1. Anatomy and Structure of the Nasal Tip
The nasal architecture is complex, and assessing its external appearance requires critical understanding of the underlying structure. Although the aesthetic goal of rhinoplasty surgeries sets the framework for the task at hand, the inherent anatomy often guides the operative technique1,2. Its composition of skin, fibrofatty soft tissue, bone and cartilage contribute to the gentle contour of the tip. In turn, slight imperfections in any part of the framework could disrupt the aesthetic balance. The nasal tip is a delicate primarily cartilaginous structure that provides definition to the nose, and can affect the overall aesthetic of the face. Traditional teaching has described the nasal tip and lower lateral cartilages in a 2-dimensional perspective; the structural support provided is characterized by nasal projection in a ventral-dorsal axis, and tip rotation and width in a cephalic-caudal axis.
The traditional understanding of the tip has since progressed and the tip has been redefined as a 3-dimensional structure with multiple subunits and axes that affect each other, even with small changes. The third dimension takes into consideration the lateral alar cephalocaudal dimension or alar rim position. This is often a challenging concept in nasal surgery and reconstruction.
The nasal tip consists of the lobule, columella, vestibules, alar bases, alar sidewalls and nasal floors3. Or more simply, it is sometimes described 3 subunits: the columella, ala and lobule3,4. Surgery of the nasal tip is commonly recognized as the most complex portion of rhinoplasty. The ultimate goal is to create an appropriately projected, rotated, and stable tip, that is symmetric and harmonious with itself and the rest of the nose and face.
The ideal described nasal length is between 45-49mm, defined at the distance from the nasion to the nasal tip. Byrd described the ideal nasal length as measured from the glabella to the subnasale to be equal to two-thirds the height of the midface5. Other methods of nasal length take into account not only the length but the height, tip projection, and angulation. Crumley discusses the nasal profile as a 3-4-5 right triangle whereas Goode’s method relates tip projection to nasal length as a ratio of 0.55-0.606,7. When assessing the nasal profile, the nasofacial angle is approximately 36 degrees, the nasofrontal angle 115-135 degrees, and the nasolabial angle is 105-115 degrees in females and 90-105 degrees in males.
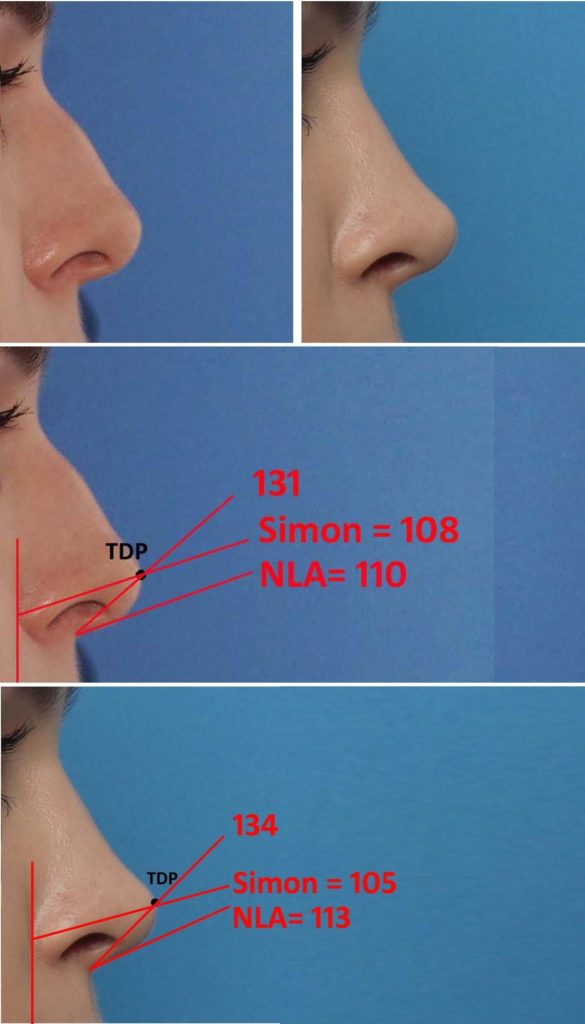
The width of the nostril measured from alar crease to alar crease, should be equal to the height measured from the subnasale to the tip defining point, with a 2:1 ratio between the nostril to infralobule7. The ideal nostril shape should be at a 45 degree angle, elliptical in shape measured from the lateral border. The frontal view of the nose emanates from the medial brows and extends to the dorsal esthetic line made up of the tip-defining points. The frontal and basal views provide the best perspective to evaluate the shape, while lateral and basal views are best for position and projection. Cephalad to the nasal tip is the supratip break where the contour lines of the nasal dorsum rise toward the tip-defining points. Despite the nasal tip dictating the projection and rotation of the nose, its numerous components are important in tip analysis. Although calculations and measurements can generalize an ideal aesthetic, they are rarely validated in studies. Attractiveness and beauty lie on a spectrum and is transient with the generation, different ethnicities and cultures and therefore is a collaboration between the surgeon and patient.
