Introduction
Nasal airway obstruction (NAO) is defined as the sensation of insufficient airflow or difficulty breathing through the nose. A common problem in otolaryngology, NAO affects approximately 20 million Americans with a significant impact on quality of life (QOL).1-4 NAO can be caused by infectious, allergic, vasomotor, or structural abnormalities, with etiology impacting the optimal treatment option which can also be treated by an ENT doctor.5 Given the high prevalence of this disease, it is important to consider how objective measures can be utilized to evaluate the severity or etiology of obstruction, help drive treatment, or assess outcomes after intervention. The objective measures that will be discussed include the Peak Nasal Inspiratory Flow Meter (PNIF), rhinomanometry, acoustic rhinometry and image-based volumetry, and computational fluid dynamic (CFD) modeling. The goal will be to highlight the clinical utility of each objective measure and to discuss future directions to improved upon the devices that are currently available.
Peak Nasal Inspiratory Flow
PNIF is a noninvasive, inexpensive, rapid, portable, and easy-to-use objective measure that directly measures nasal airflow during maximal inspiration (Figure 1).6,7 Despite its ease of use, PNIF is effort dependent, and therefore can only be applied to patients with adequate pulmonary function. Ottaviano et al. found that PNIF values in healthy elderly individuals are lower than those in younger healthy individuals, demonstrating the need for normative data for this technique.8
Applications of PNIF are currently being studied. Chin et al. found that a lack of improvement in PNIF of at least 20L/min or 20% may be associated with a persistant structural obstruction.9 PNIF has been used to evaluate postoperative outcomes from radiofrequency ablation of turbinates and to correlate with computed tomography (CT)-based, cross-sectional area measurements of nasal patency.10

However, correlations with the scores from the validated Nasal Obstruction Symptom Evaluation (NOSE) scale have been mixed.11-14 Tsounis et al. showed a correlation between PNIF and patient-reported outcome measures (PROM) when the NOSE scale is used, but we found only a weak correlation between PNIF and NOSE scores because there is a large variance in PNIF scores between patients.13,14 We, therefore, do not feel that PNIF should be used for the diagnosis of the severity of nasal obstruction.
However, we do recommend the use of PNIF in the clinical management of patients with nasal obstruction. We collect three PNIF measures and record all three measures in the electonic medical record at the pre-operative visit and at each post-operative visit. The highest value is the value used to compare results between visits. The PNIF measurements are useful to determine improvement in nasal airflow after surgical management, so we recommend using the increase in PNIF values as an indicator of improvement in nasal airflow. Clinically, we have found that PNIF is most useful in patients with presistent symptoms of nasal obstruction post-operatively despite having a normal clinical exam. When patients have significant improvement in PNIF values after surgery, no anatomic signs of obstruction, but continued symptoms of nasal obstruction, PNIF can provide the patient and the provider with confidence that the nasal airway has structurally improved and that revision surgery is not the next best step. Instead, this offers the reassurance to wait and allow additional time to heal. Often these patients will have improved symptoms by 6-12 months.
Rhinomanometry
Rhinomanometry measures dynamic pressure and flow through the nose during inspiration and expiration to assess nasal resistance and airflow velocity, markers of nasal patency. In contrast to easy-to-use PNIF, rhinomanometry requires extensive resources, including temperature and humidity control, efficient mask seal, patient cooperation, and dedicated equipment, staff, and space.15 Similar to PNIF, active anterior rhinomanometry, more commonly performed than the passive approach because of its use of the patient’s own respiration as the flow source, depends on effort. Correlations of active anterior rhinomanometry with subjective measures have been mixed, with some results showing poor correlation despite normative data established by a meta-analysis.16,17
Beyond passive and active rhinomanometry, four-phase rhinomanometry has higher resolution by measuring ascending and descending components of inspiration and expiration over time and with reports of increased consistency of readings (Figures 2,3).18,19 A meta-analysis showed correlation of visual analog scale with logarithmic transformations of measured effective resistance and vertex resistance.18 Despite the improvements of four-phase rhinomanometry compared to the standard approach, further validation is needed for extensive implementation of this objective measure. Still, it has promise to provide a valid measure of nasal airflow and nasal valve dynamic collapse. If space and clinical support are available, then this does have clinical utility. The exam takes about 20 minutes and is most efficiently integrated into clinical practice if a dedicated person and room is available for testing. We have found that this objective measure is well-received by patients especially those with persistent symptoms as the exam allows patients and the examiner to see their nasal airflow with normal inspiration and expiration in real-time.
