Intro:
Few operations in the entire field of plastic surgery are as challenging as revising a nasal tip that has been previously operated on. Achieving optimal aesthetics from distorted remnants of delicate cartilages may seem difficult, but to also contend with the vagaries of wound contracture, the frequent need to use cartilage from a distant site, the prominent and central position of the nasal tip in facial aesthetics, and the hopes and expectations of a patient that has already been disillusioned and/or traumatized, make this procedure particularly demanding. Revision tip surgery requires that we employ all that we have learned and then, beyond our teachings; some of what we simply “feel”. Perhaps it is for this reason that restoring a nasal tip is so seductive to many of us in the field of plastic surgery.
Anatomy:
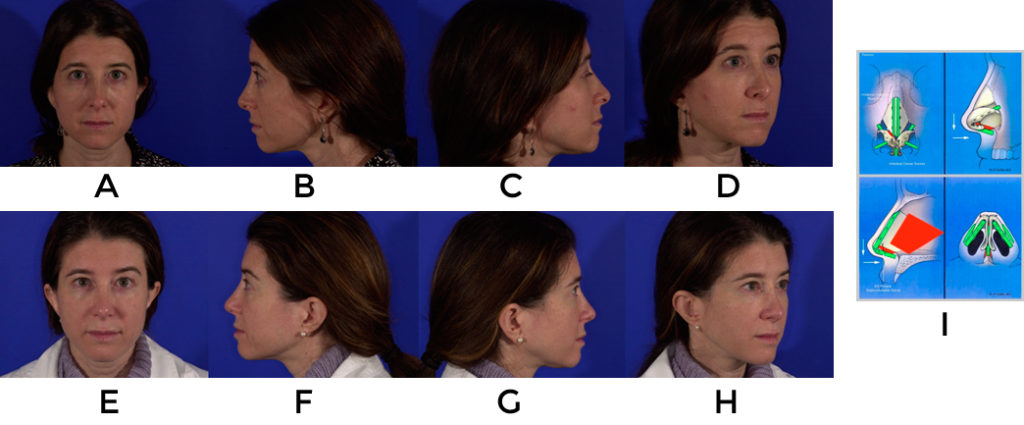
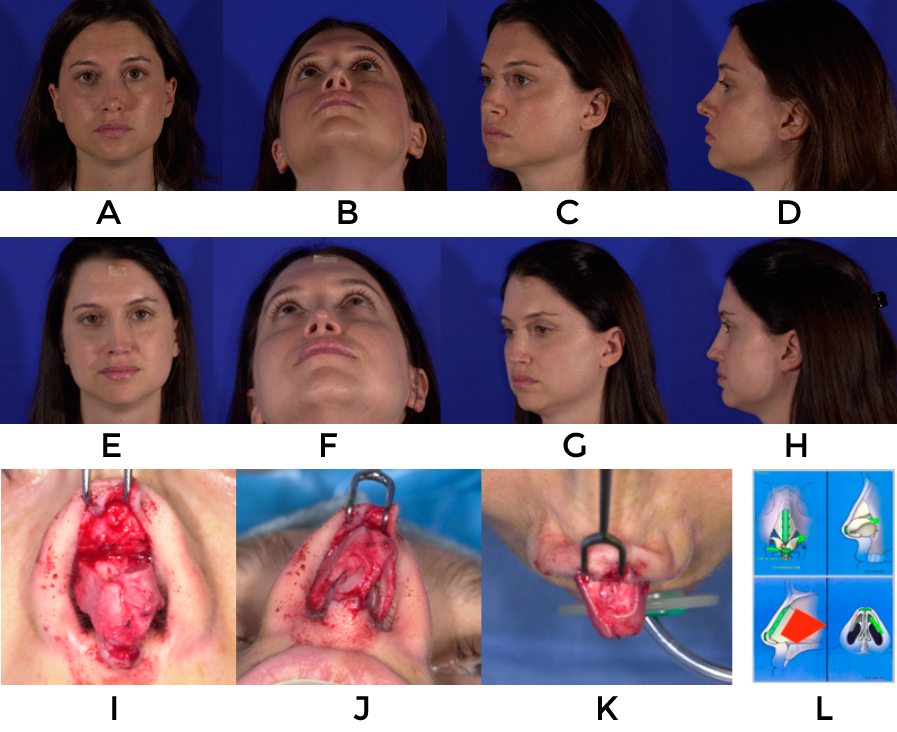
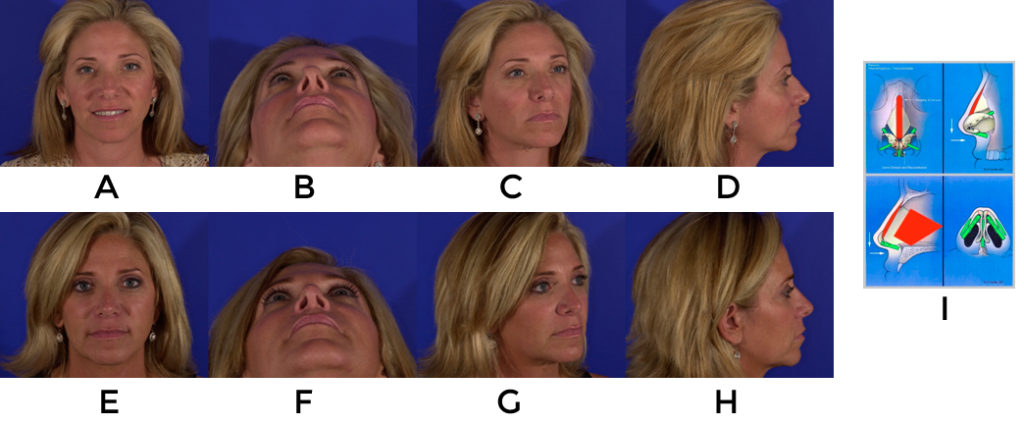
A prime requisite for revision surgery of the nasal tip is a thorough understanding of normal anatomy and the potential variations that exist (figure 1). Only with such knowledge is it possible to sift through the wreckage that may exist from prior surgery and identify the underlying constituent parts in an effort to reconstruct things on an anatomic basis (fig 2,3). Even in cases where reestablishment of normal architecture is not required, such as creating an improved silhouette, it is vital to understand what ‘normal’ anatomy should be in order to simulate it (Fig 4)
Consultation:
Pre-operative consultation begins with the patients own words about why they are there and what is bothering them. Try to have them prioritize their issues and be specific about what changes they would like to enact. Revision rhinoplasty patients will usually provide a history of multiple prior surgeries and what occurred with each procedure. It is helpful to decipher why the patient went ahead with each of the prior operations and why they felt the procedures failed. Copies of prior operative reports are helpful but just as often as not, they are incomplete or inaccurate. Questions regarding nasal function such as whistling, crusting, bleeding, rhinitis and obstruction should be asked. Previous trauma, cocaine use, decongestant use as well as whether the patient uses any devices such as breathe-rite strips or nasal cones also provides helpful information.