Alar Cartilages
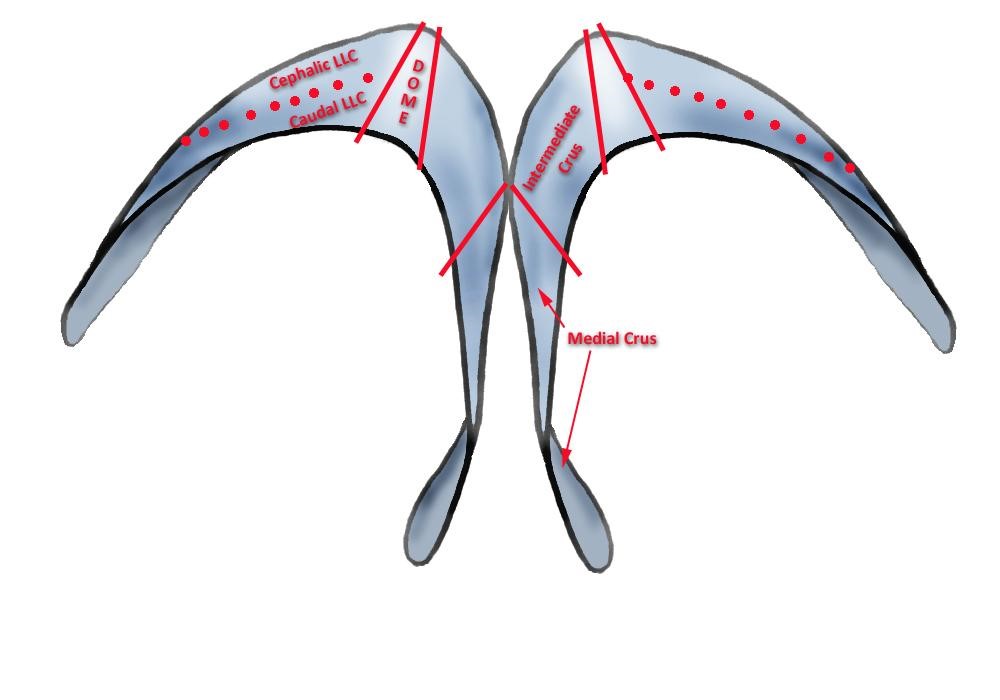
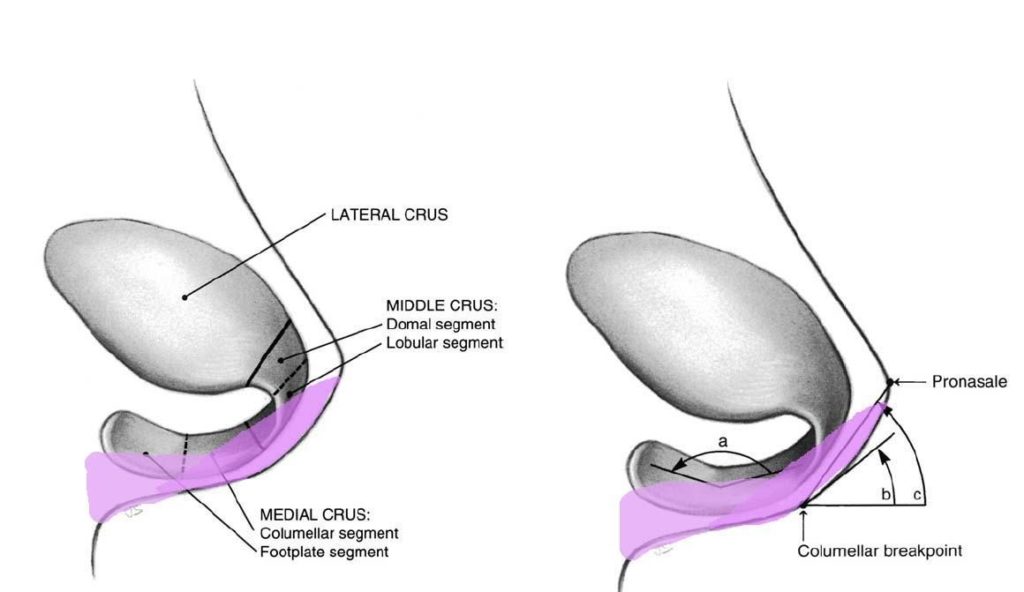
The alar cartilages were traditionally thought to be comprised of a medial and lateral crural connected by an anatomical domal segment8. It wasn’t until Sheen and Sheen through cadaveric work introduced the middle (intermediate) crus as an important component of the lower lateral cartilages that define the nasal tip that our understanding of alar evolved into three complex components9.
Medial Crus
The medial crus are comprised of both the footplate and columellar segment and act as the pillar of the nose. The columella begins at the distal end of the footplate and ends where it meets at the middle crus with the columellar lobule junction. This is the breakpoint that marks the transition from the nasal base to the lobule3. At the columella, the medial crura above the footplates should be tightly opposed (2-3mm apart) and straight in both the craniocaudal and antero-posterior planes10. As the medial crura transition in the intermediate crura towards the dome, they should begin to gently separate and curve cephalically3,10. This slight framework change results in the double break when viewed on profile and determines the volume of the infratip lobule from the front. They are typically one of three shapes: straight, divergent symmetrical curve or reciprocal curve.
Middle Crus
The middle crus are divided into the lobular and domal segment and begins at the columellar lobule junction and ends at the medial portion of the lateral crus. Within the middle crus are the genus which mark out the domal notch or soft tissue triangles of the tip. These tip defining points can be thought of as two equilateral triangles which extend from the supratip region cephalically the columellar lobule angle caudally11–13. The cartilage over the tip defining points allows for an external light reflex that affects the perceived tip shape. The lobular segment and its length, shape, and angulation largely determines the infratip lobule shape, protrusion and height. The domal component which is the most delicate portion, can vary in degrees of concavity and convexity to give an aesthetic nose3,4. It extends from the medial genu at the infralobular segment to the lateral genu at the extent of the lateral crura. The domal junction found at the transition from middle to lateral crus is the critical landmark for a refined tip. The domes themselves should be triangular in shape, with the apex at the cephalic edge3.
Lateral Crus
The lateral crus make up the alar sidewall and is the largest component of the lobule. It is composed of the body which begins at the domal junction and ends with the accessory chain that makes up the narial ring14. The lateral crus determine largely the lobule shape, size and position. The scroll area is located at the junction of the cephalic edge of the lateral crus and the caudal edge of the upper lateral cartilage and any overlap gives support to the internal nasal valve.
2. Reasons for Poor Nasal Tip Aesthetics
The nasal tip is a critical part of rhinoplasty and can lead to poor aesthetic results if not performed correctly. The aesthetically balanced nasal tip must integrate shadows, lines and highlights over its breakpoints and contours that can be conceptualized as a series of geometric forms15. Multiple studies have cited asymmetry to be a common problem in rhinoplasty patients with more than half presenting with asymmetry of the lower lateral cartilages16,17. Any distortion of symmetry can offset this harmonious balance and lead to a poor tip aesthetic.
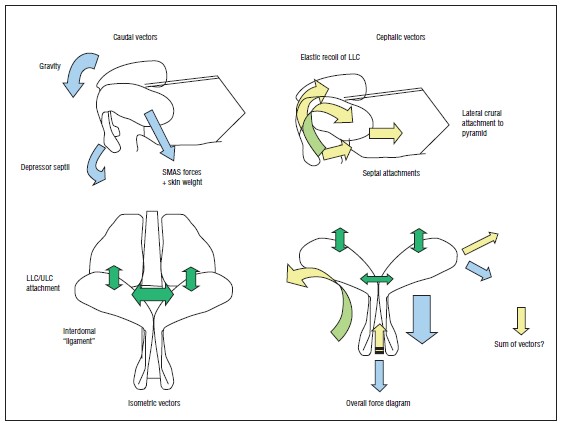
The cartilaginous framework of the nasal tip has been historically described as dependent on major and minor tip support mechanisms. It is the opinion of the senior author, however, that this distinction has no significance for modern Rhinoplasty techniques. Rather, central and lateral stabilization through rigid cartilaginous framework abutting a centralized caudal septum is the stabilization model of choice. The nasal tip, then acts as a cantilevered spring with its stabilization point at the base of the columella.
Asymmetries
The nasal septum is the center point for attachment of the upper and lower lateral cartilages. It can affect the lower lateral cartilages and nasal tip by its position, strength and resiliency in supporting these structures. The caudal border of the quadrangular cartilage is the most influential portion for tip symmetry and, when deviated, is a common cause of nasal tip deviation. Due to its relative position to its structural attachments, even the slightest deflection can unbalance the aesthetics of the nose. The caudal septum, while not having definable ligaments, still provides important foundational support for the tip.
The anterior septal angle influences the rotation and projection of the nasal tip and can alter both the tip defining points independent of one another. Establishing a midline reference can help the surgeon in aligning a crooked nose or deviated tip. The central incisors or anterior nasal spine are reliable reference points but can also be deviated in some cases. The anterior nasal spine, although not as common, may also be off midline leading to tip asymmetry and deviation. As the point of attachment for the caudal septum and columella soft tissues, this should be taken into consideration when analyzing the nose for asymmetries. Septal deviations are crucial to correct first before tackling other complex tip work.
