It is important that the rhinoplasty surgeon pay attention to both form and function. In other words, your nose should look great, but it also has to work!
Dr. Becker is double board certified in ENT (Otolaryngology) and Facial Plastic Surgery. This means that his training and experience focus on both the aesthetic and functional aspects of rhinoplasty.
When you see Dr. Becker, he will examine your nose inside and out. If you have a breathing problem, he will identify the cause. If you are interested, he will be able to show you the reason for your breathing problem using digital video-endoscopy.
If you do not have a breathing problem, but you want a smaller nose, Dr. Becker will examine the inside of your nose to make sure that all steps are taken to be sure that after surgery, your smaller nose will still work!
Dr. Becker has a national and international reputation in cosmetic and functional nasal surgery. Since 1998, he has been the Course Director for the PENN Rhinoplasty Course Aesthetic and Functional Rhinoplasty. This course attracts surgeons from across the country and around the world. In this course, and wherever he lectures, Dr. Becker emphasizes the importance of both aesthetics and function.
Nose Form and Function, Page 2
Most recently, he lectured plastic surgeons at the prestigious New York City conference, “Advances in Aesthetic Plastic Surgery: The Cutting Edge V.”. A transcript of Dr. Becker’s lecture on the subject, along with the pictorial slides, is shown below:
Thank you for the privilege of speaking to you today on the subject of Functional Considerations in Rhinoplasty and The Role of Pre-operative Endoscopy in Functional Rhinoplasty.
Amongst physician specialists who take care of nasal breathing problems, nasal endoscopy (examining the nose using a special telescope) is the standard of care in the evaluation of patients with nasal blockage. Unfortunately, a significant number of rhinoplasty surgeons do not routinely perform this evaluation. We will show you today that those doctors may be missing important problems causing nasal obstruction. It is no surprise that in these cases a number of these patients have persistent nasal blockage even after rhinoplasty. We will show you examples of patients who had problems causing nasal blockage that could only be discovered by endoscopic exam or subsequent CT scan. And, we will discuss the treatment of these problems as well.
As we discuss the causes of nasal breathing problems in patients seeking rhinoplasty, my question to the audience today is this:
If a patient has nasal obstruction, should the fact that they are seeking rhinoplasty change the standard of care? In other words, shouldn’t we perform a nasal endoscopy on every patient with nasal obstruction to be sure we find the cause? How do you justify NOT doing an endoscopy on such a patient just because they are having a rhinoplasty as well?
Nose Form and Function, Page 3
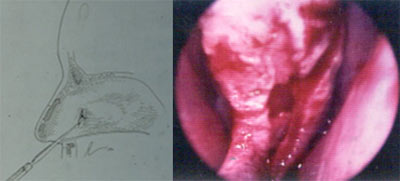
For those of you who are not familiar with nasal endoscopy, it is a simple officeprocedure in which a telescope is inserted into the nose to allow a close lookat the nasal cavity, all the way back to the eustachian tubes. (Of course, a numbing and decongesting agent is applied to the nose first so that this can be performed painlessly and quickly.
The differential diagnosis for nasal obstruction includes allergic rhinitis, rhinosinusitis, deviated septum, nasal valve collapse, nasal polyps, adenoid hypertrophy, rhinitis medicamentosa, choanal atresia, nasal tumors, and others.
Some of these problems occur quite commonly. In my practice, the most common causes of nasal obstruction include a deviated septum, also allergies and sinusitis. We’ll talk more about these common problems a little later.
Nose Form and Function, Page 4
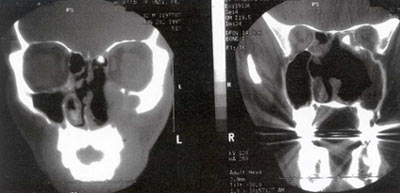
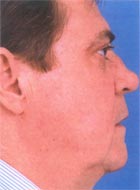
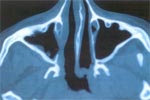
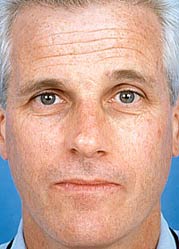
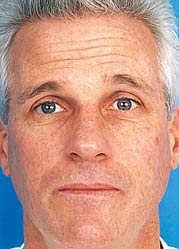
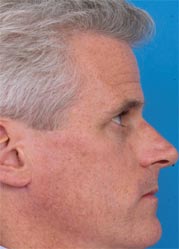
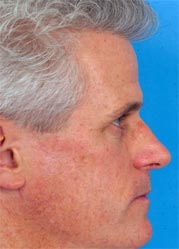
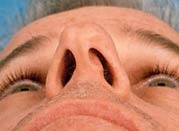
The patient shown in these photographs presented to my office with nasal obstruction. As a secondary concern he was interested in rhinoplasty, specifically in improving the appearance of his twisted nasal tip.
