Synopsis
Successful intervention for nasal tip ptosis begins with a careful history and comprehensive nasal analysis. Identification and correction of the etiology will allow for surgical modification with predictable and reliable outcomes. Adherence to the tripod theory principles will guide this successful surgical plan.
Introduction
A number of different etiologies may contribute to nasal tip ptosis. These include congenital structural deficiencies, loss of support with age, nasal trauma, and iatrogenic causes (following nasal surgery). When evaluating a patient with tip ptosis, it is essential that the surgeon identify the correct etiology to formulate the appropriate treatment plan. This chapter will outline nasal tip anatomy as well as diagnosis and surgical intervention for nasal tip ptosis.
Nasal Tip Anatomy
The relationship between the cartilaginous framework and overlying soft tissue dictates tip position. Major and minor tip support structures exist to maintain this position (Table 1). Major support mechanisms include the inherent strength and integrity of the lower cartilages, the attachment of the upper lateral cartilages to the lower cartilages (ie; scroll), the fibrous attachment between the footplate of the medial crura and the septum, and by some accounts, the septum. Minor support mechanisms consist of the interdomal ligament, nasal spine, sesamoid cartilages, attachment of the lower cartilages to the overlying soft tissue envelope, cartilaginous septal dorsum, and membranous septum.1
Table 1
| Major and Minor Tip Support Mechanisms |
| Major |
| Size, shape, and resilience of the lower cartilages |
| Attachment of the upper lateral cartilages to the lower cartilages |
| Medial crural footplate attachment to the caudal border of the quadrangular cartilage |
| Minor |
| Interdomal ligament spanning the paired domes of the lower cartilages |
| Nasal spine |
| Sesamoid cartilage complex as it extends the support of the lateral crura to the piriform aperture |
| Attachment of the lower cartilages to the overlying soft tissue envelope |
| Cartilaginous septal dorsum |
| Membranous septum |
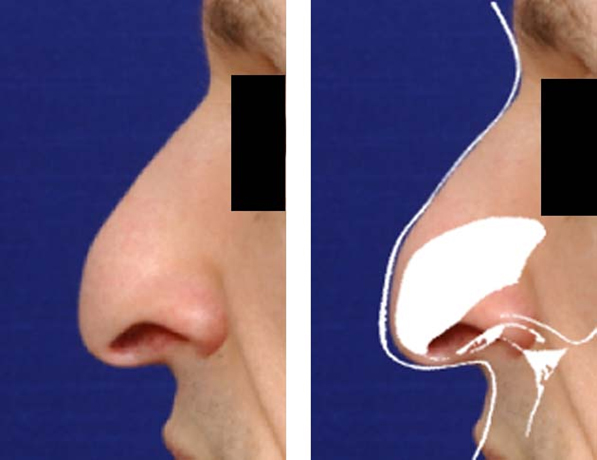
With the consideration of these anatomic tip support mechanisms, Anderson described the tripod theory.2 The tripod consists of three legs, the shorter paired medial crura and each lateral crus. The tripod rests on the anterior nasal spine and is supported medially by the membranous septum and laterally by the soft-tissue attachments to the upper lateral cartilages and the sesamoid cartilages as they extend to the piriform aperture. Modification of the tripod along the frontal plane leads to changes in nasal tip rotation and projection (Figure 1).
Figure 1: The tripod concept. The shortened medial crura relative to the lateral crura results in tip ptosis.
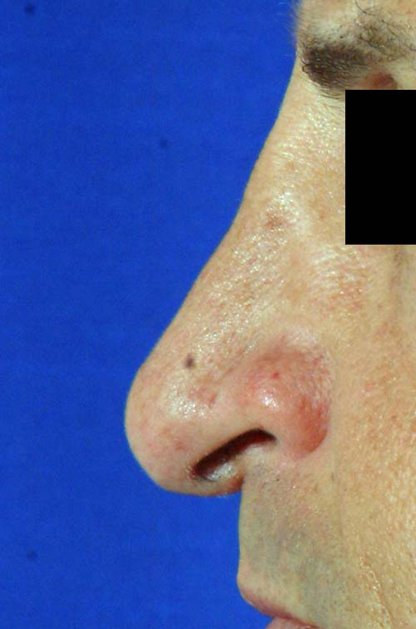
During the course of routine rhinoplasty, disruption/alteration of one or more of these support mechanisms may occur. Intra-operative recognition and correction of the surgically destabilized tip is critical to a successful outcome. In an unsupported tip, it is difficult to predict the forces of healing and wound contraction of the overlying soft tissue envelope, which often leads to an unfavorable result. Examples of rhinoplasty maneuvers leading to iatrogenic tip ptosis include: over-resection of the anterior septal angle or anterior nasal spine, destabilization of the medial crura, uncorrected complete transfixion incisions, and under-resection of excessively long lower lateral crura (Figure 2).
Figure 2: Iatrogenic tip ptosis from prior rhinoplasty. The tip is under-rotated and deprojected. Note the acute nasolabial angle.
Analysis and Diagnosis
A careful and comprehensive nasal analysis is essential to a successful rhinoplasty outcome. While the lateral view provides the most visible information concerning tip ptosis, a complete evaluation allows the surgeon to develop a global operative plan. This includes direct palpation, which adds insight concerning the size, shape, and resiliency of alar cartilages as well as their contribution to the patient’s tip support. For the revision patient, palpation helps elucidate the significance of scarring within the soft tissue envelope. During each examination, the surgeon should try to visualize the underlying anatomy of the lower cartilages and their relationship to the septum (Figure 3).
Figure 3: Note the narrow, weak paired medial crura in relationship to the lateral crura. Modification of this tripod directly affects rotation and projection.