Dome Shape
Domal shape and asymmetry refers to the degree of columellar and alar show, caudal septal excess/insufficiency, and overall morphology. Diagnosis should include static and animated views to view dynamic ptosis. Dome asymmetry may be inherent or iatrogenic after primary rhinoplasty. The goal of tip and domal refinement is to create a slender and refined lobule with 2 tip defining points aligned in the same vertical plane. Oftentimes, the actual orientation and the integrity of the dome cartilages are not compromised, but there is a problem with their relationship to other structures of the nose. This leads to a variety of asymmetrical presentations of the nasal domes. The tip may be broad, bifid, amorphous, bulbous, boxy or distinctly asymmetric. Repositioning techniques to achieve a desired nasal dome include cartilage reshaping, suturing and resecting. In recent years, preservation of nasal tip cartilages has become more popular as over resection can lead to unfavorable results.
Lateral crural position – caudal versus cephalic border
The lateral crus have been shown to be variable in size and length. The cephalic portion of the lateral crus transition to the upper lateral cartilages at the scroll region. This S-shaped fibrous junction is where the dynamic nasal tip becomes the static nasal body and is important in that it harbors a portion of internal nasal valve. The lateral extension of the caudal lateral crus parallels the nostril rim before turning cephalically. Any malposition of the lateral crus can cause shape deformities in the lower lateral cartilages9,18. The shape of the lateral crura has been described as one of 6 types: smooth convex, convex-concave, concave-convex, concave-convex-concave, concave and completely irregular3. The ideal shape of the lateral crura should be slightly concave near the anterior one-third and flat in the posterior two-thirds. Malposition of the lateral crura was first described by Sheen in 1978, and is referred to as cephalic placement of the lateral crura19. The medial and lateral canthus on the ipsilateral side can be used as reference points for mispositioning of the lateral crura. Cephalically positioned lateral crura are typically 30° from midline and directed toward the medial canthi. A normally positioned orthotopic lateral crura in comparison diverges at an angle of 45° or more from midline and directed toward the ipsilateral lateral canthi14,19. Asymmetries in the lateral crura that are due to cephalic positioning has been cited in various conditions such as external valve incompetence, nasal tip parenthesis deformity, long alar creases and nasal tip boxiness19,20. Alar malposition has been detected in 68% of patients undergoing primary rhinoplasty and 87% of his patients undergoing secondary rhinoplasty and has been concluded as the reason for cosmetic deformities such as a bulbous and boxy tip in addition to functional deficits20.
The caudal border of the lateral crus is best evaluated for symmetry in the basal view to evaluate the alar rim for asymmetry21. The base view should form an isosceles triangle lines drawn to connect the alar facial grooves and nasal tip with a tip-lobule-to-columella ratio should be 1:2. The alar base is dynamic and comprised of four different types of muscles which include depressors, elevators, compressors, and dilators that are critical in nasal base positioning. Two critical muscles being the levator labii alaque nasi and the dilatator naris. The dilatator naris inserts over the alar skin from its origin at the lateral crus of the lower lateral cartilage and dilates the nostrils. The levator labii superioris alaeque acts by pulling the ala superiomedially22. Both act to aid in dilation of the nostrils to improve airflow and breathing. It is part of the external nasal valve and vestibule, playing a critical role in nasal function and breathing. Profile views of the caudal border can be used to assess alar-columellar disproportions23. The ideal nostril is ovoid in shape with the alar rim giving its gentle curve to create the superior border, and the columella giving 2-3mm of maximal show24. Alar notching or asymmetries can be a cause of primary or secondary rhinoplasty alar cartilage, skin or mucosa excision or alar division. A columella-to-nostril axis distance of less than 1mm is consistent with columellar retraction whereas a distance of 2 mm or greater is consistent with a hanging columella. Acquired disproportions can be due to the inherent shape and integrity of the lateral crus. Asymmetry needs to be determined whether the cause is from the ala or the columella, as both can be the cause of disproportions but are corrected differently surgically.
3. Reasons for Desirable Tip Aesthetics
Symmetry
Facial symmetry plays a role in the balance and proportion of appearance. A crucial component of this is nasal symmetry, particularly with regards to the tip. The midline placement of the septum and its fibrinous and ligamentous attachments to the lower lateral cartilages create a center focus point in nasal and facial balance. A midline septum allows the supportive cartilages of the nasal tip to be appropriately positioned. 31
Triangular Dome Configuration
The domes of the nasal tip ideally harbor a triangular configuration, with the apex at the cephalic edge. This creates a caudal flare, the angle of which should be 25-30 degrees when compared to the cephalic width. It is important to pay attention to the positioning of the dome and its degree of rotation and projection and its relationship with the medial and lateral crura. The gentle curvature of the caudal aspect of the domes allows the caudal edge of the lower lateral cartilage to stay slightly more projected than the cephalic one, helping to set the lateral crural resting angle at an optimal 100-120 degrees of midline.
Soft Transitions
Since light interplay on the soft tissues is the ultimate result of these cartilages, this configuration will produce optimal aesthetics. The higher the tissue, the more reflective it will be of overhead light. With the caudal border of the domes being highest, it will be the brightest spot on the nose. As one moves cephalically into less projected areas of the tip, a gradual increase in shadowing will occur. A flat infratip cannot catch light and will lie, along with the columella, in a relative area of shadow, defining the lower vertical limit of the tip. Provided the cephalic dome lies above the anterior septal angle, a shadow break at the supratip/profile will finish the topography of the nasal tip and provide a defined upper vertical limit of the tip. In all the tip should have a triangular or diamond shaped area of greatest prominence. When taken together, these light effects will cause a nasal tip to be “refined.”
Caudal Border Prominence
The domes themselves should be tightly opposed cephalically and separated a variable amount caudally. Dome divergence allows for shortening of the cephalic edge and allows for increased length of the caudal edge. This caudal length “excess” allows the intrinsic cartilage spring to unfurl more, projecting the caudal edge or both the domes and the crurae. This helps to maintain airway patency and allow for a relative setback of supratip volume.

4. Measureable parameters for optimal nasal tip aesthetics
Dome divergence
The optimal divergence (Angle of Dome Divergence) of the 2 domes lies in the 50-70 degree range when viewed from above. The physical separation of the caudal domes should be somewhere in the 4-6mm range. This allows for a relative shortening of the cephalic edge from attachment point to center, when compared to the caudal edge, which should be longer. The dome angle, which is evaluated on a basal view evaluates the angle of divergence from a different perspective. This measurement is approximately 25-40 degrees. The caudal flare angle, which compares the width of the dome from cephalic to caudal border should be 25-30 degrees.
