Harvesting Ethmoid Bone
The perpendicular plate of the ethmoid bone and/or the vomer may be used as a splinting graft in the treatment of a deviated cartilaginous septum. Ethmoid bone may be harvested via a standard septoplasty approach.
Harvesting Conchal Cartilage: Anterior Approach
Auricular cartilage can be harvested using the anterior or posterior approach (1-6). In most cases, we prefer the anterior approach because we believe it is less traumatic, and the incision heals well if vertical mattress closure is used. If smaller cartilage grafts are needed, then we use the posterior approach.
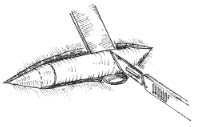
With a marking pen, outline an incision that follows the outer edge of the cavum and cymba concha. This incision should he placed along the portion of the concha that is vertically oriented in relation to the lateral aspect of the skull (Fig. 1). Use a syringe with 1% lidocaine (Xylocaine) solution with 1:100,000 epinephrine (or for the lab demonstration, water) to “hydrodissect” the skin of the concha cavum and cymba from the underlying cartilage.
Make the incision with a no. 15 blade, and elevate the skin and perichondrium from the underlying cartilage. Dissection proceeds by using appropriate scissors, and also bluntly with cotton-tip applicators. Care should be taken not to damage the soft auricular cartilage, which can tear. The dissection should stop short of the cartilage of the external auditory canal. The radix helicis should be preserved if preservation of ear position is critical. If the entire conchal bowl in excised, the auricle will usually settle closer to the head.
Dissect out the desired piece of cartilage, and leave the underlying muscle behind (perichondrium will remain adherent to the posterior surface of the cartilage). Avoiding deep dissection into the soft tissue minimizes bleeding.
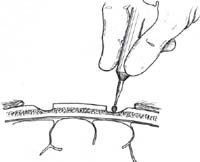
Suture the circumferential incision with a 6-0 nylon running mattress suture. Alternatively, the incision may be closed with interrupted vertical mattress sutures. Special care must be taken to avoid overlap of the skin edges. Place a bolster dressing of Telfa, dental roll, or other suitable material into the concha, and suture it into position to decrease the risk of hematoma. No residual deformity of the pinna is expected with this approach.
Figure 1. A-T: Injection hydrodissects the skin of the concha cavum and cymba from the underlying cartilage (A). The incision follows the outer edge of the cavum and cymba concha and is placed along the portion of the concha that is vertically oriented in relation to the lateral aspect of the skull (B, C). Dissection proceeds by using appropriate scissors, and also bluntly with cotton-tip applicators (D—G). The dissection stops short of the cartilage of the external auditory canal. Incise the cartilage (H, I) and dissect out the desired piece of cartilage (J, K). Achieve perfect hemostasis before closure (L). The cartilage should be handled gently to avoid tearing or damaging the soft auricular cartilage. Suture of the circumferential incision is shown here with a 6-0 nylon running vertical mattress suture (M-P). Alternatively, one may close the incision with interrupted mattress sutures. Place a bolster dressing of Telfa, dental roll, or other suitable material into the concha and suture it into position (Q-T) to decrease the risk of hematoma.
Harvesting Rib Graft
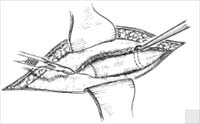
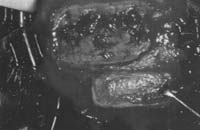
Cartilage is typically harvested (Fig. 2) from the eighth and ninth ribs or the confluence. If additional cartilage is required, the tenth rib also may be harvested. Bone may be harvested with the ninth rib if desired.
A 4-cm to 6-cm incision overlying the eighth rib allows adequate exposure. Dissection proceeds to and then through the rib perichondrium. The muscle fibers can be separated in-stead of cut to minimize postoperative pain. Dissection around the rib is undertaken subperichondrially; the pleura is typically closely adherent to the perichondrium. With the graft completely separated from surrounding soft tissue, the graft is incised and delivered under direct vision. The surgeon may elect to place a malleable retractor beneath the rib as it is incised. Saline is placed in the surgical site and Valsalva or positive pressure applied to check for a pleural leak. If a pleural tear is identified, a pursestring suture closure is un dertaken around a red-rubber suction catheter. The surgeon then requests a TM Valsalva” from the anesthesiologist. The red rubber is then removed and the suture tightened. Saline may be placed in the wound and another Valsalva undertaken while the surgeon carefully inspects for air bubbles. A standard, layered soft-tissue closure without a drain is accomplished. Skin edge eversion can be accomplished with everting subcutaneous sutures.
A chest radiograph is obtained in all patients after rib harvest. In the rare instance of a difficulty, the surgeon may wish to consult the appropriate surgical colleague.
Figure 2. Rib cartilage harvest. Cartilage is typically harvested from the eighth and ninth ribs. A 4 cm to 6 cm incision overlying the eighth rib allows adequate expo- sure (see also Chapter 11, Fig. 6). Dissection proceeds to and then through the rib perichondrium. Dissection around the rib is undertaken subperichondrially; the pleura is typically closely adherent to the perichondrium. With the donor rib completely separated from surround ing soft tissue, the graft is incised and delivered under di rect vision. The surgeon may place a malleable retractor beneath the rib as it is incised.
