Introduction
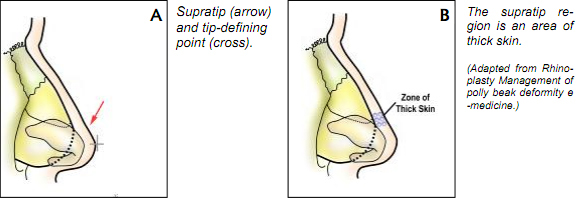
Post-operative persistent, unattractive nasal dorsal fullness in the lower half that distorts the profile and observes the nasal tip similar to the convex profile of the parrot’s beak is colloquially termed Polly Beak deformity.
In general, rhinoplasty remains the most challenging of all esthetic facial procedures. Never are two procedures ever identical. Hence, it is important that rhinoplasty should be approached as an anatomical dissection and exposure of the nasal structures requiring alteration, conservatively shaping and reposition- ing these anatomic elements. Many problems including polly beak deformity and other complications arise from over correction of nasal abnormalities than from conservative correction. The statement “It is not what is removed in rhinoplasty that is important but what is left behind” stands true and will always stand true.
While the polly beak may be the result of techniques, it may also be an unpredictable complication for even the most experienced surgeon. Under re- section of the cartilaginous middle third of the nose gives rise to a common rea- son for revision rhinoplasty surgery: the pollybeak. This supratip prominence is most often a consequence of inadequate lowering of the dorsal septal / upper lateral cartilage complex comprising this area. The combination of a lowed dor- sum, a relatively high septal angle and postoperative loss of tip support with re- sultant tip deprojection presents as a polly beak deformity. Soft tissue scaring can also give rise to this complication. The causes of polly beak include inade- quate resection of supra-tip structures, most commonly the dorsal septal carti- lage or the cephalic margins of the lower lateral cartilages; loss of tip support; or paradoxically excessive cartilage resection in the supra-tip region that results in subcutaneous our scar tissue formation, often in conjunction with thick nasal tip skin. If excess cartilage is the cause, cartilaginous polly beak is the termed used and simple trimming of this cartilage will solve the problem. With loss of tip support, a cartilage strut or tip graft can be placed to correct or disguised the de- formity. It can also be caused by over resection of the nasal bone as well.
Deformity that occurs paradoxically as a result of over resection of the lower dorsal cartilaginous septum and/or the cephalic margins of the lower lat- eral cartilage in the area of the supratip is a more difficult problem. This usually occurs in combination with thick nasal skin resulting in inadequate skin contrac- tion and excess dead space between the skin and septal border, which fills with fibrous scar and results in supra-tip fullness. Poor redraping of inelastic nasal skin, inadequate trimming of vestibular mucosa after large reduction can also be the cause. This is also seen in patients who are undergoing revision rhinoplasty with major alar and septal cartilage resections. This deformity is more precisely called soft tissue polly beak.
In the latter, it is sometimes possible to expect this post-operative deform- ity and take corrective measures. The famous and well known Simon’s equation puts all this into perspective:
PB = (BHR/CHR) x (ST/LSMC)
where,
PB = polly beak BHR = bone hump removal
ST = Skin thickness CHR = Cartilage removal
LSMC = length and strength of the medial crura.
A polly beak deformity appears unnatural and occurs when the supratip region leads the tip. A clear understanding of the nasal-tip support mechanisms is needed to predict the dynamic changes that occur during the rhinoplasty operation. Major and minor tip support mechanisms are listed below.
- Major
– Size, shape, and resiliency of the lower lateral cartilages
– Relationship of the medial crural feet to the cartilaginous septum
– Attachment of the caudal margin of the upper lateral cartilages to the cephalad border of the lower lateral cartilages - Minor
– Interdomal ligament
– Cartilaginous dorsum (septum)
– Relationship of the lower lateral crura to the pyriform aperture and the sesamoid cartilages
– Maxillary crest (nasal spine)
– Membranous septum
– Attachment of the alar cartilages to the overlying skin soft tissue enve lope.