In profile, the aesthetic ideal for tip rotation is a nasolabial angle of approximately 90-100° in men and 100-110° in women. This angle is determined by a line drawn from the anterior columella to the subnasale and the subnasale to the mucocutaneous border of the upper lip. Care must be taken in individuals with altered anatomy in this region, such as maxillary retrusion, prominence of the anterior nasal spine, or medial crural asymmetry, as the nasolabial angle may inaccurately assess true rotation. In these cases, measurement of the angle between a line along the long axis of the nostril and a line perpendicular to the Frankfort horizontal provides a more accurate estimate of rotation.3
Classically, the postrhinoplasty patient with tip ptosis suffers from deprojection, underrotation, and poor tip support. A cartilaginous or soft tissue pollybeak deformity may accompany and accentuate the ptosis. The cartilaginous pollybeak is the result of unanticipated loss of tip projection leading to a supratip prominence. Overreduction of the dorsum in a thick-skinned patient may lead to a soft tissue pollybeak because of an inability of the redundant tissue to contract over the cartilaginous framework.
The patient may complain of new onset nasal obstruction. Therefore, analysis must include an intranasal exam. Attention is directed at the position of the septum, size and position of the inferior turbinates, presence of lower cartilage recurvature, internal valve, external valve, and inter-valve area. Note is made of dynamic mobility of the nasal sidewall and its effect on the nasal valves.
Surgical Intervention
Often aesthetics as well as function are important to the ptotic tip patient. In the postrhinoplasty patient this is of particular significance as they may have lost both as the result of prior surgery. Optimal results are achieved when the result is anticipated and satisfying to the patient and surgeon. The patient should have a clear understanding of the surgeon’s perspective on their nasal anatomy and as well as the expected outcome.
A clear appreciation of the interplay of surface deformities and their underlying anatomic counterparts helps dictate a successful surgical plan that avoids landmines leading to a suboptimal result. For this reason, we advocate an open approach for the vast majority of these patients. This allows the surgeon to accurately diagnose and precisely correct the deformity.
A gullwing or inverted “V” transcolumellar incision is used to access the tip. Dissection proceeds in a subnasal superficial musculoaponeurotic system (SMAS) plane with skeletonized of the crural cartilages. In the revision patient, it is essential to identify this plane and fully release the subcutaneous fibrous scar tissue to mobilize the tip and reposition the cartilage.
With the upper and lower cartilages in full view, the surgeon may identify the etiology of tip ptosis (Figure 4). Recalling the principles of the tripod theory, the tip is surgically repositioned. Where possible, attempts are made to employ non-destructive, cartilage-preserving techniques. Some common surgical maneuvers used to correct tip ptosis include the tongue-in-groove setback, caudal extension graft, columellar strut, tip graft, and lateral crural repositioning techniques.4
Figure 4: Intraoperative tip destabilization prior to repositioning. Note the cephalically oriented lower cartilages.

Tongue-in-Groove Repositioning of the Tip
This maneuver is used to reliably set tip projection and rotation.5 Following elevation of bilateral septal flaps through a hemitransfixion incision, an external approach to the nose is performed. With the domes retracted laterally, the anterior septal angle is identified and a pocket is created in continuity with the septal flaps inferior to the caudal septum. This allows mobilization of the medial crura in relationship to the caudal septum. The crura are repositioned and secured to the caudal aspect of the septum. This technique is most successful in the underrotated but adequately projected tip.6
Of note, this technique may result in setback of the medial crura. Thus, in cases of a short septum (e.g., the Asian nose) or baseline columellar retraction, a caudal extension graft may be used concomitantly.
Caudal Extension Graft
In revision patients with prior aggressive reduction of the caudal septum, tip support is lost with tip ptosis and columellar retraction. Caudal deficiencies may also be present to a lesser degree in the primary patient with ptosis. When available, a portion of quadrangular cartilage inferior and posterior to the dorsal and caudal struts is ideal for grafting material. In the postrhinoplasty patient with inadequate septal cartilage, autogenous rib is an alternative. After positioning the strut in the midline and suture securing it, a tongue-in-groove setback may be performed to precisely position the rotation and projection of the tip. Plumping grafts placed for premaxillary augmentation are used for deficiency at the nasolabial angle despite adequate tip position.
Columellar Strut
To correct for medial crural insufficiency, a columellar strut is employed. A precisely dissected pocket is created from the junction of the intermediate and medial crura down to the anterior nasal spine. The graft is obtained from quadrangular cartilage or rib and is suture secured to the medial crura posterior to the intermediate-medial crural junction to prevent alteration in the shape of the infratip lobule.
Tip Graft
For improved definition and support of the amorphous tip, a tip graft is often used. A shield-shaped graft is carved from quadrangular or auricular cartilage and placed adjacent to the caudal edge of the junction of the intermediate and medial crura. This resets the tip defining points and allows some projection and cephalic rotation of the tip. This technique may be combined with the aforementioned maneuvers to refine the final tip appearance and position. Caution is undertaken in thin-skinned individuals where the graft edges may appear as bossae. It is important to bevel these edges to prevent long-term contour irregularities.
Figure 5: Tip graft. Edges of the graft are beveled for optimal contour.