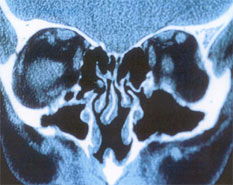
He had been to other doctors who had told him that he had a deviated septum. However, when I examined him I couldn’t see all the way to the back of the nose with anendoscope, and so I obtained a CT scan, shown here. As you can see, this gentlemen had a benign but extremely large tumor. Fortunately, this bony tumor was benign, and we have been able to treat him successfully.
While this kind of problem is rare, it highlights the fact that there are a lot of different causes of nasal obstruction. This fact should not be ignored just because a patient wants a rhinoplasty.
As we go through this lecture we are showing you some of the uncommon things that we have seen from time to time over the years. Of course, we see the very common things – like a deviated septum – much more frequently. Still, it is important to realize that these rare problems can show up in any doctor’s office and that while they are uncommon, they definitely occur.
It is our job as doctors of the nose and as rhinoplasty surgeons to identify the common and the uncommon causes of nasal obstruction. To accomplish this, we must perform a thorough examination including endoscopy. If a patient comes in to see us for a rhinoplasty to improve their appearance and also to improve their nasal breathing, it is important to identify all the causes of nasal obstruction so that we give them the best possible result.
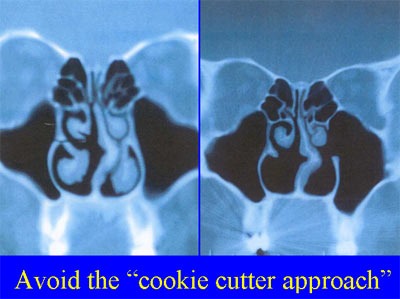
One of the problems that we see – more often that we would like – is that some surgeons seem to assume that if a patient complains of nasal obstruction they must have large inferior turbinates or a deviated septum. This leads to an “assembly-line” or “by-the-numbers” rhinoplasty approach that we strongly condemn.
Nose Form and Function, Page 5
The X-ray shown above belongs to a patient who had nasal obstruction on the left side only. A plastic surgeon performed bilateral inferior turbinectomies and did not do a septoplasty. Now, the patient has atrophic rhinitis and bitterly complains of nasal obstruction on both sides. (For those of you who are not familiar, atrophic rhinitis is a condition in which the nose does not have enough mucous lining. Taking out the inferior turbinates can lead to a situation where the nose is too dry and the patient loses the sensation of airflow. In this situation, the patient physically has a very wide nasal airway but cannot feel the air passing through, so they complain bitterly of nasal blockage. This is an extremely debilitating problem for which there is no good treatment.) This patient illustrates clearly the reason that we condemn a “by-the-numbers” rhinoplasty. We advocate a thoughtful approach in which a careful examination allows proper diagnosis and is followed by proper treatment designed to address the specific cause of nasal obstruction.
To provide some perspective on this, our team looked back on all patients that I operated on over a time period of approximately one year. We looked at patients who had two requests: treatment of nasal obstruction and improvement in nasal appearance (i.e., cosmetic rhinoplasty). Therefore, all patients whose nasal breathing was good – patients requesting only cosmetic rhinoplasty – were excluded.
We recorded our findings from looking inside the nose with a headlight (anterior rhinoscopy) and recorded additional findings on nasal endoscopy. In this study we looked at 95 patients, 83 of whom had primary rhinoplasties and 12 of whom had revision rhinoplasties. On an external exam and anterior rhinoscopy, we were able to identify a deviated septum, nasal valve compromise, and inferior turbinate hypertrophy. Additional findings that we discovered on nasal endoscopy included obstructing adenoids, large middle turbinates with concha bullosa, choanalstenosis, nasal polyps, and chronic sinusitis.
Nose Form and Function, Page 6
It is important to note that additional surgical therapy was undertaken in 28 of 93 patients due to findings on endoscopy (and at times CT scan):
Partial middle turbinectomy with resection of a concha bullosa was undertaken in 9 patients. Endoscopic sinus surgery was undertaken at the same time as rhinoplasty in 13 patients. 2 patients required adenoidectomy. Choanal stenosis occurred in 1 patient. 3 patients had persisting posterior septal deviation after having had septoplasty elsewhere.
In the remaining 20 minutes or so I would like to go through some patient examples that highlight some of these things that we discovered on endoscopy. I think that these cases will be illuminating.
The patient shown below told us that she had been to approximately 10 prior surgeons seeking treatment of her nasal obstruction and improvement in her nasal appearance. I asked if she had undergone a nasal endoscopy and she told me that no doctor had looked in her nose with an endoscope. In her case, endoscopy revealed extremely large adenoids. I was able to make the diagnosis of adenoid hypertrophy.