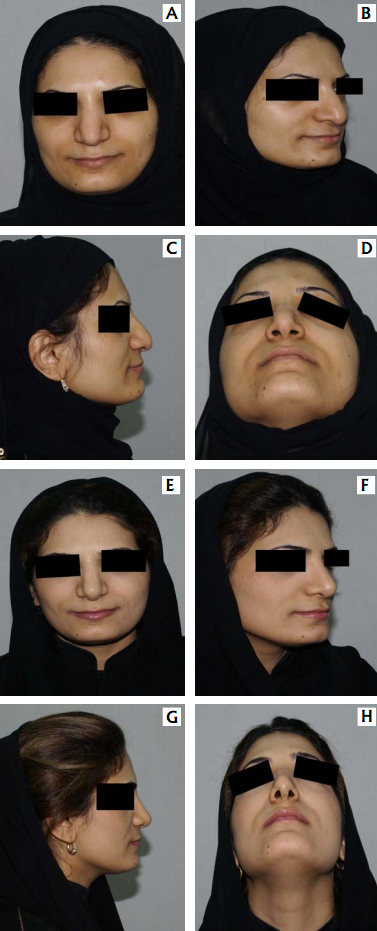
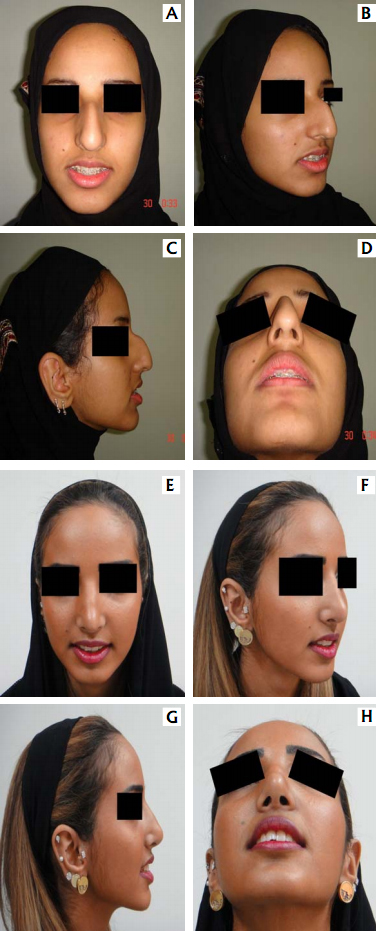
Post-operatively. D – frontal view B – oblique view C – lateral view

A – frontal view B – oblique view
C – lateral view D – basal view
She underwent open septorhinoplasty with tip work, and columellar support. The 3 month post-operative results wasm seen in:
E – frontal view F – oblique view
G – lateral view H – basal view
The exact incidence of polly beak deformity is not know but some studies have shown that up to 64% of patients presenting with complication of rhino- plasty have polly beak deformity. Since the healing time for rhinoplasty can take up to one year, this deformity should not be critically viewed till at-least an year after the primary surgery.