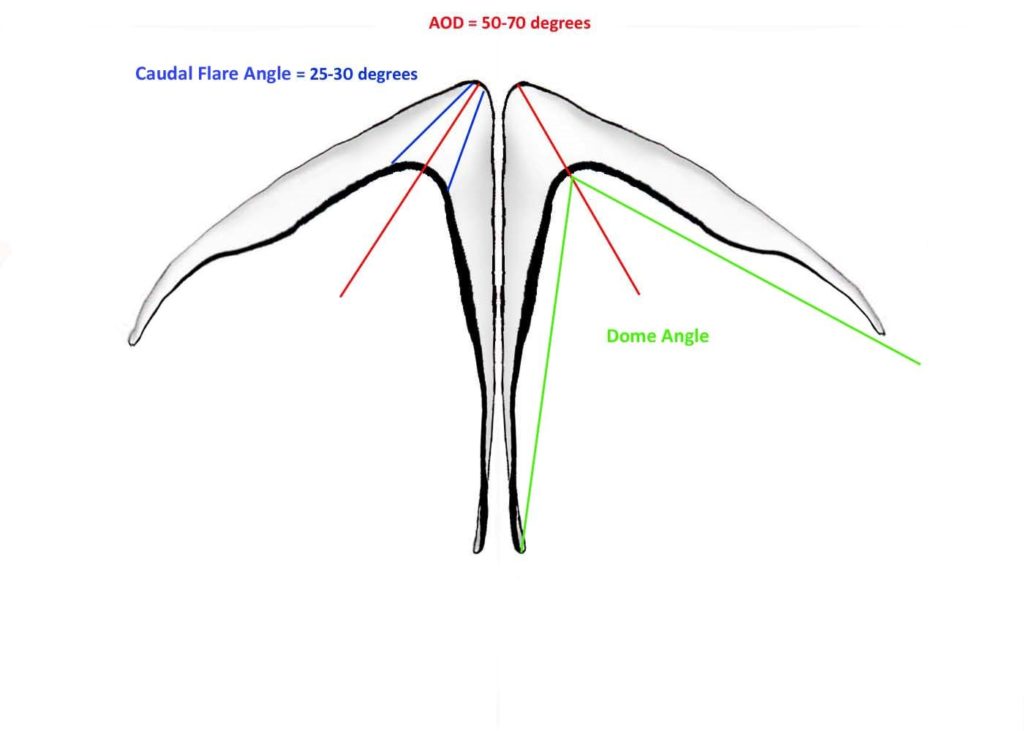
Figure: Angle of Dome Divergence versus Dome Angle versus Caudal Flare Angle.
Lateral Crural flattening/spin: 100-120 degrees from vertical axis
As described by Cakir et al in several publications, the lateral crural resting angle, is the angle of the short axis of the lateral crus in relation to the upper lateral cartilage Long axis. This angle demonstrates the flattening of the lateral crus in relation to the vertical plane in the nose. The caudal edge of the lateral crus is therefore more projected than the cephalic edge. This creates a surface shadow that gradually increases as one travels from the free nostril edge into the supratip.27, 28

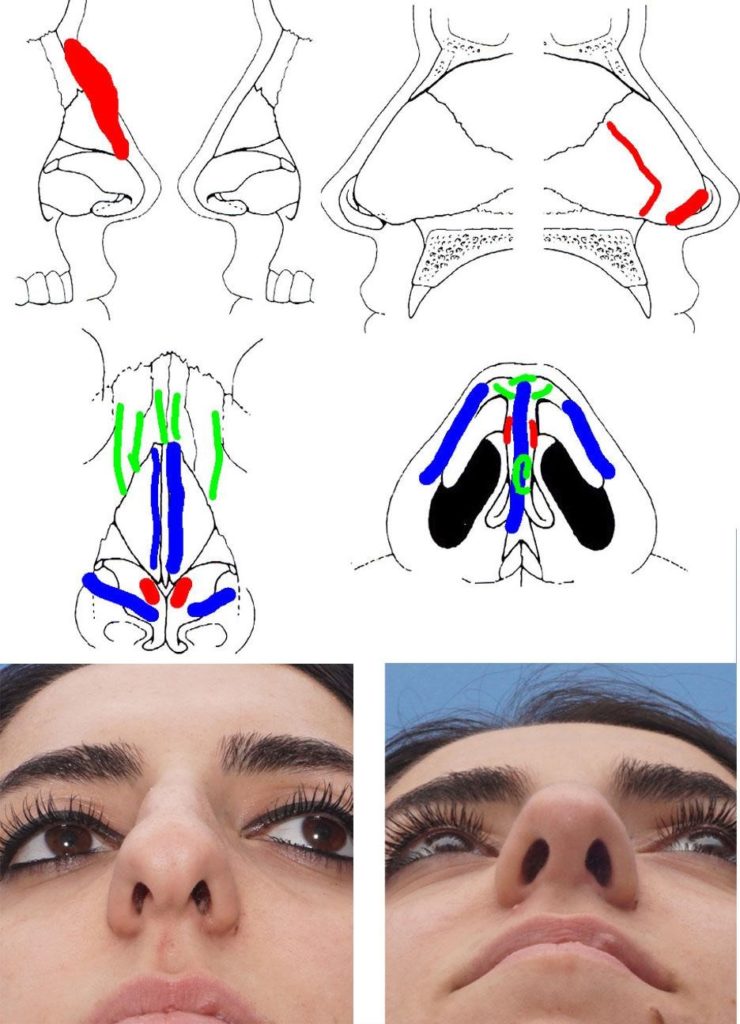
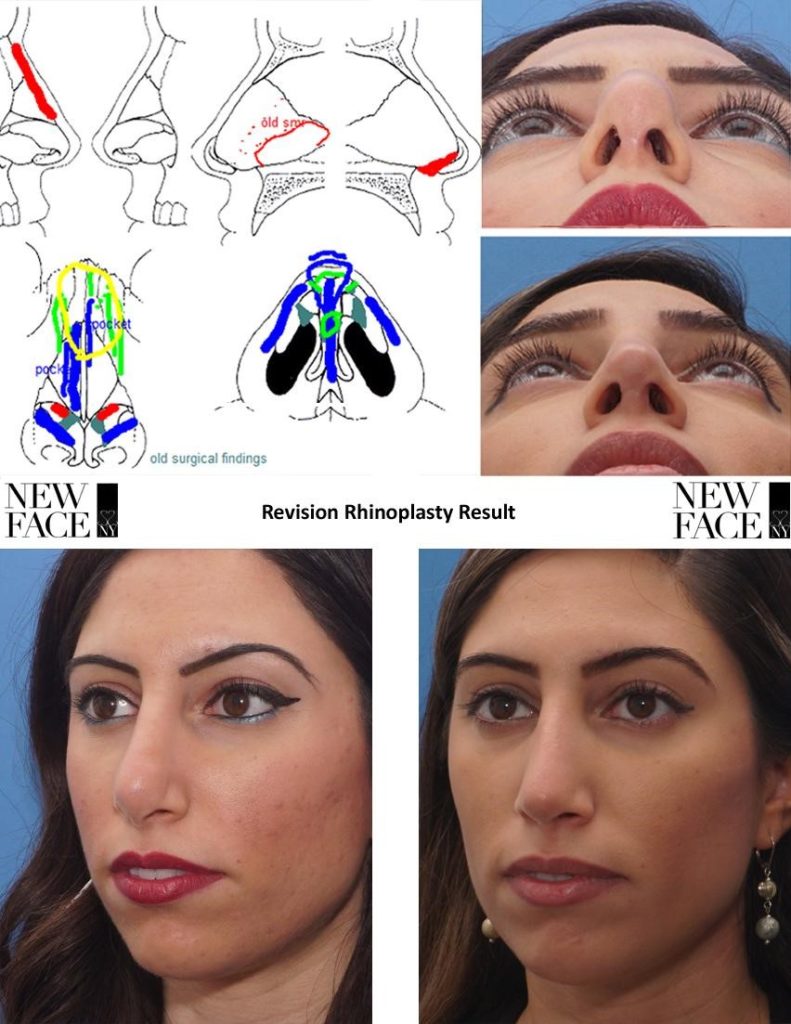
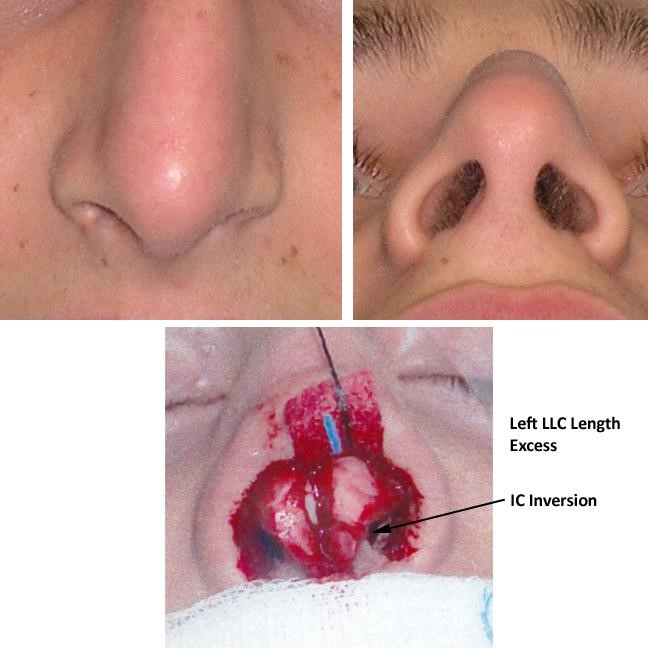
Figure: Primary Rhinoplasty showing excess length and curviture of the intermediate crus, causing a significant fullness of the infratip lobule. Shortening of the intermediate crura was a critical part of the operative plan. This intervention did not cause counter-rotation, since the domes were already cephalically placed on the lower lateral cartilages.
Degree of double break
The double break signifies the junction of the medial and intermediate crus, best seen on lateral view. An exaggerated double break will lead to the appearance of a short nose. The absence of a double break will add length to the nose. Therefore the double break and its degree will affect the appearance of the length of the nose.
5. Controlling the 4 critical areas of the nasal tip
Medial Crurae/Columella
The medial crurae make up the majority of the columella, with the exception of the infratip. Medial crurae can be smooth or undulate, creating surface contour problems or frank deviation of the columella. The caudal septum being off midline can also secondarily cause columellar deviation and/ or medial crural contour asymmetries. A caudal septum that lies midline behind the membranous septum is critical for columellar symmetry.