Acoustic Rhinometry and Image-Based Volumetry
Acoustic rhinometry utilizes reflected acoustic waves to measure cross-sectional areas and volumes along the nasal passage.15 Inconsistencies have been reported with regards to the region assessed, as anterior cavity measurement is more accurate than posterior cavity measurement in comparison studies with imaging.20 Furthermore, it is important to note that acoustic rhinometry offers a static measurement of a dynamic process. In addition, there may not be a correlation between suggestive symptoms of NAO and acoustic rhinometry measurements of nasal volume. Toyserkani et al. showed that 157 patients who underwent septoplasty had no correlation between NOSE scale scores and acoustic rhinometry results preoperatively, at 3 months postoperatively, or at 11-year follow-up.21
Similar to acoustic rhinometry, CT- or magnetic resonance imaging (MRI)-based volumetry uses cross-sectional areas measured on imaging determine nasal passage volume.15 Manual or automatic algorithms are also needed to outline the nasal cavity. Although Menger et al. revealed that automated, CT-derived minimal cross-sectional area and PNIF correlated better
with NOSE scale scores than did acoustic rhinometry-derived minimal cross-sectional area, automated area calculations can be inaccurate since they are a static measurement and depend on image resolution and appropriate thresholding.12 Tomazic et al. showed that CT- and MRI-based volumetry do not correlate with improved NOSE scores after radiofrequency ablation of the inferior turbinates.22
Because subjective measures of NAO do not appear to correlate with voluemtric analysis using acoustic rhinometry or CT and MRI imaging, nasal volume may only be one aspect that results in the sensation of obstruction.23,24 Thus, additional measures are needing to evaluate NAO and determine its cause. Therefore, we do not currently recommend the clinical use of acoustic rhinometry or image-based volumetry
This is a small portable unit that requires a laptop or desktop computer and disposable masks.
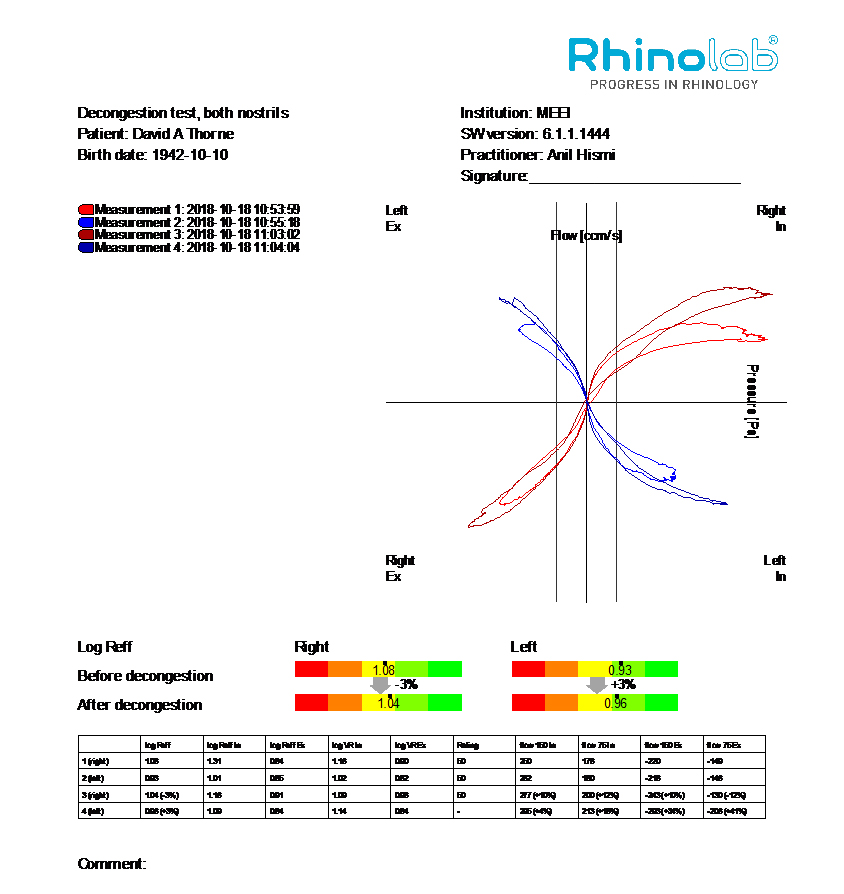
Demonstration of the standard output for a patient undergoing four-phase rhinomanometry showing nasal airflow during inspiration and expiration before and after nasal decongestion.