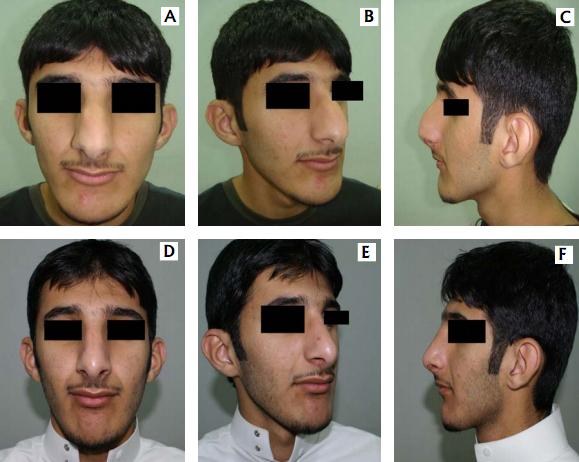
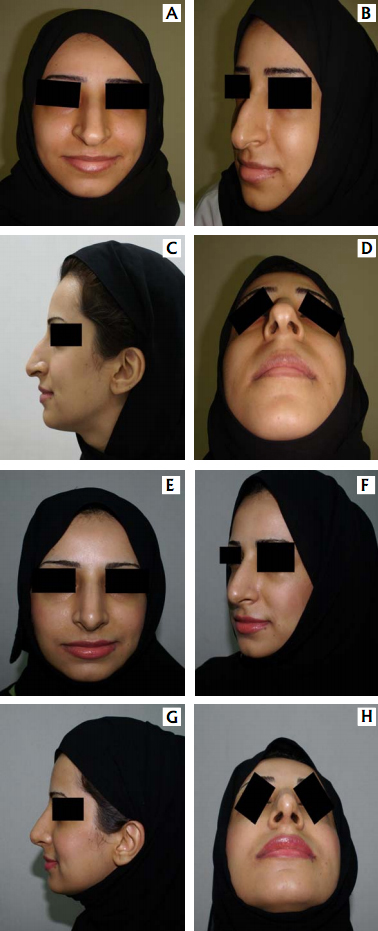
A – frontal view B – oblique view
C – lateral view D – basal view &
Post-operatively results as seen in:
E – frontal view F – oblique view
G – lateral view H – basal view
This patient underwent open septorhinoplasty 3 months ago and had incomplete resection of hump with developing tip collapse. Plan is for him to undergo local steroid injection to prevent supratip fullness to prevent polly beak deformity. If unsuccessful, he would be observed for at least 1 year before revision is considered.
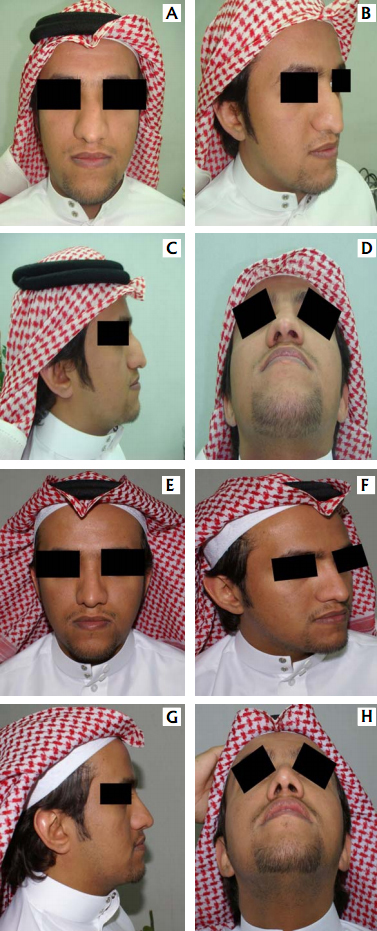
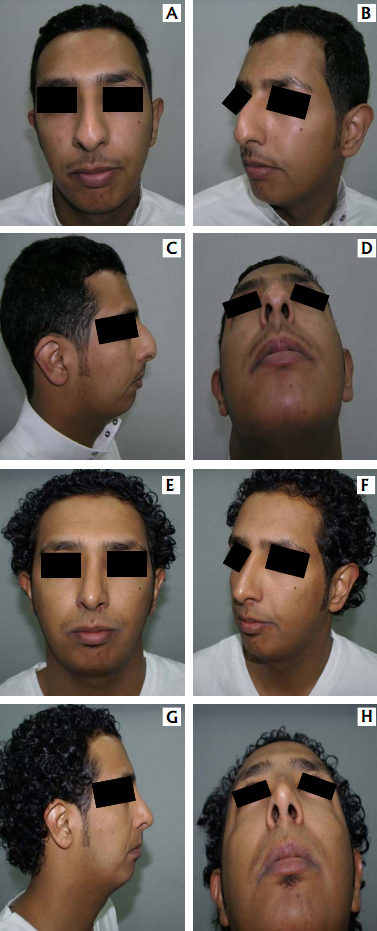
Although the incidence of finding pollybeak deformity is more in postop- erative cases, it is not the rule. Polly beak apperence of the nose is also seen, more so in the Middle Eastern and Mediterranean noses. Some of the noses with similar deformity are shown in Fig. 3 & Fig. 4.