Interaction and discussion with the patient during the consultation provide an opportunity to assess that individual’s psychologic state. Rhinoplasty patients are often their own worst enemies. Unrealistic expectations with great attention to detail and a disproportionate amount of angst over small irregularities tend to typify patients who have undergone multiple nasal surgeries. If a patient is very flattering or complementary during the visit it should alert you to potential problems. Patients that berate their prior surgeons, exhibit significant anger or that speak of becoming reclusive as a result of their prior surgical result should also be considered carefully. Body dysmorphic disorder is a potential pitfall that is difficult to identify and suspicion from the surgeon or any members of the surgeon’s staff should warrant an evaluation from a specialist. When indicated, the patients are told of the surgeon’s concerns and the reason for the second consultation as clear lines of communication are of supreme importance when dealing with a demanding, detail-oriented patient.
Examination:
The nature of a revision nasal surgery is such that a very detailed physical examination cannot be overemphasized. With enough experience the accomplished surgeon should begin to see through the skin and be able to decipher what has occurred to the nascent cartilages to create the particular deformities.
In addition to “seeing through the skin” with one’s touch, it is important to view the nose from many different angles including from above the patient in order to fully appreciate the subtle asymmetries, curves and high points that may exist. Gently pulling on the ala and tip can indicate the amount of laxity in the vestibular skin which is important when lengthening a nose. Placement of the caudal end of the septum between the thumb and forefinger in order to determine its position also provides useful information. A proper intranasal exam must be stressed as without correcting for webbing, synechia or valve stenosis, surgery may be unsuccessful. It is helpful to watch the dynamics of the side walls as the patient inspires. The use of a cotton swab, as done with a Modified Cottle maneuver, to support small areas of the vestibule will help to target which areas will respond best to opening or increased support. Because patients presenting for revision rhinoplasty may have had septal cartilage removed, it is crucial to palpate the septum to determine if there is any cartilage remaining for harvest. Similarly, it is also advisable to examine the ears to determine the availability and condition of cartilage which may be required for tip reconstruction.
Following the examination the author performs computer imaging with each patient. The process of reviewing the patient’s anatomy and modeling changes digitally provides a great opportunity to establish surgical goals, set realistic expectations, and identify patients who may be difficult. A recent study of the senior author’s experience with imaging suggests it can also be an accurate predictor of outcomes.
The final segment of the consultation involves a frank discussion about the surgical process and post operative course. It focuses on the goals of the operation and limitations based on where things are likely to be problematic. Potential complications are detailed and even the potential need for future surgery to refine postoperative asymmetries is mentioned. The patients are given a copy of their computer imaging and encouraged to follow up with any questions that they might have.
