Corresponding Author:
Ira Papel, MD
The authors have nothing to disclose.
Abstract/Synopsis:
The facial plastic and reconstructive surgeon must carefully consider both nasal form and function to successfully perform rhinoplasty surgery. This chapter highlights important nasal anatomy, preoperative considerations, and various techniques to improve the structural support of the alae. Structural techniques involving cartilage grafts, suture techniques, and additional relevant approaches to provide alar support are discussed. We aim to equip the rhinoplasty surgeon with a set of reliable tools to successfully improve alar structural support in patients with nasal obstruction while respecting nasal aesthetics.
Keywords: rhinoplasty, functional nasal surgery, tip rhinoplasty, nasal alar support, nasal valve
Introduction
Rhinoplasty surgery is one of the most challenging procedures requiring an expertise in both the underlying dynamic nasal anatomic structure and a critical appreciation for nasal aesthetics influencing facial attractiveness. Commonly, patients seek rhinoplasty to address nasal obstruction, which can be related to a myriad of anatomic nasal deformities or deficiencies that compromise nasal airflow. In performing rhinoplasty, the surgeon aims to improve the underlying nasal structure while respecting potential aesthetic ramifications. Importantly, the rhinoplasty surgeon must carefully consider the internal and external nasal valve function and apply correct techniques to achieve a successful outcome. Among these considerations, improving the structural robustness of the alae may be required to improve nasal function. The objective of this chapter is to discuss the various techniques to improve alar structural support when performing rhinoplasty surgery.
Anatomy
An important element in mastering rhinoplasty is a thorough understanding of the anatomic framework of the nose including the skin-soft tissue envelope, cartilaginous structure, and bony vault. Much like a sculptor and engineer, the rhinoplasty surgeon must appreciate the intrinsic characteristics of the nasal components, the interplay between these components, and the dynamic external forces acting upon the framework, which varies between patients.
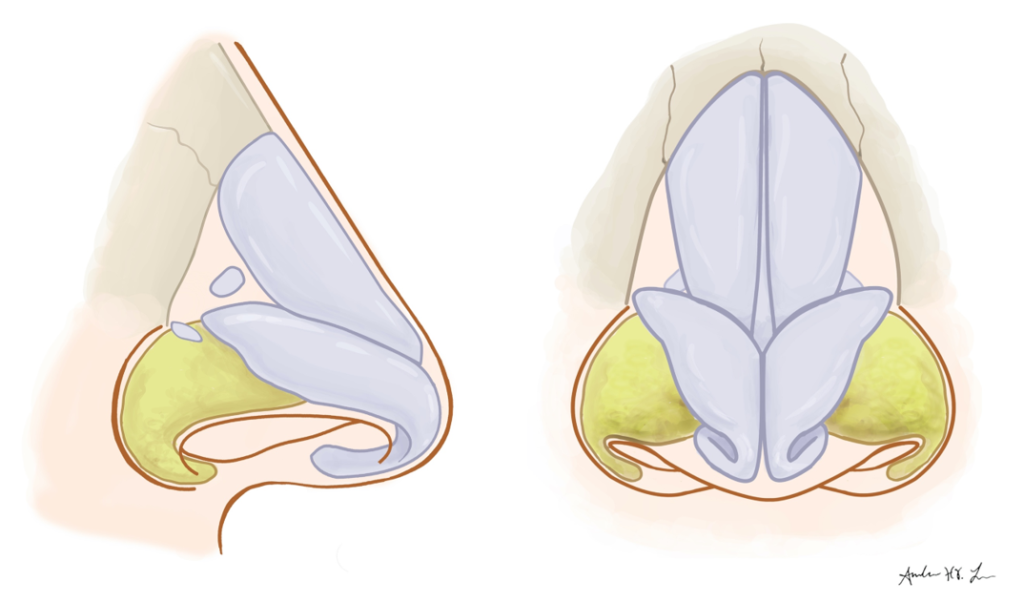
Lower lateral cartilage – medial, intermediate, and lateral crura
- : footplate and columellar segments
- : lateral aspect of lateral crura with fibrofatty tissue supporting ala
External nasal valve
Boundaries: Alar sidewall, medial crus, nasal spine, floor of nose
| Major tip support structures: |
| 1) Strength of lower lateral cartilages including size, shape, thickness |
| 2) Scroll region with junction of upper lateral cartilage and cephalic margin alar cartilage |
| 3) Medial crura attachment to caudal septum |
Preoperative Analysis
Clinical History/Motivations/Expectations
The preoperative interview is an important opportunity to capture the patient’s clinical history including specific complaints, prior medical and surgical interventions, medical history, and other potential risk factors important for surgical decision-making. Importantly, the rhinoplasty surgeon must clearly understand the patient’s expectations, motivations, and self-image, which are not always readily apparent. Both functional and aesthetic goals should be explicitly discussed as well as highlighting the risks and limitations of surgery in achieving the patient’s goals. Photo documentation and image editing software can complement these discussions. Upon developing a trusting relationship, setting realistic expectations improves rhinoplasty outcomes and satisfaction for both the patient and physician.
| Patient Selection |
| Realistic and specific functional and aesthetic surgical goals |
| High chance of achieving goals by surgeon |
| Acceptance that there is no guarantee of attaining the anticipated result, perfection, or psychosocial improvement |
| Demonstrates ability to tolerate suboptimal results or complications |
Physical Exam
Patient examination should be performed using a standardized approach. First, the facial structure, shape, and proportions should be evaluated. Next, the patient’s skin thickness, quality, elasticity, and pigmentation should be noted as well as appreciating ethnic characteristics. For example, identifying if the patient has thick or thin skin proves critical for surgical planning and the expected postoperative course. Nasal analysis can be performed in thirds by assessing the upper, middle, and lower third of the nose. For the purpose of this chapter, we will emphasize nasal analysis of the lower third, nasal tip including the alae, but careful inspection and palpation of the patient’s nasal bony pyramid, midvault, septum, and inferior turbinates are critical when assessing nasal function and appearance.
