam H, et al. Global aesthetics consensus: avoidance and management of complications from hyaluronic acid fillers—evidence- and opinion-based review and consensus recommendations. Plast Reconstr Surg. 2016;137(6):961e-971e
- Urdiales-Gálvez F, Delgado NE, Figueiredo V, et al. Treatment of soft tissue filler complications: expert consensus recommendations. Aesthetic Plast Surg. 2018;42(2):498-510
- Sclafani AP, Fagien S. Treatment of injectable soft tissue filler complications. Dermatol Surg. 2009;35 Suppl 2:1672-1680