In the worst case scenario – if she had had rhinoplasty surgery and had not had her adenoidectomy at the same time (in other words if a surgeon had overlooked this problem) – then she would have had persisting nasal obstruction. Eventually one might imagine that a doctor would have finally found this problem and she would have gone back to surgery (for a second operation) for an adenoidectomy. In the case of obstructing adenoids, this unnecessary second trip to the operating room can be avoided by a careful examination with endoscopy.
Nose Form and Function, Page 7
This patient had broken his nose and had had a repair of his septum (i.e. a septoplasty). However a septal perforation had resulted and the patient had a persisting deviation of his septum behind the perforation, which as you all know can be a very difficult problem. We were able to undertake this septorhinoplasty using an endoscopic septoplasty technique. We have described an endoscopic technique in this situation in the literature (Operative Techniques in Otolaryngology vol 12 no 2, 2001). Using an endoscope the surgeon can look directly at the part of the septum where there is deviation and just correct that, leaving everything else undisturbed. This is in contrast to a more traditional septoplasty in which the entire septum is exposed. The endoscopic septoplasty is particularly useful when there is persistent obstruction further in the back of the nose after previous septoplasty, and in these revision cases the lining of the septum is very densely adherent and more difficult to elevate. Therefore, rather than undertake this very trying and challenging dissection that risks septal perforation, it is much more appropriate – and easier – to undertake an endoscopic septoplasty to bypass the hazardous area and go directly to the deviated site.
I have had numerous patients present to me for revision septoplasty who were worried about a septal perforation because they have been to other doctors who have recommended revision septoplasty and told them that they would most certainly have a septal perforation. However, using the endoscopic technique in these cases, we have never had this problem.
Nose Form and Function, Page 8
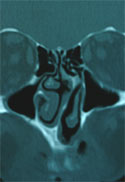
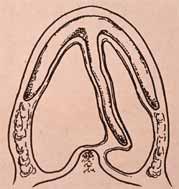
This next patient has two problems. She has a saddle nose deformity (also known as a “boxers nose” deformity) that is contributing to nasal obstruction and to an unpleasant nasal appearance. Many surgeons would simply assume that this was the cause of her nasal breathing problems – in fact two other surgeons she saw before me told her that!
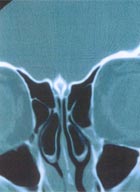
Looking in her nose I with an endoscope, I suspected another problem and obtained a CT scan. Looking at this CT scan you can see that her inferior turbinates are small and her septum is straight – but she has two aerated middle turbinates (called concha bullosa) and these are crowding the nasal cavity and causing her nasal obstruction. By resecting the side portion of each concha bullosa, we make this space available for nasal breathing and significantly improve her nasal airway. We find this problem in a significant number of patients with nasal obstruction.
Nose Form and Function, Page 9
A wise doctor once said that you only find a problem if you look for it, and you only look for it if you know exists. We know these kinds of things cause nasal obstruction and you can only find them by being knowledgable and performing a careful and complete examination.
Here is another patient who you might assume has nasal blockage because of a saddle nose deformity. However his blockage is only left sided, and when we do an endoscopy we see that he has a post-traumatic, posterior choanalstenosis that was easily identified and treated with endoscopic techniques.
Nose Form and Function, Page 10
We have talked about the turbinates and in some cases the lower or inferior turbinates are the problem as seen here. Sometimes they are the problem, but the treatment must be very conservative for the reasons that we outlined above. What we would like to do is called radiofrequency reduction often known as Somnoplasty or Coblation. When done properly, this preserves the turbinates but simply shrinks overlarge turbinates so they are closer to normal size.



Before & After

Turbinates
Nose Form and Function, Page 11
We strongly oppose aggressively resecting inferior turbinate tissue as we believe that it is very important tissue for nasal breathing. It has nerve fibers that sense airflow, and it also provides resistance to nasal breathing, which seems to be important. In the absence of these two factors, atrophic rhinitis can occur.
Many patients who have nasal obstruction have sinusitis. It is important to remind you that the most common presenting symptom of sinusitis is nasal obstruction. With this in mind, a large number of patients who have nasal obstruction have chronic sinusitis and this should be identified and treated. Most commonly this can be treated with medical therapy; however, at times surgery may be of benefit.
This CT scan belongs to a patient who has severe nasal blockage from her sinuses, perhaps more than most. Endoscopic exam in this patient and others like her will show significant swelling of the mucous membrane lining and also will show thick abnormal discharge.
At times, pollops are discovered in patients who have sinusitis, as shown here :
Nose Form and Function, Page 12
Sinus surgery can be safely performed at the same time as rhinoplasty. If the surgeon is skillful in the performance of both of these procedures, then this can be undertaken by a single surgeon, but if not, there is certainly a skillful surgeon in your area who can do this for you.