| Functional Considerations |
| Nasal valve collapse, septal deviation, synechia |
| Weak tip support – weakness of ULC, LLC, or soft tissue |
| Prior trauma or surgery, scarring contraction of soft tissue |
| Congenital nasal deformity |
| Nasal deformity related to facial paralysis |
Nasal Tip Analysis
The nose should be examined from the frontal, lateral, and base views with attention to nasal deformities, asymmetries, and distinct nasal features as manifested by highlights and shadows creating contour. On frontal view, the brow-tip aesthetic line, alar base width, and tip definition should be assessed. The nasal tip should be examined for a double break of the supratip and infratip, degree of bulbosity, and width of the alar base. Bulbosity may be related to skin thickness, width of the lateral crura, cephalic positioning of the lower lateral cartilage, or an exaggerated divergent interdomal angle. On profile view, tip rotation, projection, and definition should be inspected. Additionally, the alar-columellar relationship, nasal length, and chin position should be assessed. On basal view, the height and shape of the lobule, columella, nostrils, and alar base should be examined. The alar base should approximate the intercanthal distance proportional to the rest of the face. External nasal valve can be assessed by having the patient inspire while noting the presence of alar collapse.
In addition to visual inspection, the nasal tip should be palpated to determine tip support and the intrinsic strength of the underlying septum and lower lateral cartilages. Assessing lateral crura orientation is important. Notably, a common issue is the presence of cephalic malposition characterized by a parentheses appearance on frontal view and an associated deficiency at the alar lobule. Further, the surgeon should examine the shape, width, and curvature of the lower lateral cartilages. Correspondingly, lateral crural deficiency may be present related to weak, over-resected, or concave cartilages. Revision rhinoplasty patients may present with excessive cephalic trim, alar retraction or notching, or vestibular scarring.
| Common surgical problems |
| weak intrinsic strength of lower latera cartilages |
| overprojected tip |
| wide columella |
| cephalically positioned lateral crura |
| lateral crural deficiency |
| alar collapse |
| lack of dilator nasalis function related to facial paralysis |
| prior reductive rhinoplasty |
Alar Structural Support Techniques
After meticulous nasal examination, deliberation of functional and aesthetic factors, and visualization of desired nasal changes, both immediate and long-term changes, the surgeon may elect to perform a single or combination of rhinoplasty techniques to provide increased alar support. The surgical options include structural grafting, suture methods, or other less common techniques. Additionally, open or closed rhinoplasty may be performed depending on the technique utilized and surgeon preference. Commonly, rhinoplasty requires grafting material with common grafts including septal cartilage, auricular cartilage, and cadaveric vs. autologous rib cartilage. Understanding the strengths and limitations of each surgical technique and graft type is vital in developing the surgical plan. In the following section, indications, technical descriptions, and strengths/limitations of each alar structural support technique will be discussed.
Structural Graft Techniques
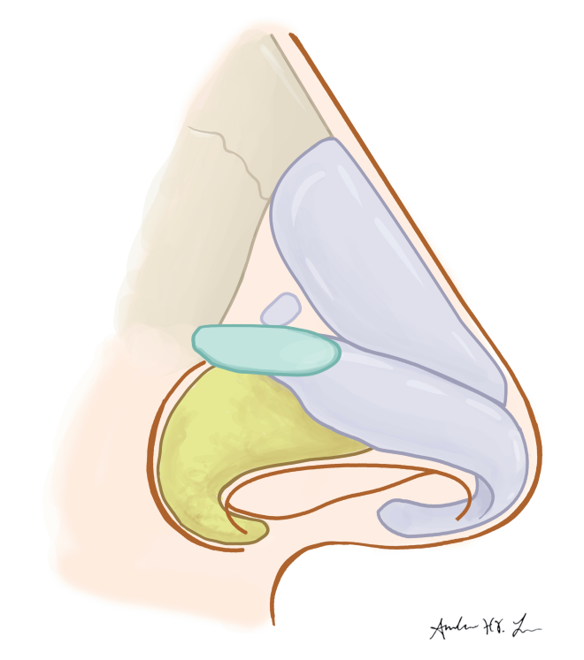
Alar Batten Grafts
Alar batten grafts are cartilage grafts with a convex surface that are inserted in a pocket at the location of nasal valve collapse, internal or external, and oriented laterally sitting on the pyriform aperture. This technique is useful to prevent external/internal nasal valve collapse, reposition the nasal lateral wall, and address supra-alar pinching. Additionally, this technique may be useful in patients with facial paralysis.
Technique 1
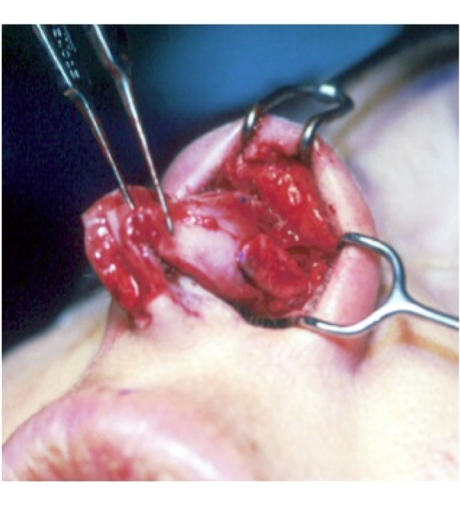
- The surgeon may perform alar batten grafts through an open or closed rhinoplasty approach.
- The alar batten grafts are carved in a rectangular shape with dimensions measuring 10-15mm in length and 4-8mm in width adjusting the size of the graft depending on the severity of collapse and thickness of skin. Grafts should be thick enough to overcome negative inspiratory forces and thin enough to prevent excess widening.
- The site of most severe nasal valve collapse is identified and marked externally for the anticipated placement of the graft
- After injecting local 1% lidocaine with 1:100,000 epinephrine, a precise pocket is dissected at the site of nasal valve collapse.
- The pocket is dissected in a subcutaneous plane extending laterally to the pyriform aperture. Avoid dissecting an unnecessarily large pocket or dissecting too laterally to minimize bleeding, swelling, and postoperative migration.