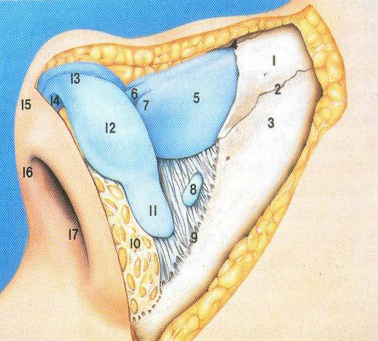
Pre-operative Analysis
An exacting pre-operative analysis and diagnosis of the unique nasal de- formity is arguably more important than surgical skill. Thus certain aspects of the nasal anatomy deserve consideration. Details are available in a number of ex- cellent books and atlas’s. The commonly accepted anatomical terms in rhino- plasty are illustrated in Fig. 5-7. The surgeon must note the thickness and seba- ceous quality of the nasal skin–soft tissue envelop (SSTE). In darker skin indi- viduals with thick skin, incision may take longer to heal with increased potential for a visible scar. In addition, the underlying structural framework of the nose must push into the thick soft tissue envelope in order for form to project through. Moreover, a significant tissue void in such patients will result in exuberant scar formation and poor definition, particularly in the tip and supra-tip areas. Thus the post-operative soft tissue polly beak may be prevented by avoiding over reduc- tion of structural framework of the thick skin nose and opting instead to achieve balance by augmentation to areas of relative deficiency.
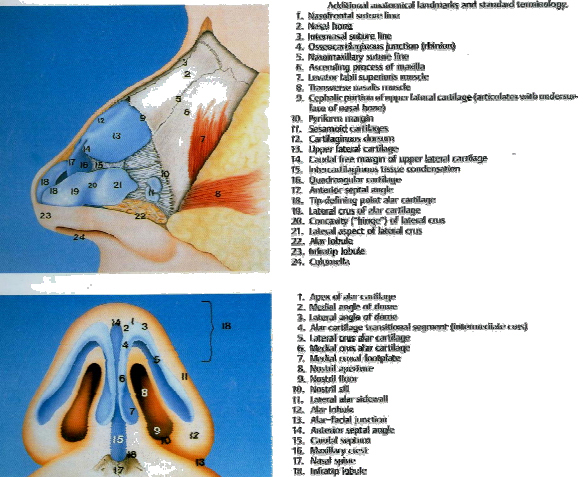
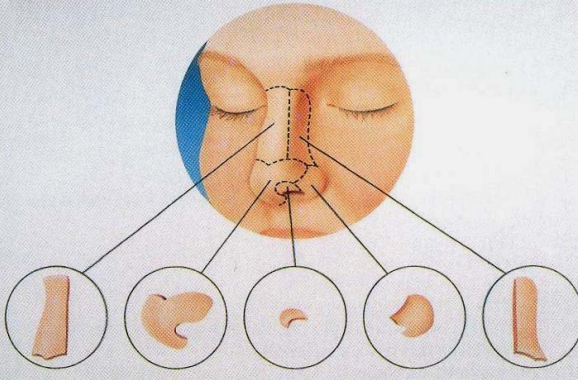
1. Nasal bone
2. Nasomaxillary suture line
3. Ascending process of maxilla
4. Rhinion/Osteo-Cartilagenous junction
5. Upper lateral cartilage
6. Anterior septal angle
7. Free caudal edge of upper lateral cartilage
8. Sesmoid cartilages
9. Margin of pyriform fossa
10. Alar lobule
11. Lateral part of lower lateral / alar cartilage – lateral portion
12. Lateral part of lower lateral / alar cartilage – central portion
13. Tip defining point
14. Intermediate part of lower lateral / alar cartilage
15. Infratip lobule
16. Columella
17. Footplate of medial crura of lower lateral/alar cartilage
Medical Therapy
Medical treatment is possible only in the early stages of soft-tissue polly beak. Steroid injections can be administered to decrease edema and ultimately the amount of scar tissue that forms in the dead space of the supratip region. These injections can be given prophylactically in patients at increased risk of this deformity (eg, those with thick nasal skin, poor skin elasticity, large nasal reductions) or as treatment for a developing polly beak. Injections must be deep to the dermis to avoid changes in the dermis and epidermis (eg, hypopigmenta- tion, atrophy).