This combined surgery can compose as much as 18%-20% of a surgeon’s practice (personal communication from Dr. Paul Toffel). In my practice, approximately 12% of patients who undergo sinus surgery also undergo rhinoplasty. For those of you who are interested, this information is more fully detailed in the journal, Aesthetic Surgery, where Dr. Kennedy and I wrote an article entitled “Indications forEndoscopic Sinus Surgery in Patients Seeking Aesthetic Rhinoplasty.”
We often see patients who have had previous rhinoplasty, and if – unfortunately – they have had too much cartilage taken out from the nose they can have nasal collapse.
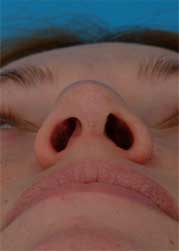
As shown here, when this patient breathes in through her nose has complete collapse of her nostrils. This is treated by restoring structural support to her nose. This can be done by a very simple outpatient procedure under sedation anesthesia, and you can see that on these pictures that the strength of her nose is restored.
A few years ago, we published an article entitled “Clinical Study of Alar Anatomy and Surgery of the Alar Base.” In this report we examined the features of the noses of 100 randomly selected patients. What was important here is that the nostril is of “normal” thickness and strength in about 73% of the patients but was thin and weak in 20%. In other words, in this particular sampling 20% of the patients have thin, weak nostril margins. It is important for the surgeon to identify these patients pre-operatively, and then you must be especially careful that you don’t resect too much. You would probably want to resect a little bit less than usual in these patients to avoid this sort of problem, because this can result not only in nasal obstruction but also in an unsightly cosmetic appearance.
Nose Form and Function, Page 13
Now all rhinoplasty surgeons are familiar with the internal nasal valve, which is considered the narrowest portion of the nasal airway. The nasal valve is defined by an angle of 10-15 degrees formed by the lower border of the upper lateral cartilage where it joins with the septum. Underneath this angle is the more important nasal valve area, which is the cross sectional surface area beneath the nasal valve angle. The nasal valve area can be blocked by enlargement of the inferior turbinate, deviation of the septum, and other structural problems.
At times spreader grafts (also known as “spacer grafts”) may be placed to widen the middle portion of the nose and increase the internal nasal valve angle and the internal nasal valve area. Also, these can be placed asymmetrically to improve any cosmetic deviation of the nose in this region.
Also, when a large nose is reduced, it is important to realize that the cross sectional area in this region will be narrowed, and so counter-measures must be undertaken to preserve the cross sectional area at this critical location. So when a patient – such as this one – has a very large nose to begin with, we place spreader grafts during reduction rhinoplasty to maintain a good nasal airway. Otherwise the patient may have a nice looking nose but he may have a nose that doesn’t work!
So these are some of the subtle technical details that are important to having the best chance of functional and cosmetic success.
Nose Form and Function, Page 14
I want to take some time to talk about a specific problem of the septum, a deviation of the caudal (or front part) of the septum. Deviation of the septum at this location, at the front near the nostril) can block nasal breathing and also cause an unsightly appearance. Surgeons over the years have found this to be a relatively difficult problem to treat, and there are a lot of different solutions that have been proposed. Dr. Norman Pastorek and I have recently published an article in Archives of Facial Plastic Surgery entitled “Treating the Caudal Septum.” In this article, we proposed a very simple technique that may be called the “door-stop” technique. We take advantage of the natural anatomy and are able to flip the cartilage to the opposite side of the nose, securing it in such a way that it straightened very reliably. Since I learned this technique, I have also passed it on to others who have also reported to me great success with this technique. So, I share it with you today as it can simplify things a great deal and may allow you to treat your patients with greater success.
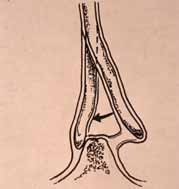
Deviation of the septum
Nose Form and Function, Page 15
And here is another patient who had treatment of a similar problem using these same techniques. It is a very nice technique and I really do recommend it to you highly.

Nose Form and Function, Page 16
So, as we conclude our discussion of the various causes of nasal obstruction in rhinoplasty patients, I would like to repeat my question to you at the beginning: Is it enough to examine the nose with simply the naked eye? Or are we obligated to evaluate all the way back to the nasopharynx in a patient complaining of nasal obstruction?
The simple fact is that nasal endoscopy is a very easy office procedure that has virtually no complications to speak of and provides a great service to our patients. Really, it would be difficult for me to imagine why a physician might resist performing nasal endoscopy on these patients. Unfortunately there are still many surgeons who do not perform endoscopy on this group of patients, and I hope that this lecture has helped to persuade a few to provide this important service to their patients. Thank you very much.