Planning:
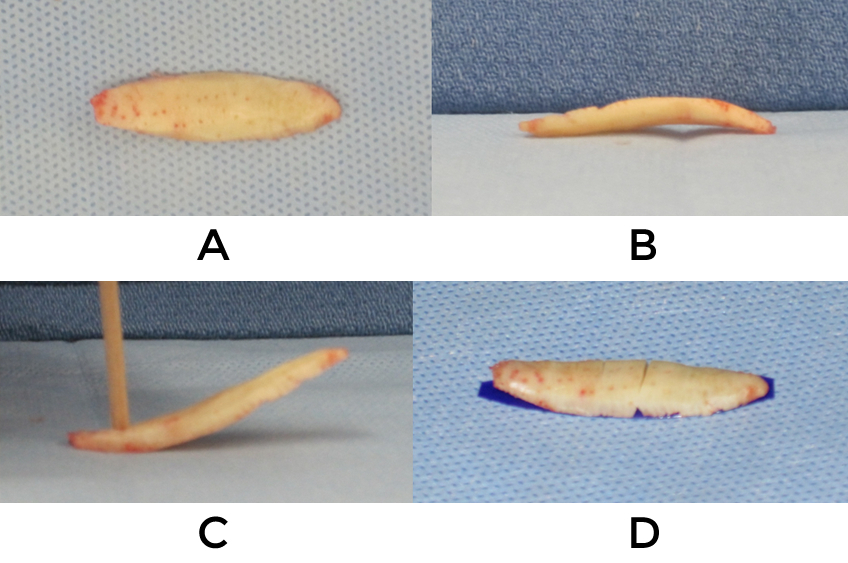
Because revision rhinoplasty involves the potential for unforeseen complexities it is vital to have a well thought out surgical plan. Prioritizing the objectives is of critical importance since during complex repairs it is easy to lose sight of the primary goals of the patient and instead get caught up with less relevant maneuvers. It is advisable to define the top two most important goals of surgery to accomplish and work towards those ends first. With respect to the tip these would mainly involve support, projection, length, symmetry and irregularities. Preoperative consideration for sources of additional cartilage allows for proper consents to be obtained, decisions to be made as to which ear to use, and for pre-surgically marking of the chest to allow for an inconspicuous incisional scar. Additionally, if the plan involves taking costal cartilage it should be harvested early so that it might sit in saline for some time, thus declaring the direction of any warping that is likely to occur (fig 5). The need for soft tissue coverage should likewise be contemplated ahead of time.
Although the author nearly always uses an open approach for revisions of the nasal tip, there are circumstances where an endonasal approach is preferred. When graft placement via precise pockets or deprojection in the face of a thick soft tissue envelope are the primary maneuvers to be performed, the endonasal approach offers several advantages. Among these are: less dissection and resulting edema, easier placement mini-composite grafts through limited incisions rather than with the tip skin fully opened, and reduced scar contracture postoperatively. The open approach offers excellent exposure for evaluating the relationship between the tip cartilages and the domes as well as for manipulating the structure. Before creating the transcolumellar incision, the decision of whether to excise existing scar should be determined so that it can be marked appropriately. If skin is to be excised it is usually done just before closing and utilizes the aforementioned marks.
General Surgical Technique:
Vestibular marginal incisions are made with a #15 blade prior to opening the columellar incision. Not only does this assist is locating the lateral crura, but it allows for making these incisions further or closer to the nostril rims depending on specific needs such as rim grafts or lateral crural repositioning. Once the caudal border of the crurae have been exposed dissection is performed over the lateral crura in the subperichondrial plane (video 1).
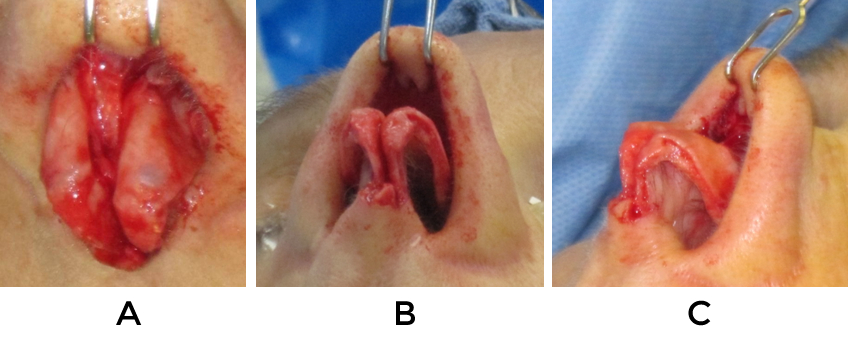
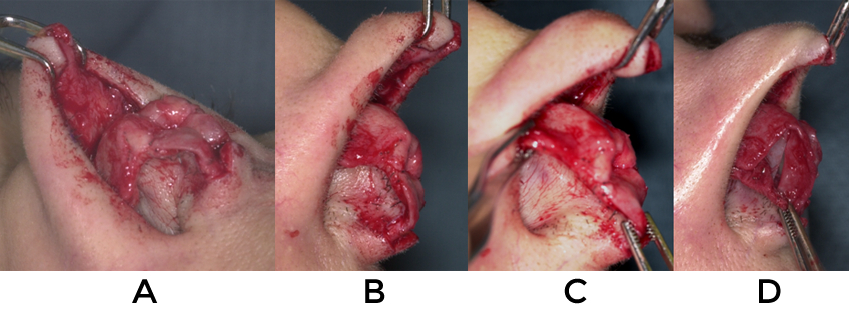
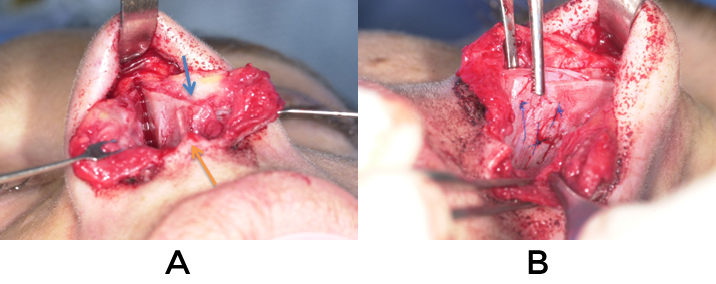
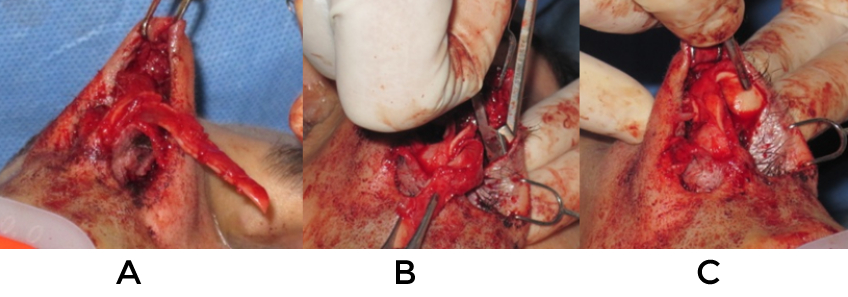
An inverted V incision is made at the columella with a #11 blade (video 2). This incision is made without regard for prior columellar scars so long as the incision healed well. If significant projection or deprojection is to occur, the incision is placed more posteriorly or anteriorly depending on the specific needs of the case. If a caudal septal extension graft is anticipated, it will be created closer to the lip to allow for easier access to the spine and floor. When elevating the tip skin it is helpful to have proper countertraction (video 3). Such assistance aids to delineate the edges of cartilage and allows for elevation in the deepest, submuscular plane. Good counter traction also uncovers buckling of the domal region which, if undetected, can lead to inadvertent transection of the lower lateral cartilages. (fig 6)
Grafts that are encountered are left in place until complete exposure has been realized and the specific needs for reconstruction are determined. Occasionally prior grafts are adherent to the undersurface of the skin and these should be left attached to the soft tissue until the specific risk and benefits of removing them are established. Dissection over the anterior septal angle and the entire dorsum allows for mobilization of the soft tissue envelope. In cases where lengthening, projection or augmentation are desired, wide dissection creates enough laxity to perform these maneuvers and allow for coverage without much tension.