Triamcinolone acetonide 10 mg/mL (0.1-0.5 mL) can be injected into the area. It can be diluted with normal saline or 1% xylocaine. The injection should not be administered more often than once every 3-4 weeks. Overtreat- ment may result in atrophy that may produce saddle-nose deformity or irregular skin changes. Diminishing returns are noted with repeated injections. Usually a 1 mL tuberculin syringe with 30 gauge needle is used.
As a standard practice in intra lesional injections, the importance of aspiration prior to injection cannot be over emphasized. Apart from cases of Cushing’s Syndromes, there has also been a case of blindness following the injection, possible by emboli obstructing the optic vessels.
Operative Strategy
Pre-operative analysis of the morphological problems of the nose is the basis of an efficient surgery.
The preferred approach for correction for correction of polly beak deform- ity is the open approach. This is because generally such deformity is:
– Post-operative surgical deformity – secondary to primary rhinoplasty.
– Approach to the supra dorsal/cephalic region. – Tip de-fattening if required.
– Need for a spreader graft and tip support if required.
Surgical Therapy
The profile is aligned by balancing dorsal reduction and augmentation. The importance of preoperative nasal analysis cannot be stressed enough. This thorough assessment helps the surgeon identify problem areas. (Fig. 9) con- sider solutions, and mentally perform the operation before embarking on the ac- tual procedure.
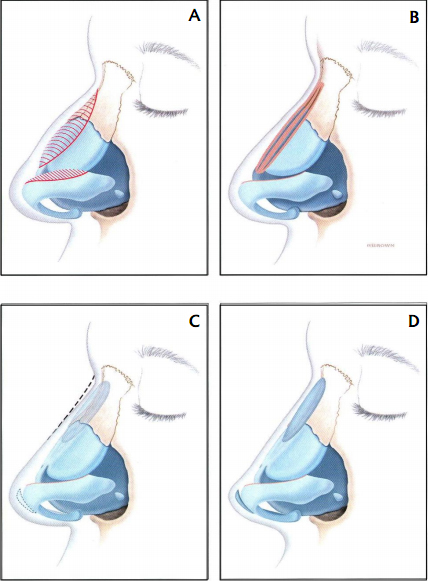
A) Thick skin patients need to undergo expansion of structures into the thick skin. Excess reduction of the dorsum causes polly beak deformity.
B) When dorsal profile is over reduced, there is excess SSTE and hence polly beak deformity worsened by tip support loss, loss of dorsal height and tip projection reduction.
C) Surgical intervention could include tip projection and dorsal grafts.
D) Expansion of thick nasal skin can improve tipsupra tip relation and balance the nose.
(Adaptive from Essentials of Septorhinoplasty – Han’s Behrbohm, M. Eugene Tardy Jr. Thieme 2009)
Sequential lower of the anatomic components under direct vision will al- low restoration of dorsal cosmesis. When the polly beak is cartilaginous, a colu- mellar strut may be required for added support and it is our standard practice to such a graft after any external approach. Soft tissue polly beaks are more trou- blesome and scar tissue may need to be excised at revision surgery followed by interval steroid injections as mentioned before.