- Gently place grafts into the pockets. Grafts should slide easily, but without a loose fit. With closed rhinoplasty, there is often no need for suture fixation. Otherwise, suture fixation can be useful to prevent medial or superior migration.
Limitations
- Transient and possibly persistent lateral wall fullness
- Widening of nose
- Graft may mobilize, especially if pocket dissected widely
- Decreased success in patients with contracted scar, loss of vestibular skin, or narrow pyriform aperture
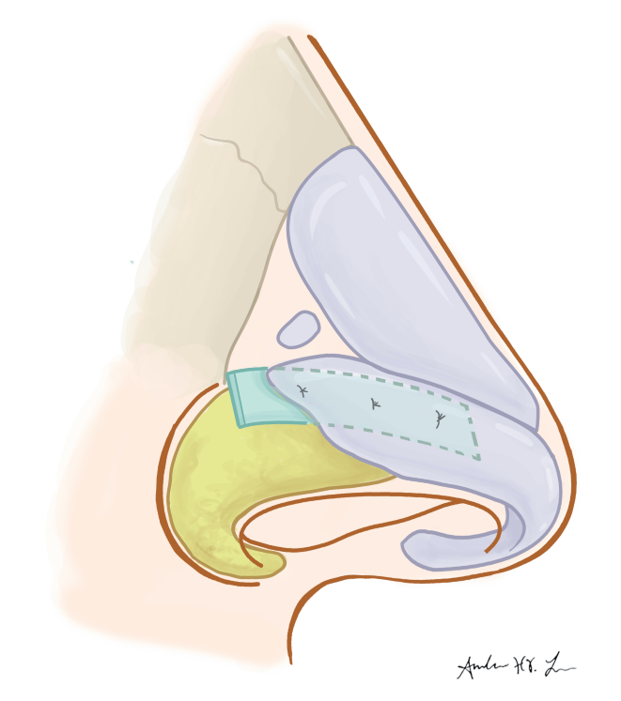
Lateral Crural Strut Grafts
Lateral crural strut grafts are thin, flat cartilage grafts that are placed between the vestibular skin and the undersurface of the lower lateral crura. This technique is useful in reshaping, repositioning, or reconstructing the lateral crura. For patients with a boxy nasal tip, malpositioned lateral crura, alar rim retraction, or concave lateral crura, the rhinoplasty surgeon may elect to use lateral crural strut grafts.
Technique 2
- The surgeon typically will perform lateral crural strut grafts through an open rhinoplasty approach.
- The lateral crural strut grafts are carved in a narrow, rectangular shape with dimensions measuring 15-25mm in length and 3-4 mm in width. Grafts should be thick enough to overcome negative inspiratory forces and thin enough to prevent excess intranasal bulk.
- After injecting 1% lidocaine with 1:100,000 epinephrine between the lateral crura and vestibular skin, dissection is performed gently undermining the vestibular skin off the lateral crura. Vestibular skin is elevated from the cephalic border to the caudal border of the lateral crura. The anterior third to two thirds of the vestibular skin is left intact at the caudal border.
- In cases of severe alar collapse, retraction, or lateral crural malposition, the lateral crura are completely released laterally. A pocket may be dissected laterally over the pyriform aperture for placement of the lateral crural strut graft.
- The strut grafts are placed on the undersurface of the lateral crura and secured with 2-3 mattress sutures. The lateral end of the strut graft is placed caudal to the alar groove.

Limitations
- Tedious, and can be time consuming
- Possibly difficult in revision rhinoplasty given the amount of cartilage required
- Grafts may be bulky
- Risk for asymmetry, especially with full release of the lateral crura. This is often not indicated.
Lateral Crural Grafts
Lateral crural grafts are flat cartilage grafts placed as an onlay graft at sites of previously excised cartilage or weakened lateral crura functioning as an anatomic graft. This technique is useful to correct tip deformities, especially useful in revision rhinoplasty to correct asymmetries and bossae combined with other techniques. Additionally, this technique can be used to create a nasal tripod framework.
Technique 1
- The surgeon may perform lateral crural grafts through an open or closed rhinoplasty approach.
- The lateral crural grafts are carved in a rectangular shape with dimensions approximating the anatomic lateral crura.
- After injecting local 1% lidocaine with 1:100,000 epinephrine, dissection is performed exposing the lateral crura completely.
- The lateral crural graft is placed as an onlay graft on the existing lateral crura or at the site of prior lateral crura resection .
- The grafts are sutured to the lateral crura using mattress sutures.
Limitations
- Fullness over lateral crura, especially in thin skin patients
- May not address nasal valve collapse depending on where the site of maximal collapse is located
- If placed in a cephalically oriented position, grafts may create the typical “parentheses” appearance
Lateral Crural Insertion Graft
Lateral crural insertion grafts are thin, flat cartilage grafts that are placed between the vestibular skin and the undersurface of the lower lateral crura medially and as an onlay graft laterally. This technique is useful in reshaping, repositioning, or reconstructing the lateral crura. Similar to the lateral crural strut graft, this technique can address lateral crura malposition, alar rim retraction, and recurvature of the lateral crura while minimizing dissection and decreasing risk of the graft mobilizing.
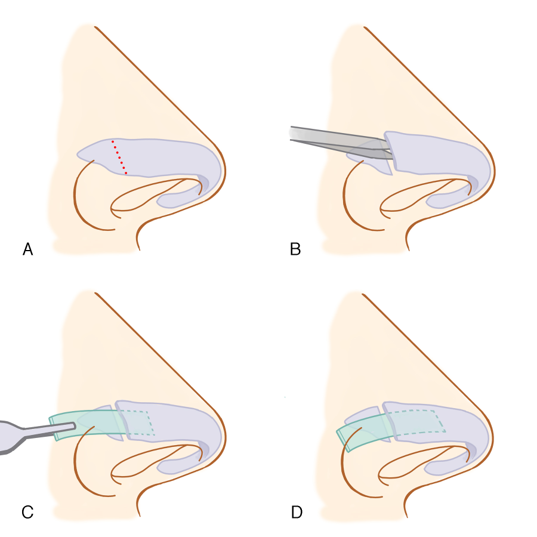
Technique
- The surgeon typically will perform lateral crural insertion grafts through an open rhinoplasty approach.