Lateral Crural Repositioning
Excessively long lateral crura may be amenable to the lateral crural overlay technique.7 The vestibular mucosa is carefully dissected from the undersurface of the mid-portion of the lateral crura. Approximately 10mm lateral to the dome, the crus is vertically divided. The dome is set to the desired position, and the crural segments are overlapped and secured with two trancartilaginous mattress sutures.
Figure 6a: Incision design for lateral crura overlay.

Figure 6b: Transection of the lateral crura. It is important to dissect free the underlying vestibular mucosa prior to cartilage incisions.
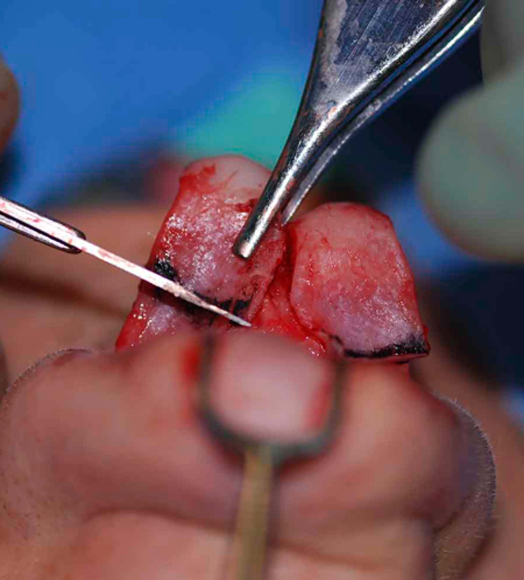
Figure 6c: Tip is set to desired rotation. Overlay of the cartilages is secured with 5-0 Prolene.

The lateral crural steal technique is an alternative to correct relative medial crural deficiency.8 Essentially, the medial crura are lengthened at the expense of the lateral crura. Approximately 5mm of vestibular mucosa is elevated beneath each of the domes. The lateral crus is advanced in a curvilinear fashion onto the medial crus and suture secured. Each dome is addressed individually. To further refine the tip, the domes are narrowed and set with a mattressed transdomal suture. The tip is repositioned in an anterosuperior direction, enhancing rotation and projection. The major advantage of this technique is cartilage preservation.
Summary
Successful intervention for nasal tip ptosis begins with a careful history and comprehensive nasal analysis. Identification and correction of the etiology will allow for surgical modification with predictable and reliable outcomes. Adherence to the tripod theory principles will guide this successful surgical plan.
References
- Toriumi DM. Rhinoplasty. In: Park S.S., ed. Facial plastic surgery: the essential guide, Thieme Medical Publishers New York 2005: 223-253.
- Anderson JR. The dynamics of rhinoplasty. In: Proceedings of the Ninth International Congress of Otolaryngology. Exerpta Medica International Congress Series, No. 206. Amsterdam: Elsevier Inc,; 1968. p. 708-10.
- Leach J. Aesthetics and the hispanic rhinoplasty. Laryngoscope 2002;112(11):1903-16.
- Konior RJ. The droopy nasal tip. Facial Plast Surg Clin N Am 2006;14:291-9.
- Kridel RW, Scott BA, Foda HM. The tongue-in-groove technique in septorhinoplasty. A 10-year experience. Arch Facial Plast Surg 1999;1(4):246-56.
- Foda HM. Management of the droopy tip: A comparison of three alar cartilage-modifying techniques. Plast Reconstr Surg2003;112:1408-17.
- Kridel RW, Konior RJ. Controlled nasal tip rotation via the lateral crural overlay technique. Otolaryngol Head Neck Surg1991;117:411-5.
- Kridel RW, Konior RJ, Shumrick KA, Wright WK. Advances in nasal tip surgery: The lateral crural steal. Arch Otolaryngol Head Neck Surg 1989;115:1206-12.