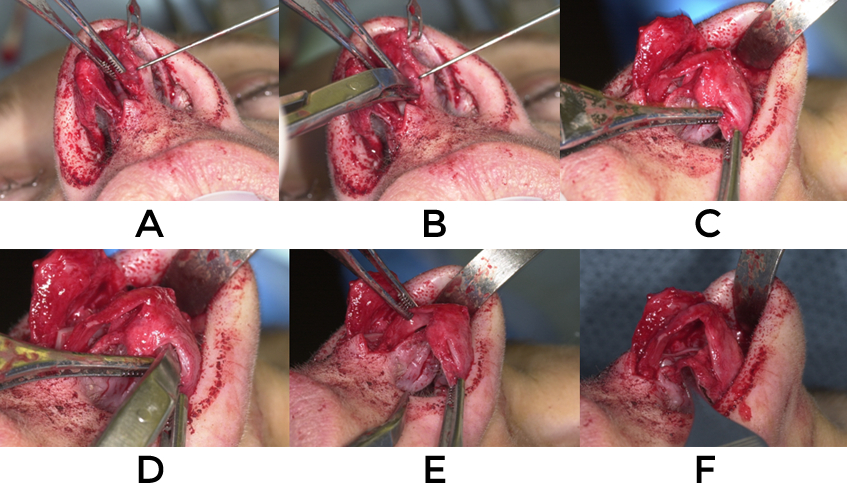
Separation of the medial crura and dissection of the interdomal ligament exposes the septum for cartilage harvest and potential repositioning (video 4). Continued dissection of the mucoperichondrial flaps from this position minimizes bleeding and allows for access to the caudal septum for suture placement and grafting (video 5). Submucosal detachment of the upper lateral cartilage further improves exposure of the septum and middle vault (video 6).
In general the surgeon must have confidence in the dorsal height prior to beginning the tip work, however the tip work may occasionally be performed primarily in a few situations: 1) when tip projection is the primary objective and it is questionable how much will be achievable 2) when a caudal septal extension graft is used or 3) when grafting material is extremely limited
Problem Solving
Although the nuances are infinite, there are several common problems that are encountered when performing nasal tip revisions. The remainder of this chapter will outline these particular problems and suggest solutions.
Problem #1
Overrotation of the tip: Two common etiologies are 1) foreshortened septum 2) retracted domes
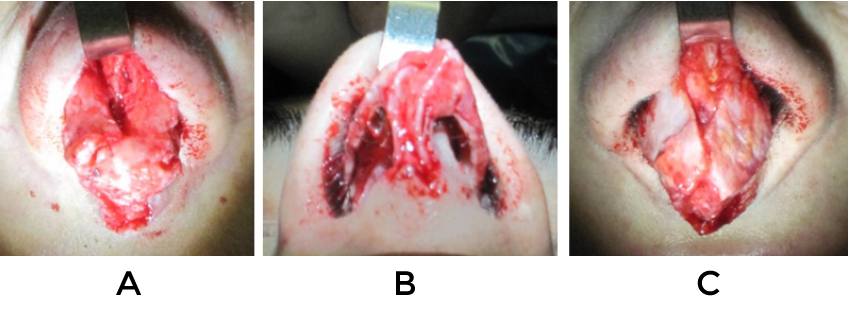
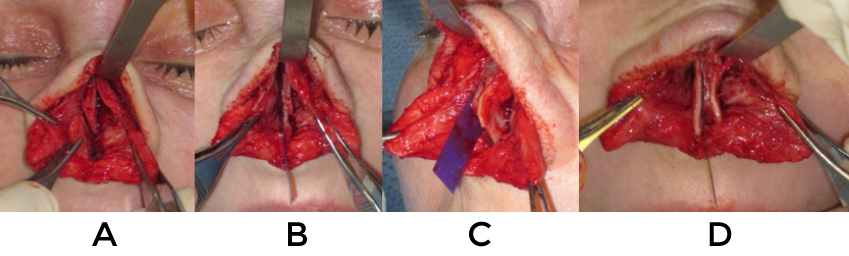
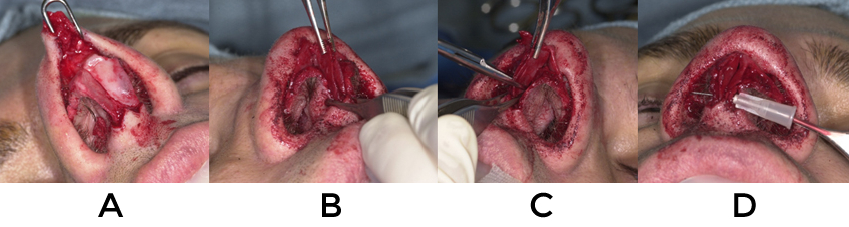
If the septum has been truncated and there is retraction or poor support at the columellar-labial angle then a caudal septal extension graft is preferred. In contrast, if the domes alone are retracted then extended spreader grafts are optimal. Firm cartilage is necessary to push the tip caudally, thus septum or costal cartilage is preferred over ear. New technologies such as the PDS plate allow the surgeon more flexibility with difficult situations where lengthening the nose is required and patients resist rib harvest (fig 8). Dissection is performed between the medial crura to expose the caudal septum and allow for submucosal detachment of the upper lateral cartilages. Vestibular skin is widely freed from the lower lateral cartilages to allow for greater freedom of movement and counter rotation (video 8).