- The lateral crural insertion grafts are carved in a narrow, rectangular shape with dimensions measuring 15mm in length and 3-4 mm in width. Grafts should be thick enough to overcome negative inspiratory forces and thin enough to prevent excess intranasal bulk.
- After injecting 1% lidocaine with 1:100,000 epinephrine over the lateral crura and between the lateral crura and vestibular skin, a lateral crura cartilage incision is made dividing the lateral third of the lateral crura.
- Dissection is performed gently undermining the vestibular skin off the lateral crura medial to the cartilage incision. Vestibular skin is elevated from the cephalic border to the caudal border of the lateral crura approximately 4mm medially.
- In cases of severe alar collapse, retraction, or lateral crural malposition, the lateral crura are completely released laterally. A pocket may be dissected laterally over the pyriform aperture for placement of the lateral crural strut graft.
- The graft is inserted in the medial pocket under the lateral crura and placed over the lateral portion of the lateral crura. The graft is secured with 2-3 mattress sutures. The lateral end of the strut graft is placed caudal to the alar groove.

Limitations
- Requires careful dissection under the lateral crura
- Division of the lateral crura can weaken the intrinsic strength of native cartilage.
- Risk for asymmetry, especially with full release of the lateral crura. This is often not indicated.
Alar Rim Grafts
Alar rim grafts are thin, nonanatomic cartilage grafts inserted in a subcutaneous pocket along the alar margin. This technique is useful to soften the transition from tip to alar lobule improving the alar margin contour and provide alar support to prevent alar retraction. Alar rim grafts are useful in patients with cephalic malposition of the lower lateral cartilages, alar retraction, alar flare, or alar collapse.
Technique3
- The surgeon may perform alar rim grafts through an open or closed rhinoplasty approach.
- The alar rim grafts are carved in a narrow rectangular shape with dimensions measuring 15-25 mm in length and 2-3 mm in width adjusting the size of the graft depending on the severity of collapse and thickness of skin. Edges should be beveled to improve contour.
- After injecting local 1% lidocaine with 1:100,000 epinephrine at the alar margin, a marginal incision is performed and the rim is everted with a double prong skin hook.
- A precise tunnel is dissected at the alar margin extending to the alar base. The pocket should be tight fitting to minimize the risk of migration.
- A suture is placed around the alar rim graft to secure the graft without fracturing the cartilage. The graft may also be fixated to the dome region.
Limitations
- May not be effective for more severe cases of alar notching or retraction
- Requires adequate vestibular skin lining and elasticity
- Does not address significant nasal valve collapse
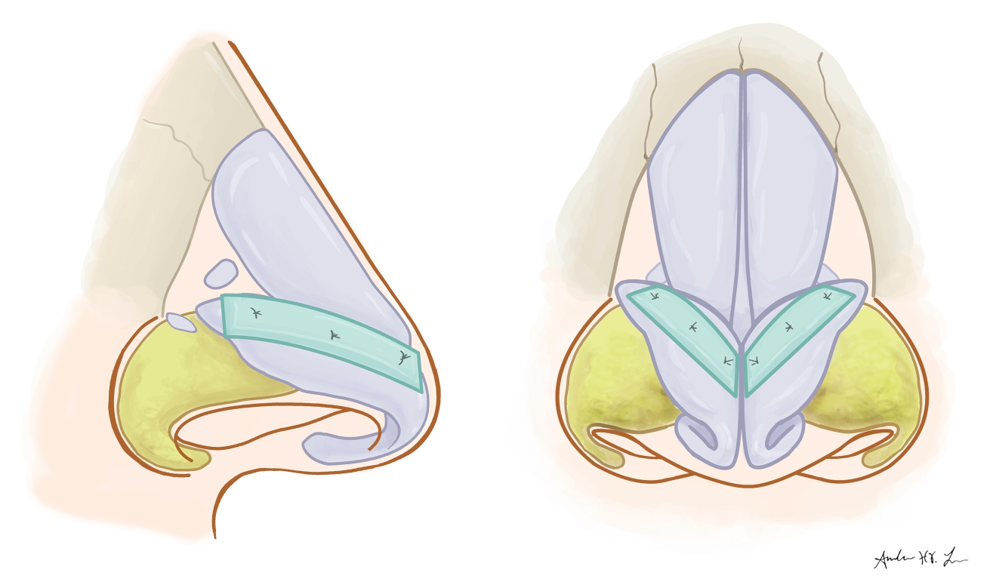
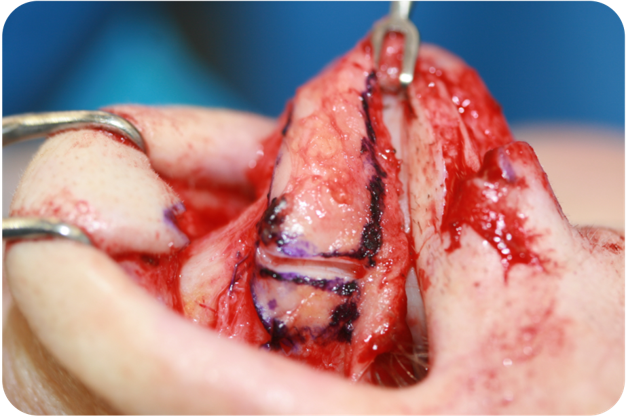