It is important not to disturb the sub-dermal plexus when resecting soft tissue. A simple but effective technique is to use a multi toothed Brown-Adson’s forceps to remove excess tissue without undue force.
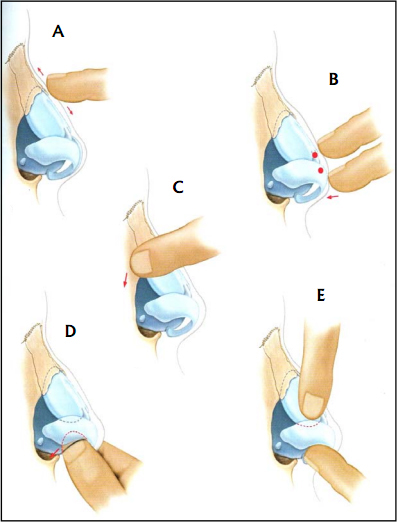
A) This is done to explore elasticity, thickness and texture of the skin and any irregularities like bony projections, their site, bony borders and open roof.
B) A good indicator for tip support is the tip recoil maneuver. The palpation of the anterior septal angle gives us idea of the size of the septum and its tension.
C) Explore the length and strength of the bony pyramid.
D) Palpation of the caudal septum, vestibule and the nasal spine. This gives us idea about the anterior septum, its tension, breadth and strength, the size and shape of the na sal spine, and tension of foot plate, the medial crura and membraneous septum.
E) Bidigital evaluation of the lower and upper lateral cartilages, their shape, size and elasticity.
(Adaptive from Essentials of Septorhinoplasty – Han’s Behrbohm, M. Eugene Tardy Jr. Thieme 2009)

A) Intraoperative view showing dorsal hump resection. It need to be remembered that less is always better and to always reassess before complete resection.
B) Columellar strut being put in place and
C) Fixed to the media crura.
A – frontal view B – oblique view
C – lateral view D – basal view &
She underwent open septorhinoplasty and her findings one year postoperative as seen in:
E – frontal view F – oblique view
G – lateral view H – basal view
A – frontal view B – oblique view
C – lateral view D – basal view &
And two years post-operatively in:
E – frontal view F – oblique view
G – lateral view H – basal view
A – frontal view B – oblique view
C – lateral view D – basal view &
And two years post-operatively in:
E – frontal view F – oblique view
G – lateral view H – basal view
A – frontal view B – oblique view
C – lateral view D – basal view &
And two years post-operatively in:
E – frontal view F – oblique view
G – lateral view H – basal view
A – frontal view B – oblique view
C – lateral view D – basal view &
And two years post-operatively in:
E – frontal view F – oblique view
G – lateral view H – basal view
For the external rhinoplasty approach, redrape the skin-soft tissue enve- lope before evaluating the profile. In addition, account for the degree of tip set- tling (1-2 mm) that may occur after surgery.
Fibrin glue may be used prophylactically in patients who are at high risk for a postoperative polly beak deformity. If amount of dead space between the skin and its underlying cartilaginous framework is substantial, fibrin glue can be used to promote adherence. This method helps prevent the formation of exces- sive scar tissue and helps improve definition of the nasal tip. As an alternative, in patients with thick skin, placement of an absorbable suture from the dermis to the deep tissues (cartilaginous dorsum of the supratip) can make the skin re- drape appropriately. Tying of this suture may need to be tried several times be- fore an appropriate position is achieved.
Remove the cast in 1 week. Make a preliminary assessment of the out- come after the cast is removed. If edema is substantial, tape should be reap- plied, and the patient should return in 1-2 weeks. Some patients may be candi- dates for steroid injections at this time. If a patient continues to have excessive supratip edema and scar tissue, steroid injection may be performed again at 4-6 weeks postoperatively. For Asian noses with a severely contracted, short nose combined with nasal tip depression after removal of their silicone implants, the use of supratip transposition flap is being used.