*PDS exposed to the skin might result in significant inflammation and thickening of the skin envelope
If a caudal septal extension graft is used it should be secured such that it is closest to the midline. 3 mattress sutures of 5-0 Prolene are placed such that the length and projection are as desired (fig 9). The base can also be fixed to the anterior nasal spine by creating a hole through the spine with a 22g needle. The leading edge of the graft should be thinned out at this time. The medial crura are then sutured in a tongue-in-groove fashion to the graft such that the proper attitude of the tip is attained.
When utilizing extended spreader grafts solely for counter rotation they should be sutured with 3 mattress sutures to the sides of the dorsal septum after determining the appropriate width required. It is often the case when counter rotating the tip that the dorsal height will be lowered slightly so this should also be taken into account when securing the grafts. The caudal extent of the extended spreader grafts can be sutured together and this midline piece used as a buttress to keep the columellar complex displaced inferiorly (fig 10). Although not always necessary, the columella (with or without a strut) can be sutured to this structure to increase and stabilize tip projection. Aligning the medial crura so that the domes are more caudal than the feet helps to create counter rotation (fig 11).
If the domes are retracted and the tip is overprojected, then a medial crural overlay may correct things without the need for grafting. Divide the segment of the medial crura necessary to achieve the desired columellar:lobule ratio (2:1) (fig 12) The edges are then thinned longitudinally and the pieces secured with the posterior segments on the lateral surface using mattress sutures. This is a powerful method for counter rotation but will not provide the length that the previous methods do.