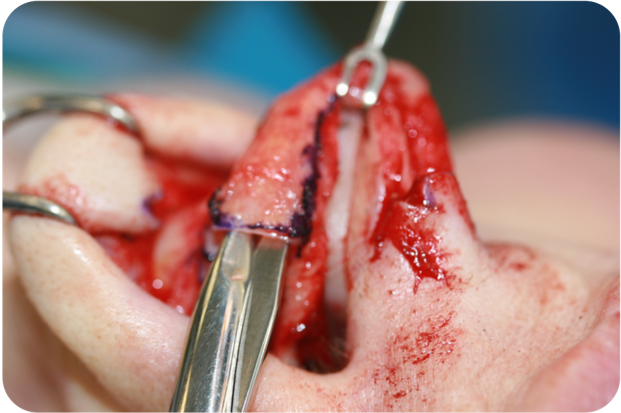
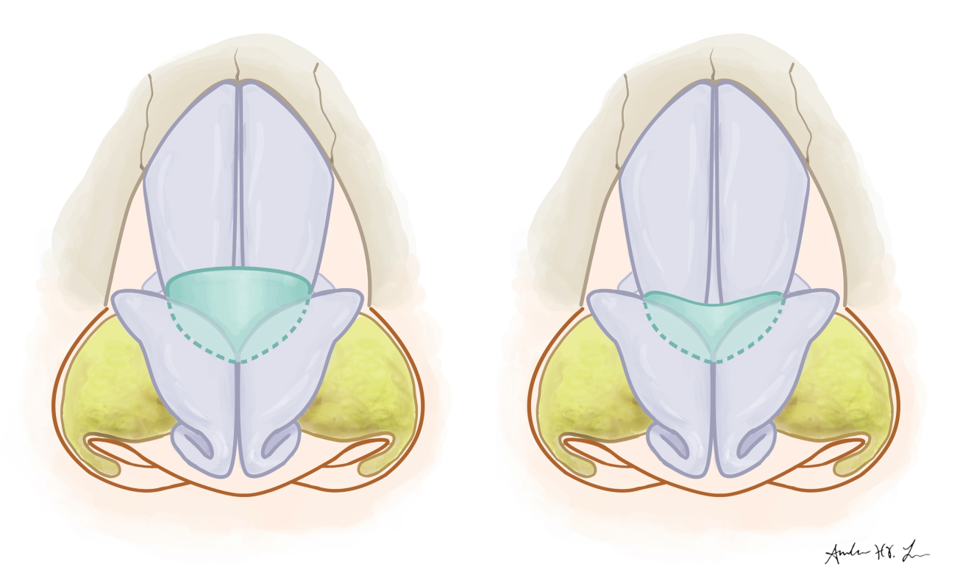
Cephalic Turn-in Flap
The cephalic turn-in flap serves as an alternative to the lower lateral cartilage cephalic trim reductive technique. In performing the cephalic turn-in flap, the cephalic portion of the lateral crura is scored and folded under the caudal portion of the lateral crura. This technique is useful in achieving aesthetic goals while reinforcing the caudal lateral crura. Additionally, the cephalic turn-in flap can reduce tip volume and narrow the tip defining point without the need for additional cartilage grafting. Patients with wide lateral crura and weak cartilages are good candidates for this technique.
Technique4
- The surgeon typically will perform cephalic turn-in flap through an open rhinoplasty approach.
- After injecting 1% lidocaine with 1:100,000 epinephrine at the surgical site, the entire lower lateral cartilages are exposed during the open approach.
- The lateral crura are measured and marked while preserving at least 8mm of cartilage caudally. The cartilage is scored along the marked line for the cephalic portion to be folded.
- The nasal mucosa and vestibular skin is dissected free from the internal surface of the lateral crura.
- The cephalic lateral crura is turned- in under the caudal portion of the lateral crura. Less commonly, the cartilage can be folded on top of the caudal lateral crura.
- The cephalic portion is sutured to the lateral crura with 2-3 mattress sutures.
Limitations
- Cannot be used in individuals without sufficient lateral crura to turn in
- Will not correct significant nasal valve collapse
- May not provide sufficient structural support compared to other alar support techniques
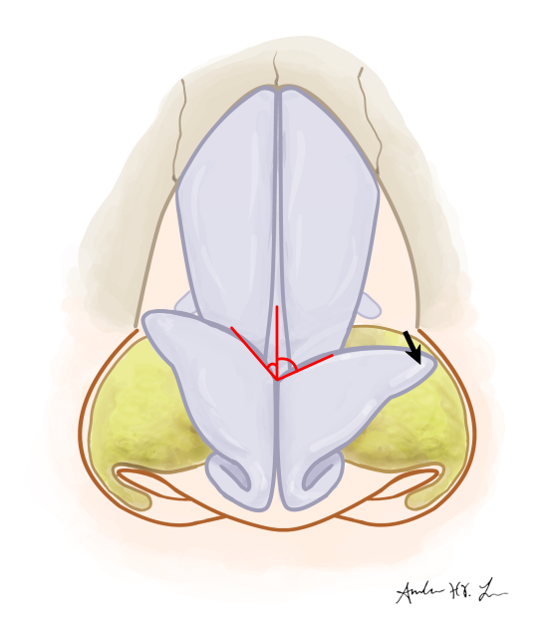
Butterfly Graft
The butterfly graft is a triangular cartilage placed over the caudal upper lateral cartilages and under the cephalic lower lateral cartilages. This technique is useful in stenting open the upper and lower lateral cartilages and increasing the angle of the internal nasal valve. A modified butterfly graft has been described to reduce the supratip visibility of the graft.
Technique5,6
- The surgeon can perform the butterfly graft via an open or closed rhinoplasty approach.
- The cartilage graft is commonly harvested from auricular cartilage utilizing the smooth, curved ascending portion or “shoulder” of the conchal bowl. The graft is carved to the dimensions of 25 mm in length and 12 mm in width. The modified butterfly graft is 35 mm in length and 9 mm in width. The graft will taper in thickness with the graft being thinner cephalically for a more natural dorsal contour.
- After injecting 1% lidocaine with 1:100,000 epinephrine at the surgical site, the upper and lower lateral cartilages are exposed.
- The vestibular skin is dissected free from the cephalic lower lateral cartilage. Resection of a small amount of dorsal septal cartilage can be useful to create space for the graft.