Computational Fluid Dynamics and Mucosal Cooling
CFD has emerged as a new objective measure, which utilizes an engineering technique of fluid-flow simulation to examine nasal airflow and resistance.15 The current body of literature suggests that variables in CFD correlate with subjective sensation of NAO. Moderate correlations were revealed between patient symptoms and airflow, heat flux, and unilateral resistance.25 Peak mucosal cooling, measured by CFD, was demonstrated to correlate with nasal patency ratings by visual analog scale. CFD-stimulated nasal resistance also correlated well with rhinomanometry-measured resistance.26 An increase in postoperative mucosal cooling correlated with increased subjective patency, measured by the NOSE scale.27 In addition, reduced middle airflow in the nasal passage correlated with the subjective sensation of obstruction, which may be attributed to reduced mucosal cooling from diverted flow secondary to caudal septal deviation.28 The utility of CFD continues to be studied by our group and others around the world. Additional research in this area will allow surgeons to perform targeted surgical approaches, understand the anatomic reasons for surgical failures, and identify causes of persistent symptoms nasal obstruction in patients without reduced airflow but with reduced perception of nasal airflow.
Patient Reported Outcomes Measures
Applying subjective measures pre- and post-operatively can add valuable insight alone and when used with the objective measures delineated above. Commonly used patient reported outcome measures (PROMs) include the Nasal Obstruction Symptom Evaluation (NOSE) scale, a validated QOL instrument for patients with NAO with an effective minimal clinically important difference (MCID) of 30.0 points.29,30 A validated, multi-modular PROM, the FACE-Q scale measures a patient’s perception of nasal appearance and its impact on social functioning.31 Although MCIDs for FACE-Q scores have yet to be determined in the literature, this value has been approximated in the literature using one-half of the mean baseline standard deviation.32,33 In addition, the 10-Item Standardized Cosmesis and Health Nasal Outcomes Survey (SCHNOS) is a recently introduced, validated questionnaire that evaluates functional and cosmetic outcomes of patients undergoing rhinoplasty.34
Conclusion
NAO is a common problem in otolaryngology with significant effects on QOL. PNIF, four-phase rhinomanometry, and CFD have arisen as objective measures to study NAO and associate interventions with the highest potential utility. These measures continue to be studied and should be adjunctive, along with subjective PROMs, to assess the severity or etiology of obstruction, help direct treatment, and evaluate outcomes.
References
- Chandra RK, Kern RC, Cutler JL, Welch KC, Russell PT. REMODEL larger cohort with long-term outcomes and meta-analysis of standalone balloon dilation studies. The Laryngoscope. 2016;126(1):44-50.
- Rhee JS, Poetker DM, Smith TL, Bustillo A, Burzynski M, Davis RE. Nasal valve surgery improves disease-specific quality of life. The Laryngoscope. 2005;115(3):437-440.
- Gadkaree SK, Fuller JC, Justicz NS, et al. A Comparative Health Utility Value Analysis of Outcomes for Patients Following Septorhinoplasty With Previous Nasal Surgery. JAMA facial plastic surgery. 2019.
- Gadkaree SK, Fuller JC, Justicz NS, et al. Health Utility Values as an Outcome Measure in Patients Undergoing Functional Septorhinoplasty. JAMA facial plastic surgery. 2019.
- Rhee JS,Weaver EM, Park SS, et al. Clinical consensus statement: diagnosis and management of nasal valve compromise. Otolaryngol Head Neck Surg. 2010;143(1):48-59.
- Starling-Schwanz R, Peake HL, Salome CM, et al. Repeatability of peak nasal inspiratory flow measurements and utility for assessing the severity of rhinitis. Allergy. 2005;60(6):795-800.
- Kjaergaard T, Cvancarova M, Steinsv.g SK. Relation of nasal air flow to nasal cavity dimensions. Arch Otolaryngol Head Neck Surg. 2009;135(6):565-570.
- Ottaviano G, Lund VJ, Nardello E, et al. Peak nasal inspiratory flow: a useful and handy tool for the diagnosis of nasal obstruction in the elderly. Eur Arch Otorhinolaryngol. 2014;271(9):2427-2431.
- Chin D, Marcells G, Malek J, et al. Nasal peak inspiratory flow (NPIF) as a diagnostic tool for differentiating decongestable from structural nasal obstruction. Rhinology. 2014;52(2):116-121.
- Andrews PJ, Choudhury N, Takhar A, Poirrier AL, Jacques T, Randhawa PS. The need for an objective measure in septorhinoplasty surgery: are we any closer to finding an answer? Clin Otolaryngol. 2015;40(6):698-703.
- Koleli H, Paltura C, Sahin-Yilmaz A, Topak M,Develioglu ON, Kulek.i M. Peak nasal inspiratoryflowmetry for selection of patients forradiofrequency ablation of turbinates. Ann OtolRhinol Laryngol. 2014;123(7):457-460.
- Menger DJ, Swart KM, Nolst Trenit. GJ, Georgalas C, Grolman W. Surgery of the external nasal valve: the correlation between subjective and objective measurements. Clin Otolaryngol. 2014;39(3):150-155.
- Tsounis M, Swart KM, Georgalas C, Markou K, Menger DJ. The clinical value of peak nasal inspiratory flow, peak oral inspiratory flow, and the nasal patency index. Laryngoscope. 2014;124(12):2665-2669.