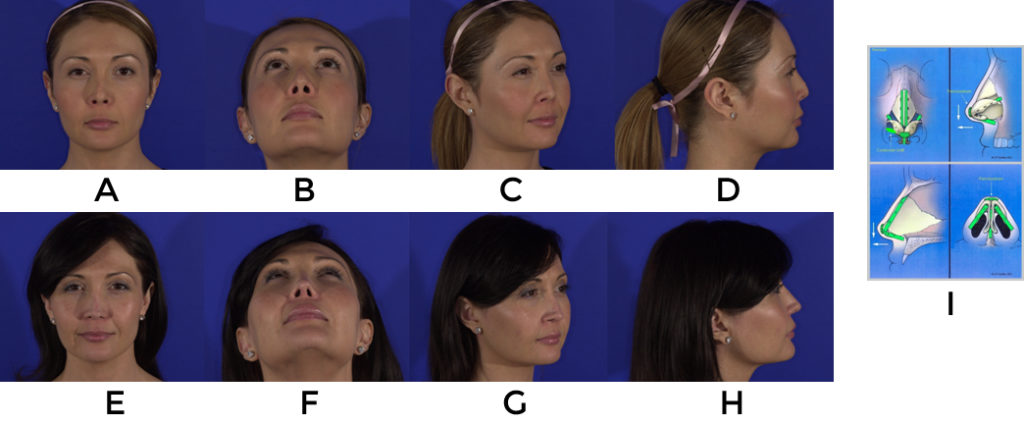
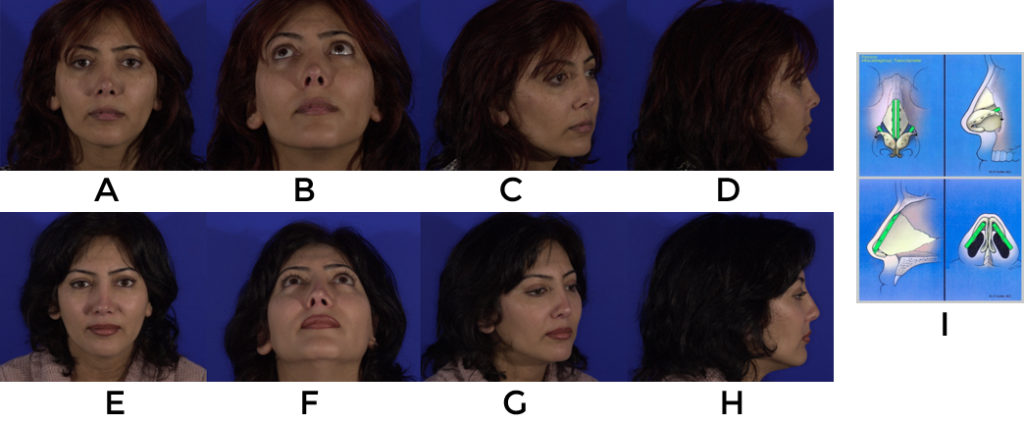
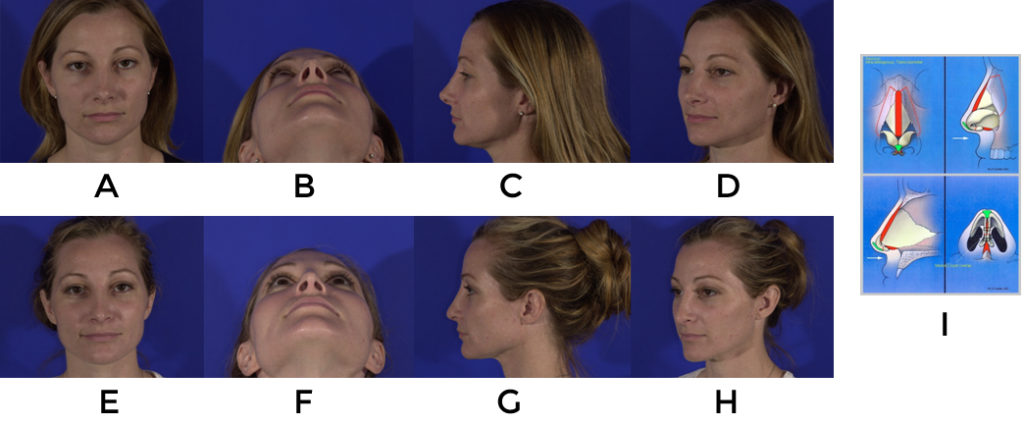
The following are examples of counterrotation using the aforementioned techniques (fig 13, 14, 15).
Problem #2
Retracted rims with excessive columellar show: Common eitiologies are 1) malposition of lateral crura 2) loss of cartilage and support 3) paucity of internal lining.
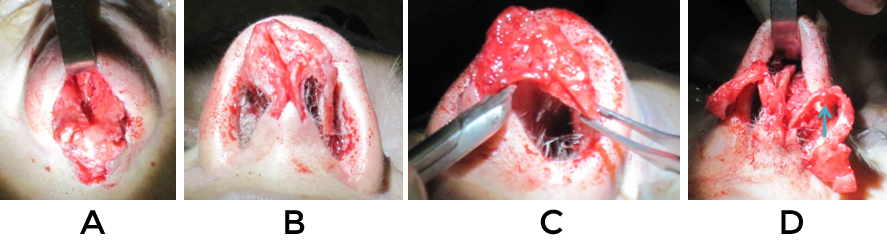
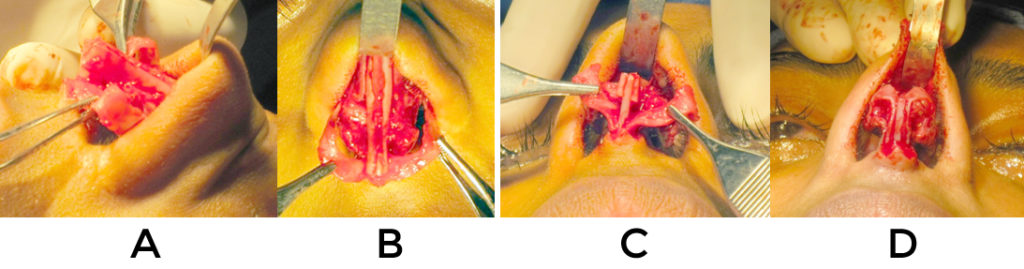
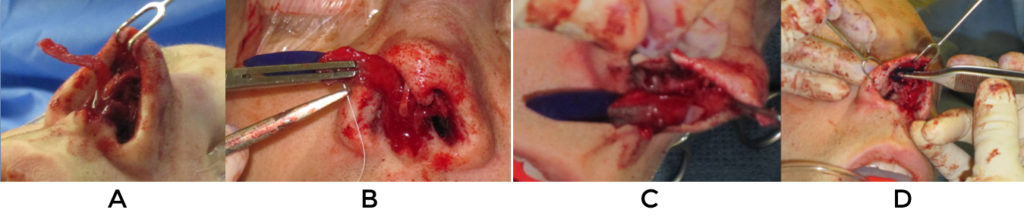
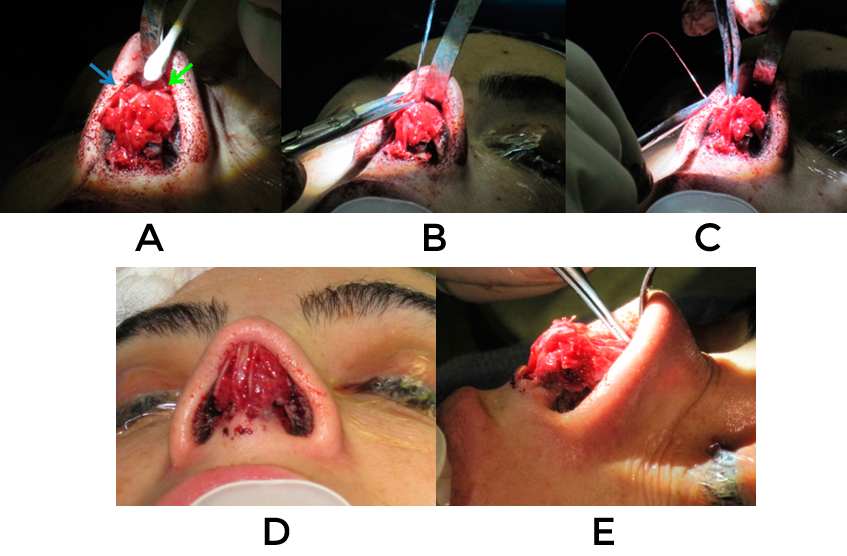
In cases where there is fullness in the supra tip as well as columellar retraction it may be the result of previously unrecognized cephalic malposition. The prior surgery may have exacerbated this problem by removing cephalic cartilage and creating wound contracture that rotated things superomedially (fig 16). The solution in such a case is to reposition the lateral crura inferolaterally. After opening the nose and assessing things the vestibular skin is widely undermined from the entire lateral crus. Next the columella and tip are stabilized and the domes secured together to help maintain symmetry. The crura are released at their lateral-most extent and usually extended with grafts on their undersurface to help prevent extrusion (fig 17). Recently PDS flexible plates have been used for this purpose when cartilage is in short supply (fig 18, video 9). Using skin hooks to provide counter traction, precise pockets are created in the vestibular skin with the converse scissors (video 10). The entrance point and orientation of these pockets with regards to the strut graft is crucial and they usually require extension to the pyriform to prevent alar collapse. Adjustments of the length and width of the crura are often necessary.