- The graft is inserted into the pocket under the cephalic lower lateral cartilage and on top of the caudal upper lateral cartilage. The modified butterfly graft will extend laterally just over the pyriform aperture.
- The butterfly graft is now sutured to the cephalic portion of the lower lateral cartilages laterally.
Limitations
- Supratip fillness and often visible
- Limited effect on external valve
- Donor site morbidity
Suture Techniques
Lateral Crura Repositioning
Lateral crura repositioning involves releasing the lateral crura of the lower lateral cartilages and suturing the cartilage in a more caudal position. This technique is useful in addressing tip bulbosity, cephalically malpositioned lower lateral cartilages, and alar base asymmetries. This technique can use a lateral crural strut graft if more structural support is required.
Technique7
- The surgeon can perform lateral crura repositioning through an open or closed rhinoplasty approach.
- After injecting 1% lidocaine with 1:100,000 epinephrine between the lateral crura and vestibular skin, dissection is performed gently undermining the vestibular skin off the lateral crura. Additionally, the lower lateral cartilages is released from the upper lateral cartilage.
- With the latera crura free, the surgeon can visualize the ideal position of the cartilage. Additionally, any mild asymmetries or deformities can be addressed with intradomal suturing. If more severe, a structural cartilage graft be necessary.
- A precise subcutaneous pocket is dissected at the anticipated ideal lateral crura position, which is typically more caudal.
- The lateral crura is inserted into the pocket and sutured in place to secure the crura
- A bolster or splint at the lateral nasal wall can be useful to maintain the positioning and reduce dead space.

Limitations
- Must be careful to not advance the lateral crura too laterally and consequently shorten the nasal tripod
- For major corrections, will often require a structural cartilage graft, such as the a lateral crural strut
- Limited correction of intrinsic cartilage deformities or severe alar retraction
Lateral Crura Mattress Suture
The lateral crura mattress suture (or Gruber suture) is a technique used to flatten and straighten the lateral crura of the lower lateral cartilages. This technique is useful in correcting convexity of the lateral crura resulting in a broad nasal tip.
Technique8
- The surgeon can perform lateral crura mattress suture can be performed via an open or closed rhinoplasty approach.
- The lateral crura must be less than 10 mm and ideally 6mm in width to optimize the effectiveness of the suture technique.
- After injecting 1% lidocaine with 1:100,000 epinephrine at the surgical site, the lower lateral cartilages are exposed.
- The suture needle is passed in one bite from inferior to superior, perpendicular to the long axis of the lateral crus, at the site of most prominent convexity. A second pass is made approximately 5 – 6 mm away medially in the parallel direction as the initial pass going from superior to inferior.
- The knot is carefully tightened while appreciating the flattening of lateral crus.
- This can be performed multiple times as needed to flatten other areas of convexity.
Limitations
- May not correct severe asymmetries or deformities
- Will not address significant nasal valve collapse
Lateral Crura Tensioning Suture
The lateral crura tensioning suture is a technique, similar to the lateral crural steal technique, used to reduce the length the lateral crura while lengthening the medial crura. This suture technique maintains the intrinsic lower lateral cartilage strength while stretching, tightening, and flattening the lateral crura. This technique is useful in patients with elongated lower lateral cartilages and can reduce the tip width, correct tip ptosis, and increase tip projection without the bulk of structural graft or requiring cartilage graft harvest.
Technique9
- The surgeon can perform lateral crura tensioning suture can be performed via an open or closed rhinoplasty approach.
- The lateral crura must remain tethered laterally to create sufficient tension.
- After injecting 1% lidocaine with 1:100,000 epinephrine at the surgical site, the lower lateral cartilages are exposed.
- The lower lateral cartilages are grasped to create a neodome at the desire location recruiting the lateral crura medially.
- The suture needle is passed in one bite from the lateral crura medially through the medial crura through the contralateral medial crura and out through the contralateral lateral crura. A second pass, approximately 2-3 mm superiorly, is performed in a mattress fashion through the lateral crura, medial crura and then contralateral medial crura and lateral crura.
- The knot is carefully tightened creating the neodome while stiffening and stretching the lateral crura bilaterally.
Limitations
- Risk for asymmetries or deformities between alae
- Tension can relax over time
- May not correct significant asymmetries or deformities
- Will not address significant nasal valve collapse
Additional Techniques
Internal V to Y / Z-plasty Advancement Flaps
In patients with a loss of nasal vestibular skin or scar contracture, structural cartilage graft or suture techniques alone may not be sufficient to provide alar support. The rhinoplasty surgeon may utilize techniques such as the internal V to Y or Z-plasty advancement flaps to release linear scar contracture at the ala and nasal sill. This can be useful in patients with acquired nostril stenosis either from prior rhinoplasty or other surgical resections, such as after skin or nasal cancer resection.
Technique
- A V to Y or Z –plasty is designed to recruit intranasal lining caudally towards the nostril sill
- Several flaps can be designed depending on the pattern of scarring or amount of skin loss.
- After injecting 1% lidocaine with 1:100,000 epinephrine at the surgical site, incision is made along the marked lines. Dissection is performed, often with excision of scar, to facilitate advancement of the skin flaps.
- After advancement of the flap, the skin is approximated and the flap is sutured in place with minimal tension.