- Fuller JC, Bernstein CH, Levesque PA, Lindsay RW. Peak Nasal Inspiratory Flow as an Objective Measure of Nasal Obstruction and Functional Septorhinoplasty Outcomes. JAMA Facial Plastic Surgery. 2019;20(2):175-176.
- Mohan S, Fuller JC, Ford SF, Lindsay RW. Diagnostic and Therapeutic Management of Nasal Airway Obstruction Advances in Diagnosis and Treatment. JAMA Facial Plastic Surgery. 2018;20(5):409-418.
- Sahin-Yilmaz A, Oysu ., Devecioglu I, Demir K, Corey JP. Prediction of outcome of radiofrequency ablation of the inferior turbinates. Int Forum Allergy Rhinol. 2014;4(6):470-474.
- Merkle J, Kohlhas L, Zadoyan G, M.sges R, Hellmich M. Rhinomanometric reference intervals for normal total nasal airflow resistance. Rhinology. 2014;52(4):292-299.
- Vogt K,Wernecke KD, Behrbohm H, et al. Four-phase rhinomanometry: a multicentric retrospective analysis of 36 563 clinical measurements. Eur Arch Otorhinolaryngol. 2016;273:1185-1198.
- Vogt K, Zhang L. Airway assessment by four-phase rhinomanometry in septal surgery. Curr Opin Otolaryngol Head Neck Surg. 2012;20(1):33-39.
- Numminen J, Dastidar P, Heinonen T, Karhuketo T, Rautiainen M. Reliability of acoustic rhinometry. Respir Med. 2003;97(4):421-427.
- Toyserkani NM, Frisch T, Von Buchwald C. Postoperative improvement in acoustic rhinometry measurements after septoplasty correlates with long-term satisfaction. Rhinology. 2013;51(2):171-175.
- Tomazic PV, Gerstenberger C, Rant B, et al. Subjective and objective parameters in the evaluation of radiofrequency ablation of the inferior turbinate do not correlate: a pilot study. Ear Nose Throat J. 2016;95(8):344-352.
- Haavisto LE, Sipil. JI. Acoustic rhinometry, rhinomanometry and visual analogue scale before and after septal surgery: a prospective 10-year follow-up. Clin Otolaryngol. 2013;38(1):23-29.
- Edizer DT, Erisir F, Alimoglu Y, et al. Nasal obstruction following septorhinoplasty: how well does acoustic rhinometry work? Eur Arch Otorhinolaryngol. 2013;270(2):609-613.
- Kimbell JS, Frank DO, Laud P, Garcia GJ, Rhee JS. Changes in nasal airflow and heat transfer correlate with symptom improvement after surgery for nasal obstruction. J Biomech. 2013;46(15):2634-2643.
- Zhao K, Jiang J, Blacker K, et al. Regional peak mucosal cooling predicts the perception of nasal patency. Laryngoscope. 2014;124(3):589-595.
- Sullivan CD, Garcia GJM, Frank-Ito DO, Kimbell JS, Rhee JS. Perception of better nasal patency correlates with increased mucosal cooling after surgery for nasal obstruction. Otolaryngol Head Neck Surg. 2014;150(1):139-147.
- Casey KP, Borojeni AA, Koenig LJ, Rhee JS, Garcia GJ. Correlation between subjective nasal patency and intranasal airflow distribution. Otolaryngol Head Neck Surg. 2017;156(4):741-750.
- Stewart MG, Witsell DL, Smith TL,Weaver EM, Yueh B, HannleyMT. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngology Head Neck Surgery. 2004;130(2):157-163.
- Rhee JS, Sullivan CD, Frank DO, Kimbell JS, Garcia GJ. A systematic review of patient-reported nasal obstruction scores: defining normative and symptomatic ranges in surgical patients. JAMA Facial Plast Surgery. 2014;16(3):219-225.
- Klassen AF, Cano SJ, East CA, et al. Development and Psychometric Evaluation of the FACE-Q Scales for Patients Undergoing Rhinoplasty. JAMA facial plastic surgery. 2016;18(1):27-35.
- Fuller JC, Levesque PA, Lindsay RW. Assessment of the EuroQol 5-Dimension Questionnaire for Detection of Clinically Significant Global Health-Related Quality-of-Life Improvement Following Functional Septorhinoplasty. JAMA facial plastic surgery. 2017;19(2):95-100.
- Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Medical care. 2003;41(5):582-592.
- Moubayed SP, Ioannidis JPA, Saltychev M, Most SP. The 10-Item Standardized Cosmesis and Health Nasal Outcomes Survey (SCHNOS) for Functional and Cosmetic Rhinoplasty. JAMA Facial Plastic Surgery. 2018;20(1):37‐42. doi:10.1001/jamafacial.2017.1083