Medial crural buckling can be controlled easily with suture fixation to a straight columellar strut or a straight caudal septum (in a tongue in groove) or septal extension graft. Sewing the medial crurae to a columellar strut, even one that is 1-2mm wide will not negatively affect columellar aesthetics, provided that excess soft tissue from the intercrural space has been resected.
Infratip lobule
In the senior author’s opinion, the infratip lobule is the key to defining favorable nasal tip aesthetics. The infratip lobule is the curvilinear portion of the lower lateral cartilages, made up by the intermediate crurae. As the cartilages bend out towards the caudal aspect of the domes, the infratip lobule is formed.
An infratip lobule that is too long or too curved can result in poor nasal tip aesthetics, with volume excess on frontal view. The patient will often perceive their nasal tip as droopy, when the profile view shows normal rotation in the columella. In patients with actual nasal tip ptosis, it serves to intensify the perception of ‘droopiness.’
A full infratip lobule is also associated with deep and large facets, as well as a false perception of over-rotation in some patients, due to excess medial nostril patency. A short and relatively flat infratip lobule is generally desired. The shape can be controlled by the placement of sutures between a columellar strut and the intermediate crurae. The most anterior suture will define the beginning of the infratip and the double break of profile. The infratip can be further flattened with intermediate crural division. The senior author will typically curve the upper most aspect of the columellar strut in order to control the shape and degree of curvature of the infratip lobule.
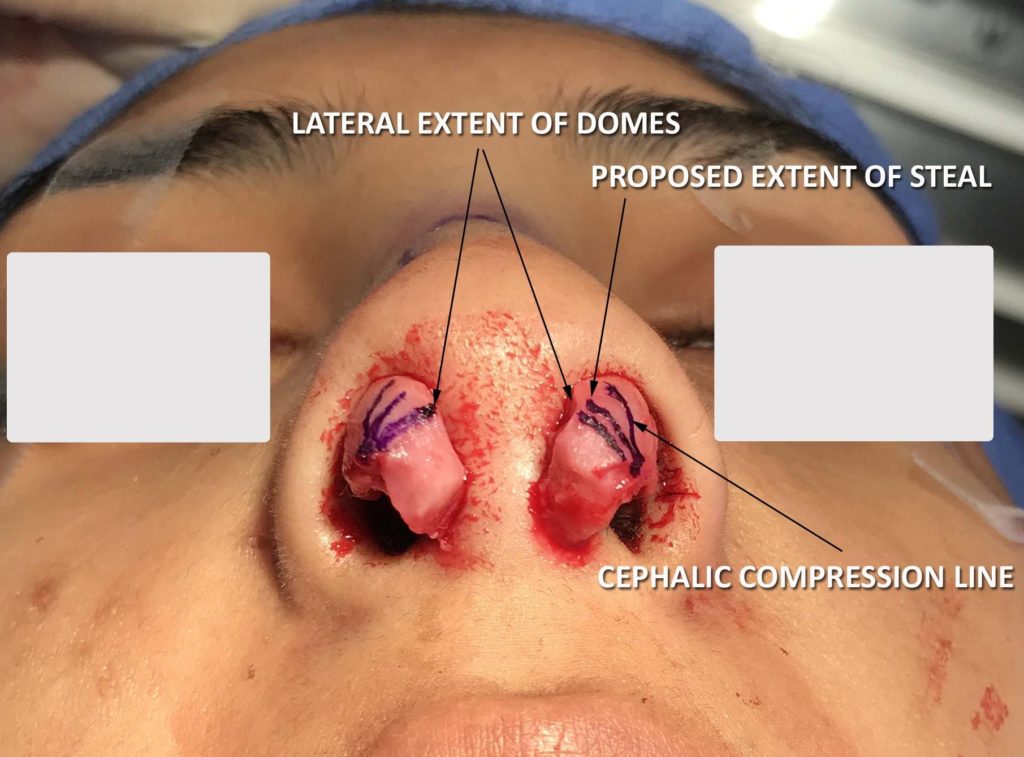
Domes
The domes of the lower lateral cartilages are, themselves, triangularly shaped. The cephalic aspect of the dome should be more tighter and the caudal aspect of the dome should be a looser turn. This creates a triangular appearance to the dome. The expansion of the caudal aspect of the dome helps to set the lateral crural resting angle medially, which will propagate along the lateral crus, provided the cartilages have sufficient tensile strength.