Limitations
- Risk to for recurrence of scar or alar retraction
- Skin will contract with time
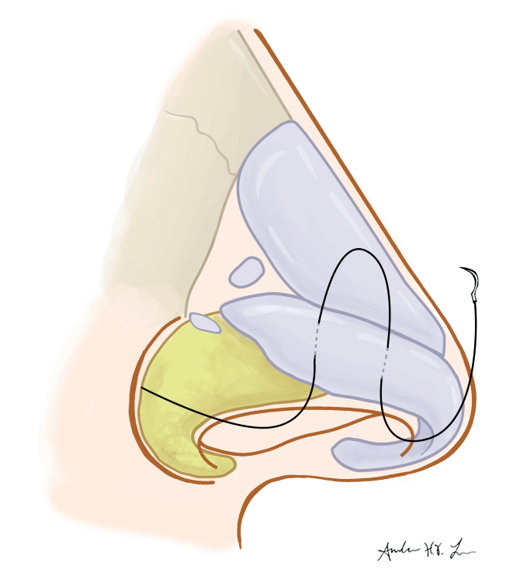
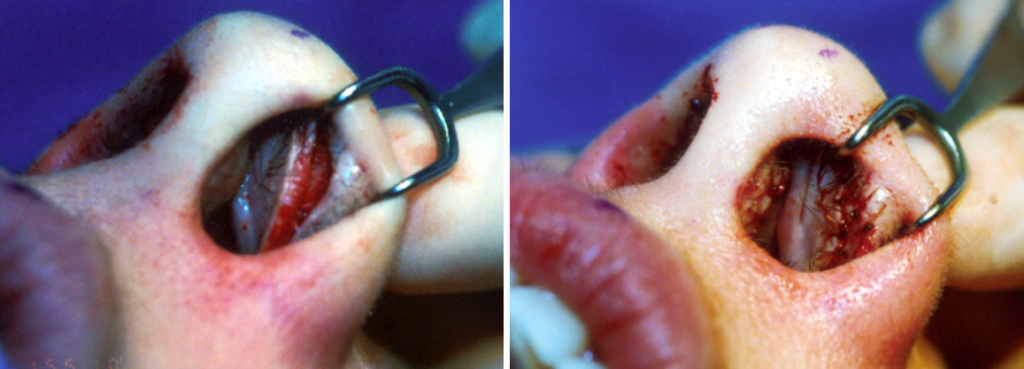
Auricular composite grafts
Auricular composite grafts are useful in patients with loss of vestibular skin and alar retraction, especially with overly resected lower lateral cartilages. This technique may be useful to replace the nasal lining and increase alar support while using the natural shape of the auricular cartilage.
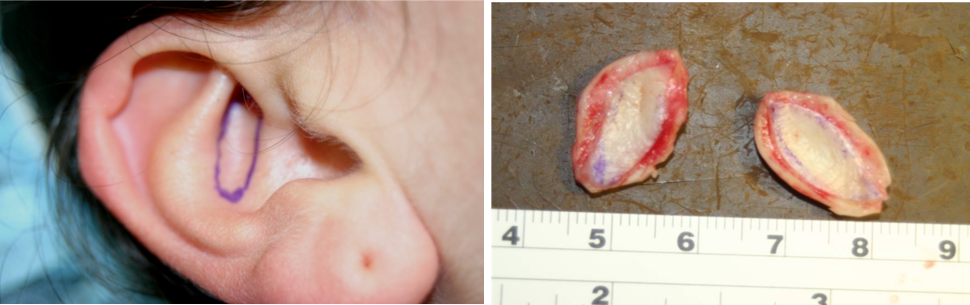
Technique10
- An auricular composite graft is harvested from the cymba concha as an ellipse tailoring the amount of skin and cartilage needed relative to the defect.
- Frequently, the cymba concha is utilized from the contralateral ear to optimize the contour of the graft.
- After injecting 1% lidocaine with 1:100,000 epinephrine at the surgical site, a marginal incision is made adjacent to the area of alar retraction or deficiency.
- A pocket is dissected releasing the vestibular skin and mobilizing the alar margin.
- The composite graft is placed with the concave side and skin facing intranasally and sutured in place.
- A bolster is useful to secure the graft. Ointment should be liberally applied during the patient’s postoperative course.
Limitations
- Risk for loss of composite graft
- Donor site morbidity
- Bulky
- May require revision surgery
Filler
Filler injections may be a useful technique in patients with nasal valve collapse who refuse surgery or did not have sufficient improvement after surgery.11 The filler can be used as a temporary measure to stiffen the external nasal valve and consequently resist collapse with inspiration. Good effect can be delivered using calcium hydroxyapatite. After injecting local anesthetics, small amounts of filler can be injected intranasally at the scroll region or alar rim. Care should be taken to avoid injecting too much filler, which could increase the weight of the ala and worsen collapse.
Absorbable Implant
Absorbable nasal implants composed of a cylindrical copolymer of poly(L-lactide) and poly(D-lactide) is a temporary nonsurgical option for patients with nasal valve stenosis.12 This is useful in patients who do not want or tolerate surgery, such as elderly patients or individuals with multiple medical comorbidities. Absorbable nasal implants are delivered over the lower and upper lateral cartilages to the frontal process of the maxilla with the goal to stiffen the underlying cartilages and resist inspiratory forces.
References
- Toriumi DM, Josen J, Weinberger M, Tardy ME. Use of alar batten grafts for correction of nasal valve collapse. Arch Otolaryngol – Head Neck Surg. 1997;123(8):802-808. doi:10.1001/archotol.1997.01900080034002
- Gunter JP, Friedman RM. Lateral crural strut graft: technique and clinical applications in rhinoplasty. Plast Reconstr Surg. 1997;99(4):943-945. doi:10.1097/00006534-199704000-00001
- Boahene KDO, Hilger PA. Alar Rim Grafting in Rhinoplasty: Indications, Technique, and Outcomes. Arch Facial Plast Surg. 2009;11(5):285-289. doi:10.1001/archfacial.2009.68
- Murakami CS, Barrera JE, Most SP. Preserving Structural Integrity of the Alar Cartilage in Aesthetic Rhinoplasty Using a Cephalic Turn-in Flap. Arch Facial Plast Surg. 2009;11(2):126-128. doi:10.1001/archfacial.2008.524
- Loyo M, Gerecci D, Mace JC, Barnes M, Liao S, Wang TD. Modifications to the Butterfly Graft Used to Treat Nasal Obstruction and Assessment of Visibility. JAMA Facial Plast Surg. 2016;18(6):436-440. doi:10.1001/jamafacial.2016.0681
- Clark JM, Cook TA. The “butterfly” graft in functional secondary rhinoplasty. Laryngoscope. 2002;112(11):1917-1925. doi:10.1097/00005537-200211000-00002
- Paquet CA, Choroomi S, Frankel AS. An Analysis of Lateral Crural Repositioning and Its Effect on Alar Rim Position. JAMA Facial Plast Surg. 2016;18(2):89-94. doi:10.1001/jamafacial.2015.1625
- Gruber RP, Peled A, Talley J. Mattress sutures to remove unwanted convexity and concavity of the nasal tip: 12-year follow-up. Aesthetic Surg J. 2015;35(1):20-27. doi:10.1093/asj/sju016
- Davis RE. Lateral crural tensioning for refinement of the wide and underprojected nasal tip: rethinking the lateral crural steal. Facial Plast Surg Clin North Am. 2015;23(1):23-53. doi:10.1016/j.fsc.2014.09.003
- Losquadro WD, Bared A, Toriumi DM. Correction of the retracted alar base. Facial Plast Surg. 2012;28(2):218-224. doi:10.1055/s-0032-1309302
- Kontis, Theda C, Lacombe VG. Cosmetic Injections Techniques.; 2013.