A second technique can be used in the case of supra tip fullness and rim retraction. If enough lateral crura remains and some rotation is desired, a stairstep lateral crural overlay can be very effective at bringing down the rims in proximity to the domes. After undermining the vestibular skin from the anterior ½ of the crura, they are divided in a staggered manner and the anterior piece is advanced caudally relative to the more posterior, stable piece (fig 19). Three mattress sutures are used to secure the pieces and prevent them from rotating relative to one another. Because the length of the crura are shortened, this maneuver will rotate and possibly deproject the tip as well as improve the retraction. For cases where cartilage must be replaced, alar strut grafts can be sewn so that their leading edge advances the caudal margin by a couple of millimeters.
For less severe retractions, alar rim grafts placed before closing the skin can add support and improve contour (fig 20)

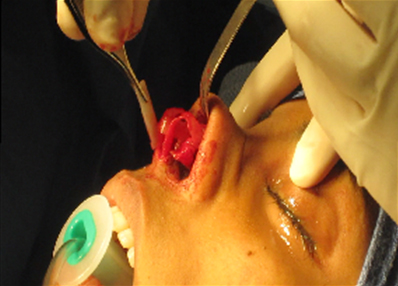
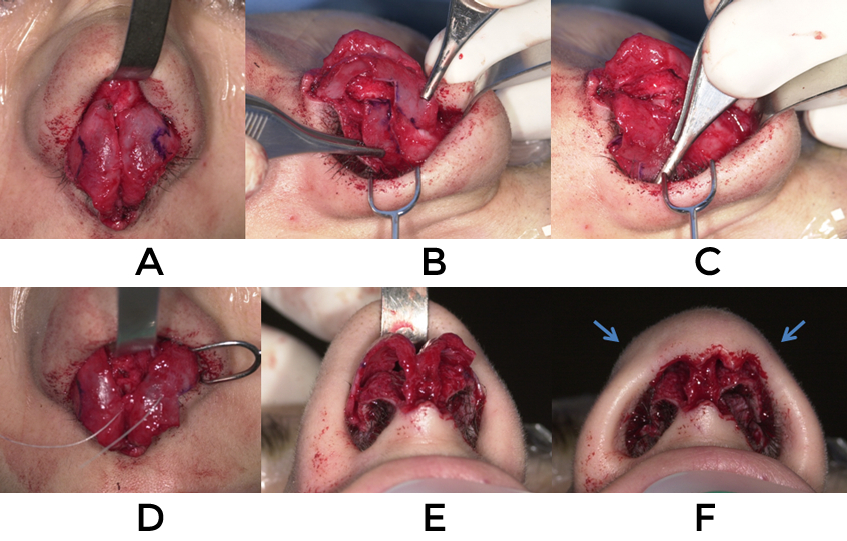
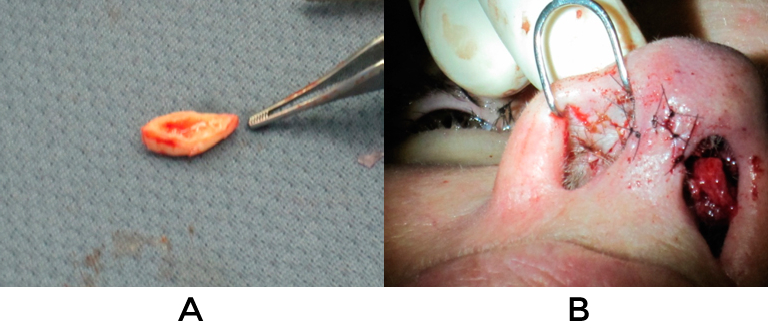
When restriction of vestibular lining is contributing to alar retraction, composite grafts are indicated. These are usually taken from the cymba concha but may also be taken from any part of the conchal bowl where the skin is tightly adherent to the underlying cartilage. Composite grafts work well as a stand alone procedure or in conjunction with any of the aforementioned maneuvers. These tend to work best for lateral retraction and are more difficult to place medially near the domes. Typically they are secured with cutaneous 6-0 plain gut sutures (fig 21).