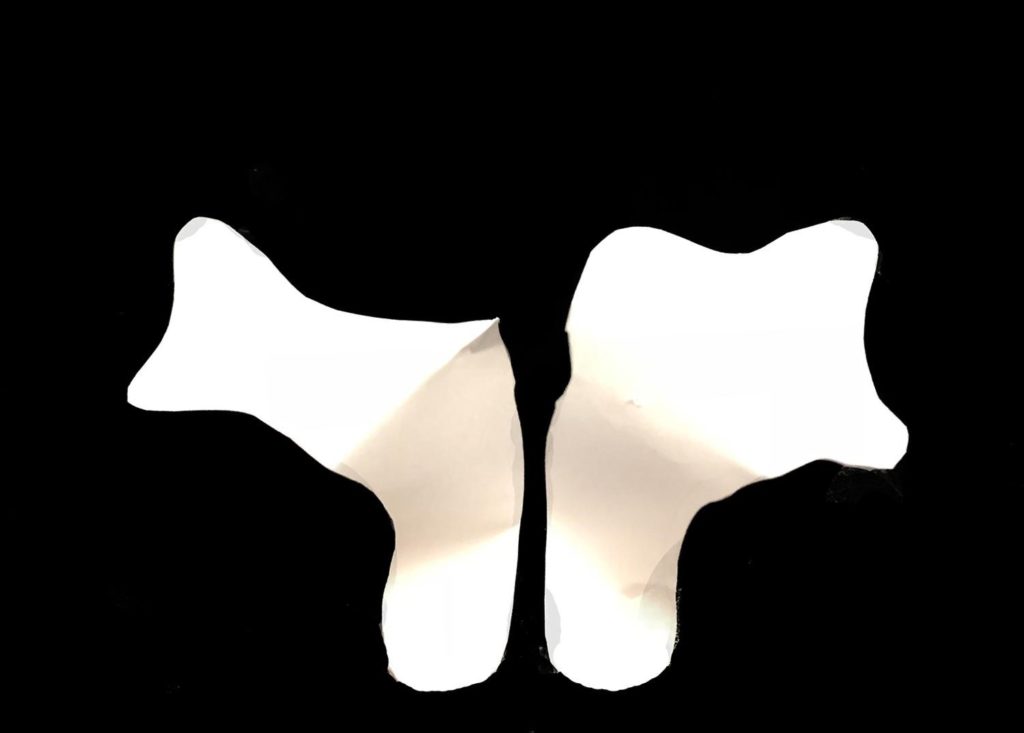
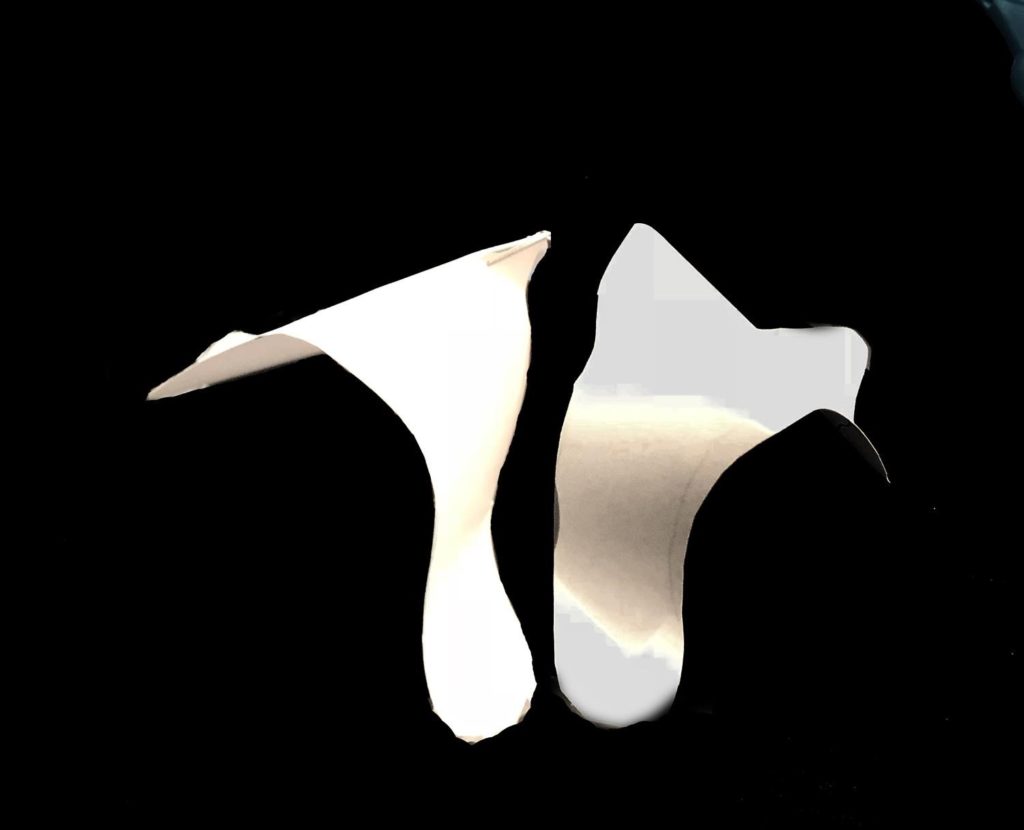
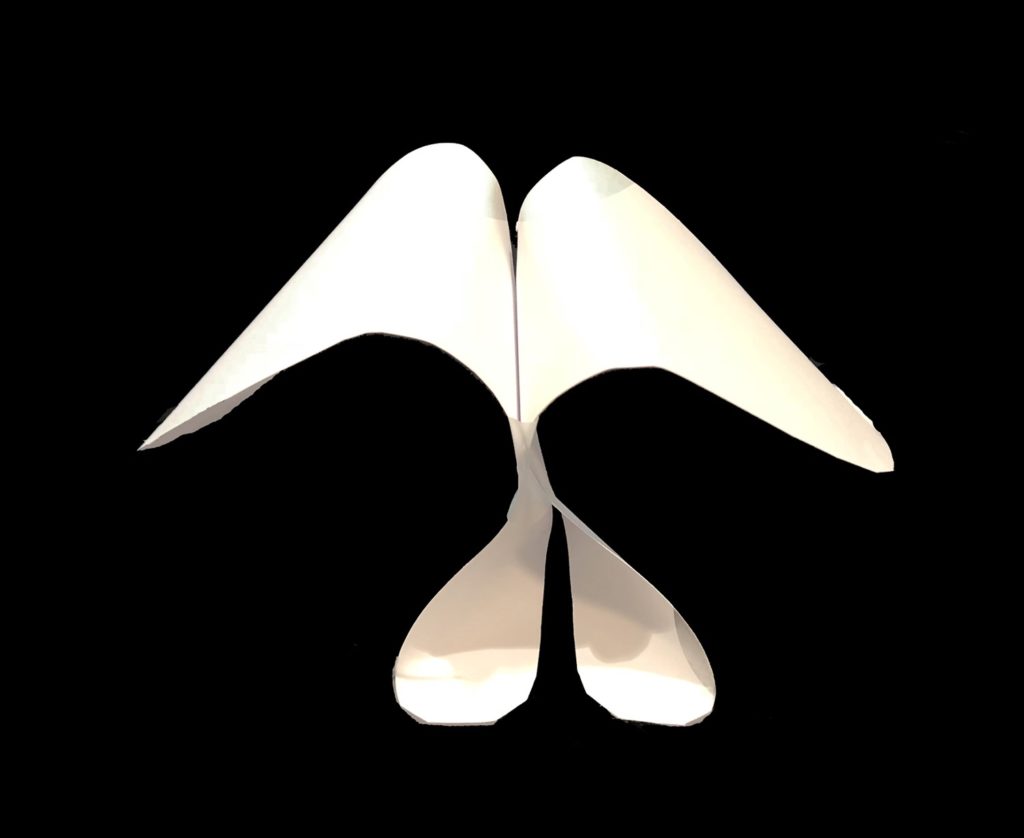
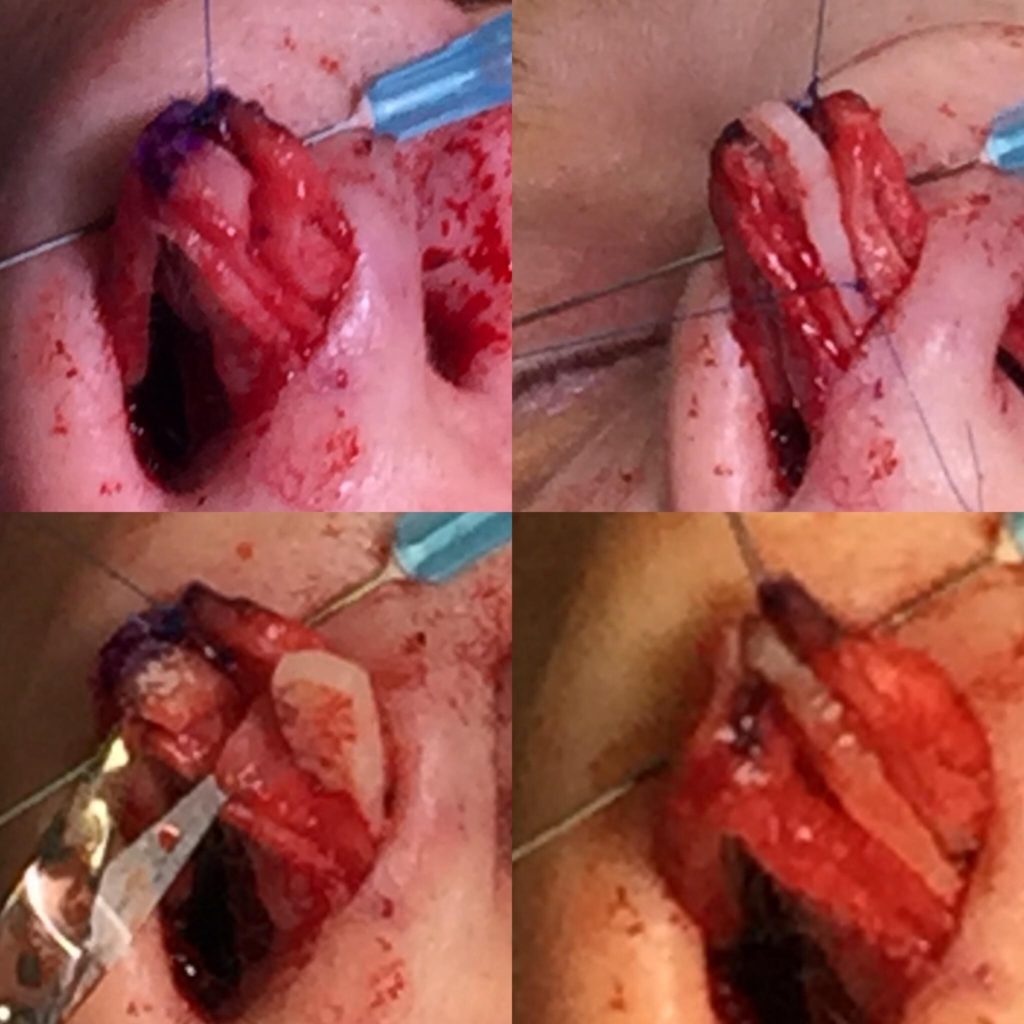
Figure: Compression of the cephalic portion of the dome seen from superior (left) and basal views (right) creates a significant improvement in lateral crural resting angle and a retrodisplacement of the cephalic upper lateral cartilage.Closure of the infratip lobule and loss of the Angle of Dome Divergence causes the opposite effect.