- San Nicolo M, Stelter K, Sadick H, Bas M, Berghaus A. A 2-Year Follow-up Study of an Absorbable Implant to Treat Nasal Valve Collapse. Facial Plast Surg. 2018;34(5):545-550. doi:10.1055/s-0038-1672213
Figure Legends
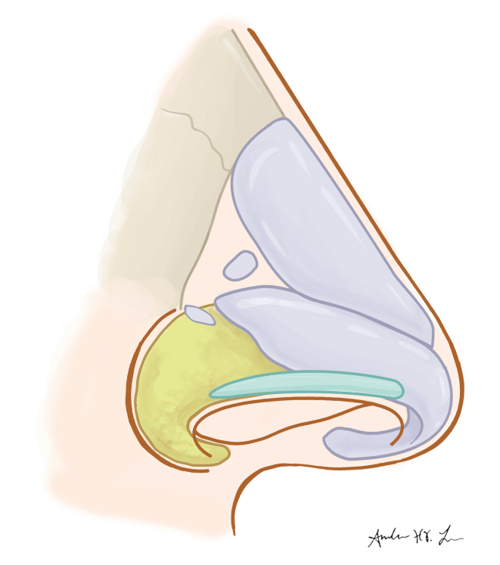
Figure 1. Nasal anatomy demonstrating upper and lower lateral cartilages
Figure 2. Alar Batten Graft.
Figure 3. Alar Batten Graft Placement.
Figure 4. Lateral Crural Strut Graft.
Figure 5. Lateral Crural Strut Graft Placement.
Figure 6. Lateral Crural Grafts.
Figure 7. Lateral Crural Insertion Graft.
Figure 8. Lateral Crural Insertion Graft Dissection and Placement.
Figure 9. Alar Rim Graft.
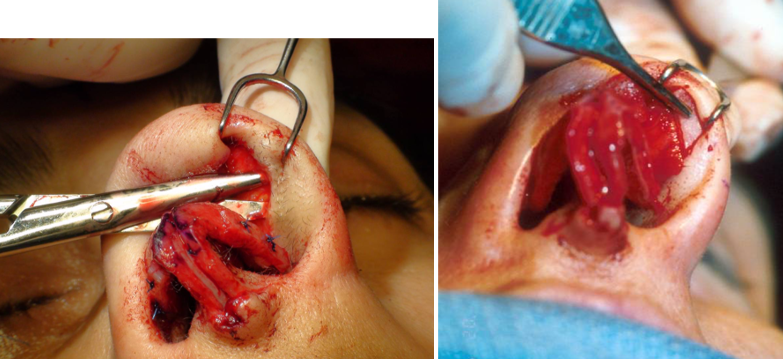
Figure 10. Alar Rim Graft Dissection and Placement.
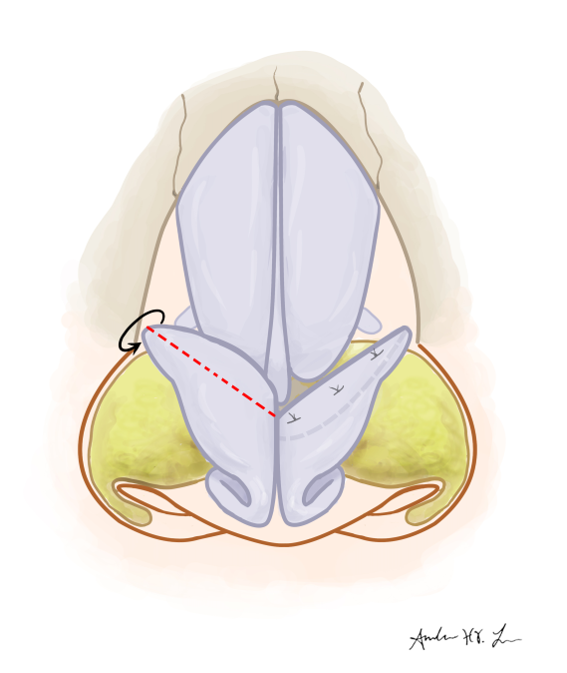
Figure 11. Cephalic Turn-in Flap.
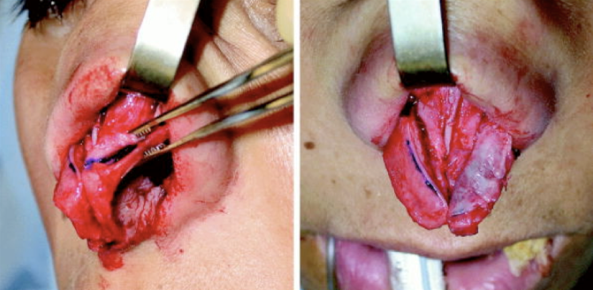
Figure 12. Cephalic Turn-in Flap Technique.
Figure 13. Butterfly Graft.
Figure 14. Lateral Crura Repositioning.
Figure 15. Lateral Crural Dissection.
Figure 16. Lateral Crura Mattress Suture.
Figure 17. Auricular Composite Graft Harvest.
Figure 18. Auricular Composite Graft Incision and Placement.