It should be mentioned that excessive columellar show can also be improved by bringing the columella cephalad with a tongue-in-groove (video 11) or septocolumellar suture (fig 22), or shaving the leading edge of the medial crura.
Example of aforementioned techniques (fig 23).
Problem #3
Asymmetric or twisted tip: Common etiologies are 1) improper alignment of cartilages 2) over resection with weakening of support and scar contracture 3) asymmetric resection of cartilage or dome division 4) bossae formation
When there are visible and palpable irregularities at the tip it is likely that division with reconstitution and grafting will be required. It will be best to utilize thin, curved grafts from the ears and have soft tissue available for camouflage to prevent edges from becoming noticeable. Once the skin is elevated any binding sutures should be removed, as these are often part of the problem. Again it is helpful to widely free the vestibular skin from the medial and lateral crura to allow for unrestricted shape changing and placement of small grafts. Once the domes have been defined, an assessment can be made.
If the tip cartilages are simply malaligned, then a columellar strut can be placed to provide for a firm stable fixation point and the two can be reoriented relative to one another (video 12).
Asymmetrically placed mattress sutures placed in a myriad of positions can be effective for this. When aligning the cartilages from one perspective it is important to note that they may deform and come out of alignment in another position. At such times other maneuvers are needed to correct for persisting problems.
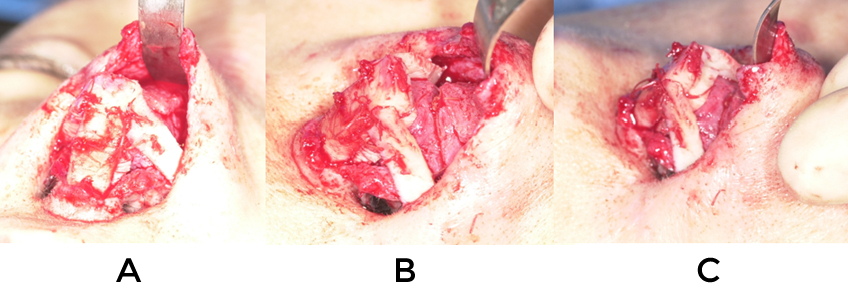
Cartilage grafting to add support in conjunction with dividing and reconstituting the domes is often times the only way to create similarly shaped tip cartilages. Overlapping edges are preferable over end-to-end sutures as they are less likely to result in visible points.
When discreet, firm points exist it is wise to place small pieces of thin cartilage or soft tissue adjacent to them and lay perichondrium or fascia over the entire complex.
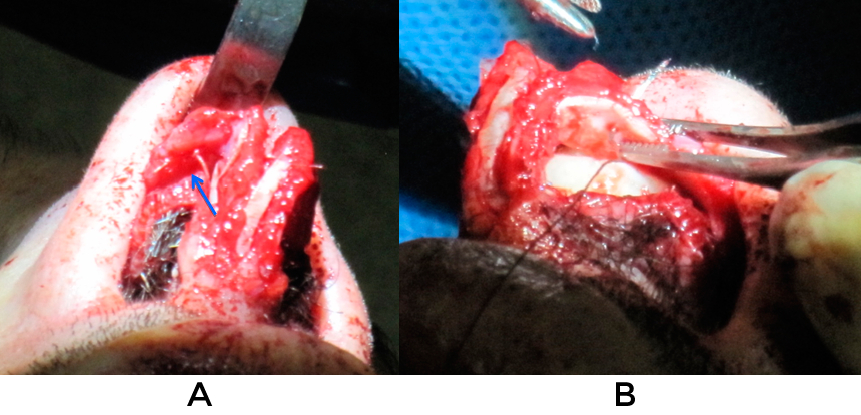
In situations where the points are not able to be camouflaged, dome division can allow for a smoother contour to the nasal tip (fig 24). Likewise, if previous dome division has been performed and the patient presents with significant collapse of the lateral crura or bossa, subdomal grafts can help recreate the smooth contour in the intermediate region of the lower lateral cartilage (fig 25, video 13). Bossae present similar challenges but often are the result of contracture of the vestibular lining which creates knuckling (fig 6). Sometimes releasing the soft tissue allows these to unfurl and flatten out. If this is not the case they can be handled in the manner mentioned above or shaved down.
Examples of the aforementioned procedures (fig 26, 27)
Conclusion:
It is not possible to provide a specific step-by-step approach for revising the nasal tip because there is no standard set of circumstances or anatomic configurations. Each nose carries its own idiosyncratic set of challenges. With careful preoperative diagnosis and analysis, the surgeon should be able to closely estimate what he or she will find intraoperatively and create a comprehensive plan for the repair. If the correct plan is actualized, even if not done with superior technical skills, the patient is likely to be content. Thus it is best to focus on what needs to be accomplished to render the result you seek, rather than on precisely how to do it. Have confidence in your decisions and carry out the maneuvers described herein and from other sources. With experience and honest critical analysis of your outcomes improvement will come.