Harvesting Calvarial Bone
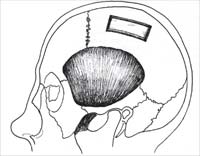
Parietal bone may be harvested (Fig. 3) through a horizontal incision (typically, 4 cm to 6 cm) superior to the temporal line. Typically the nondominant side is chosen. Incision to and through the periosteum, followed by subperiosteal undermining, provides proper exposure. A drill is used to outline the proposed graft (typical graft size, 1 cm to 1.5 cm by 4 cm to 4.5 cm). A trough is drilled through the outer table to the diploe; this allows the proper angle for application of a chisel or powered oscillating saw to harvest the grafts care -fully. Short controlled taps on a sharp osteotome allow increased precision and help de-crease the risk of inner-table penetration and dural tear.
Patients must be cautioned preoperatively of the risk of possible dural tear and possible brain injury. Any dural entry should elicit an immediate neurosurgical consultation.
The donor site can be contoured with hydroxyapatite cement or any other biocompatible bone substitute material. The incision is typically closed in a multilayer fashion.
Figure 3. Calvarial bone harvest. Parietal bone may be harvested through a horizontal incision (typically, 4 cm to 6 cm) superior to the temporal line. Typically the nondominant side is chosen (A). A drill is used to outline the proposed graft (typical graft size, 1 cm to 1.5 cm by 4 cm to 4.5 cm). A trough is drilled through the outer table to the diploe (B, D, E). A chisel or powered oscillating saw may be used to harvest the grafts carefully (C, F—I). Narrower grafts are safer and easier to harvest.
PEARLS
When harvesting auricular cartilage, the surgeon can simplify the dissection by performing local anesthetic injections in the subperichondrial plane. This will act to hydrodissect the flap and allow blunt dissection to elevate the flap.
Special care must be taken to evert the skin edges when performing the skin closure. There will be a tendency for the dissected flap to overlap the skin on the side that was not dissected. Vertical mattress sutures are most effective for aligning the skin edges.
If lateral ear position is a concern, the radix helicis can be left intact to support the auricle and preserve lateral ear position.
Perichondrium can be dissected off the posterior surface of the cartilage and used as tissue for camouflage or to cushion a tip graft.
If small cartilage grafts are needed, the posterior approach can be used to harvest ear cartilage.
If the patient has one ear that protrudes more than the other, then the cartilage should be harvested from that side. If the patient sleeps on one side of the head, then the cartilage should be removed from the contralateral side.
Palpate appropriate-shaped cartilage, and place the incision over the rib to be harvested. In female patients, the incision should be placed in the proximity of the inframammary crease.
Postoperative pain can be minimized by cutting as little muscle as possible when dissecting over the costal cartilage. The muscle fibers can be bluntly dissected to expose the costal cartilage and then retracted to perform the dissection.
Postoperative pain can be significantly decreased by keeping the inferior ribs intact to support the rib cage. With the inferior ribs intact, the patient will have much less pain on inspiration.
Dissect perichondrium off cartilage, taking special care to elevate perichondrium off the inferior surface of the costal cartilage. By leaving the perichondrium intact over the pleura, there will be minimal chance of pneumothorax.
The incision should be closed in multiple layers. After closing the muscle, fascia, and subcutaneous tissues, evert the dermal sutures [4-0 polydioxanone suture (PDS)] to provide prolonged support to the skin edges. The wound will remain everted for several months; however, the scar camouflage will be excellent. Patients should be informed of the temporary excess eversion of the skin edges.
With costal cartilage for grafting, symmetric carving is essential to avoid postoperative warping.
Harvesting Et/inlaid Bone
Avoid resecting ethmoid bone high near the cribriform plate to prevent cerebrospinal fluid leak. Use atraumatic instruments and techniques when removing the bone.
The bone graft can be shaped with a burr.
Harvesting Calvarial Bone
Examine the curvature of the skull to determine the most favorable shape to the bone to harvest the bone graft. The parietal or occipital areas are the most common areas where calvarial bone grafts are harvested.
Create a bone trough down to the diploic layer to allow a curved osteotome to elevate the external table gently off an intact inner table. Generous irrigation is necessary to avoid damage to the bone.
Narrower 1 cm to 2 cm strips of bone are easier to elevate off the inner table.
The bone defect can be filled with a bone substitute material.
REFERENCES
- Tardy ME, Denneny .I, Fritsch MF1. The versatile cartilage autograft in reconstruction of the nose and face. Larvatgoscope 1985;95:523—532.
- Metzinger SE. Boyce RG, Rigby PL, Joseph JJ, Anderson JR. Ethmoid hone sandwich grafting for caudal septal defects. Arch Owl Head Neck Surg 1994:120: 1121—I 125.
- Daniel RK. Rhinoplasty and rib grafts: evolving a flexible operative technique. Mast Reconstr Snug 1992;94: 597—611.
- Wang TD. Aesthetic structural nasal augmentation. Opel- Tech Otolaryngol Head Neck.Snrg 1990.
- Tardy ME. Rhinoplasty: the art and the science. Philadelphia: WB Saunders, 1997.
- Cheney ML, Glicklich RE. The use of calvarial hone in nasal reconstruction. Arch Ourlarvt , gol Head Neck Surg 1995;121:643—648.