Features of this deformity include contracted skin envelopment, which manifests with an obtuse nasolabial angle and is prone to develop a pollybeak deformity over the supratip after nasal lengthing, and dimpling deformity over the tip. Initially the bony cartilaginous framework is exposed through an open rhinoplasty approach. To preserve the circulation of the skin envelope, degloving just along the supraperichondrial and subperio- steal plane is important for preservation of the supplying arteries and subder- mal plexus of the nasal tip. After the rebuilding of the bony cartilaginous frame- work to elongate the skin envelope, the transcolumellar incision was approxi- mated.
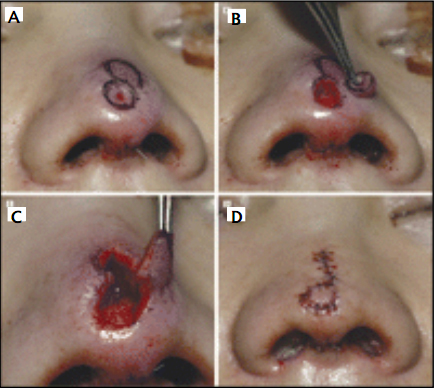
If pollybeak deformity and dimpling deformity of the nasal tip is present, the supratip transposition flap is designed adjacent to the nasal tip depression (Fig. 16). To minimize a standing cone deformity over the donor site, an ellipti- cal flap, instead of a round one, is designed (Fig. 16A). Then the dimpled area in the nasal tip is excised (Fig. 16B), and the flap is elevated and rotated into position (Fig. 16C). The incision lines are closed in a single layer with 7-0 ny- lon sutures (Fig. 16D). After the closure of the remaining incisions, the external splint is applied so as not to compromise circulation of the transposed flap. The sutures are removed on the fifth or seventh postoperative day.
Dong Hak Tung, Ray Yung Chiou Lin, Hyeong-Jun Jang, Correction of Polly Beak & Dimpling deformities of the Nasal tip in the Contracted, Sort Nose by Use of A Supratip Transposition Flap. Arch Facial Plastic Surg Sept / Oct 2009; 11 (5):311-319.
Complications
Excision of scar tissue in the supratip region may lead to thin atrophic skin and tissue loss. In general, full-thickness skin loss occurs by operating in the improper plane and by performing overly aggressive resection that trans- gresses the dermis. region is not reported.
Overuse of steroid injections can result in atrophy at the site of injection. This atrophy can lead to a depression of the supratip region resulting in a saddle -nose deformity. Other skin changes, including subdermal atrophy, depigmenta- tion, telangiectasia formation, necrosis, and ulceration, can occur.
References
- Leong S. C, Eccles Ronald, Race & Ethnicity in Nasal Plastic Surgery: A Need for Science Facial Plast Surg 2010; 26:63-68
- Rolling K. Daniel, Middle Eastern Rhinoplasty: Anatomy, Aesthetics, and Sur gical Planning. Facial Plast Surg 2010;26:110-118.
- Dong Hak Tung, Ray Yung Chiou Lin, Hyeong-Jun Jang, Correction of Polly Beak & Dimpling deformities of the Nasal tip in the Contracted, Sort Nose by Use of A Supratip Transposition Flap. Arch Facial Plastic Surg Sept / Oct 2009; 11 (5):311-319.
- Matthew M. Hanasono, Russell W H Kridel Norman J. Pastorek, Correction of the Soft Tissue Polly Beak Using Triamcinolone Injection Arch Facial Plast Surg 2002 Jan-Mar 4(1)26-30
- Henry D. Sandel IV, Jennifer P. Porter, Rhinoplasty, Management of Polly Beak deformity eMedicine for WebMD, May 5, 2009