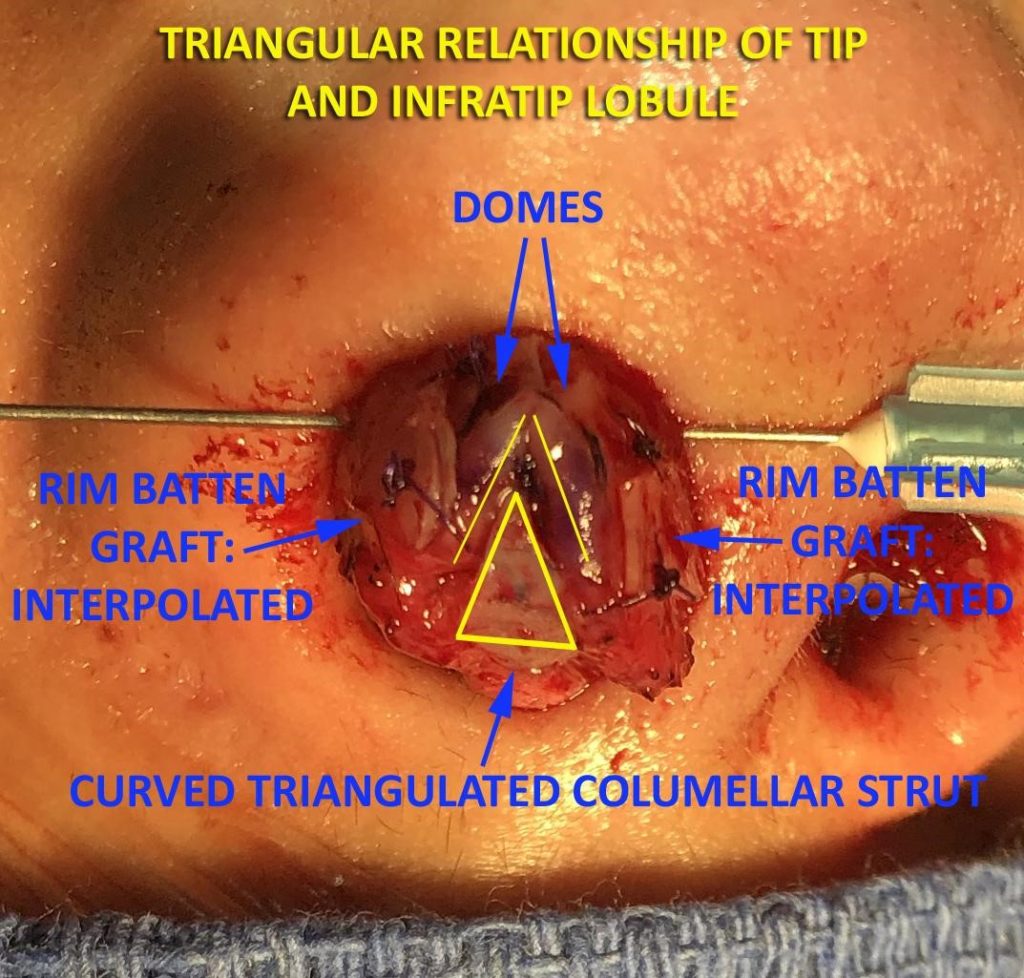
The domes should also not be tightly opposed in the caudal aspect of the dome unit. Columellar struts can be used to prevent over-narrowing of the caudal dome segment. Only the cephalic aspects of the domes should be touching. Caudally, a diastasis should be present. Closure of the inferior aspect of the dome will draw the caudal border inferiorly and medially, resulting in a poor lateral crural resting angle. The senior author typically will use cartilage that can be carved into a triangle on the most projecting portion of the columellar strut. This can be used to control the shape of the tip complex, preserving a diamond or triangular relationship between the domes.
Lateral crus:
Based on a lateral crural resting angle of 120 degrees, the cephalic margin of the lateral crus should lie posteriorly displaced in relation to the caudal margin. This may happen naturally after dome sutures have been placed. If not, it needs to be created.
Understanding that the caudal aspect may require projection to offset cephalic fullness, alar rim overlay grafts are extremely useful in this regard. While vestibular underlay grafts may flatten the lateral crus, they may not create the projection differential that is desired. Batten grafts will fight against this differential as well and should only be used if a lateral crus is overly concave and there is a loss of symmetry. Cephalic trim can be useful in order to create a reduction in the supratip contour. If an open approach is used a ‘lateral crural canting suture’ described by Dr. Minas Constantinides, can be used. This suture spans from the caudal aspect of the upper lateral cartilage to the caudal aspect of the lower lateral cartilage. Differential tension on this suture will cause the caudal border to elevate.
6. Grafts – When to use and how to decide
Columellar strut
The columella not only serves an important role in aesthetic balance of the nasal tip but also provides structural support for the lower lateral cartilage. It allows for repair of buckling or malposition, or to address asymmetry of the medial crura if required. A common indication is short, weak, or flared medial and intermediate crura. As a maneuver to project the tip, if more than 1-2 mm of projection is required, a strut graft can be useful. Therefore, the degree of nasal tip projection and structural integrity of the lower lateral cartilages dictates whether or not a columellar strut is necessary and what should be used.
The graft is placed between the medial crura but short of the domes to prevent a ‘unidome’ appearance. Additionally, to avoid displacement of the graft during lip movement, a small amount of soft tissue can be left on the nasal spine. Alternatively, it can also be secured via suturing to the spine or premaxilla, but this can cause pain or rigidity in some patients.
Lateral crural support/strut grafts
Lateral Crural Strut grafts are strips of cartilage that are sutured to the deep surface of the lateral crura, between the lateral crural cartilage and the vestibular mucosa. Lateral crural strut grafts allow for the correction of deformities of the lateral crura. They can aid in the flattening of these structures to allow for a more pleasing tip. They can be used to increase structural support in cases of previous over-resection or need for additional crural integrity. This also helps to prevent alar rim retraction, which can lead to an abnormal appearance of the nostrils, excessive columellar show and an undesired cosmetic outcome25. Other indications include repair of a boxy tip, malpositioned lateral crura, lateral recurvature, or misshapen lateral crura.
In cases where a longer strut is required for severe collapse of the ala or for retraction, the lateral crus can be separated from the accessory cartilages allowing the graft to be situated along the piriform aperture rim. This further allows the lower lateral crura to conform to the shape of the graft and the entire composite is then re-implanted.
Batten grafts
Batten grafts can provide additional support to the lateral crura and external valve, particularly in the case of collapse. The graft can be placed on the surface of the native cartilage, in true batten form, or as an alar strut graft between the mucosa and native lower lateral cartilage. Exact placement should be determined by the point of maximal collapse26.
Tip grafts
There are a variety of different tip grafts, which can achieve increased tip projection or be used to address subtle contour irregularities of the nasal tip. Onlay grafts are placed over the domes. It is often helpful to soften the edges of the graft with a beveling or morselization technique. Examples of onlay grafts include the peck or cap graft. Cap grafts in particular are good for patients with thin skin to address any areas of the tip with clefting or to soften contours when placed between the tip defining points and the medial crura. When placed in this location, they add projection and volume to the infratip lobule. When placed over the tip defining points, the tip is projected and further defined26. They should preferentially not be placed over the cephalic aspect of the unified dome structure, but, rather, slightly shifted to the caudal aspect for best aesthetics.
Infratip lobular shield grafts also help to project and define the tip while providing contour to the infratip region. They are seated over the caudal aspect, even as far as the medial crura, from the foot plates to the nasal tip. These should not be used in thin skin patients, as post operative visibility is a common problem. Other options include the anchor graft, subdomal graft, or multilayered grafts.
Pre-crural grafts
Precural grafts are not often used unless, despite the previous grafting methods, the columella still appears retracted. Occasionally, after an infratip graft to conceal intermediate crural division edges, the lower columella requires additional fullness. Also, precrural grafts are sometimes necessary with caudal septal extension grafting techniques.
7. Special considerations for deviated or asymmetric tips
Lateral length importance, Dealing with length asymmetries – shoehorn effect, Asymmetrical grafting requirements, Facial Asymmetry
Potential length asymmetries of the lower lateral cartilages are critical factors to identify preoperatively and address intra-operatively. Deviated noses, and even some midline noses will have asymmetries that can have an impact on the final result, even if they appear to be corrected intraoperatively. When extra length is forced into the columellar segment by differential crural steals, the patient is at a high risk for post operative columellar deviation. The converse is true for the lateral crus. Extra length will often present as a convexity or new deviation over time. This is called the “shoehorn effect” by the senior author.
Contour asymmetries of the infratip lobule are very common in patients with length discrepancies. A loss of the light reflux will be seen on base view, which usually results from the caudal edge of the medial and intermediate crus. A lowering of the dome height may or may not be seen in association with this finding. A high level of suspicion must exist preoperatively, as these can sometimes disappear after cartilage dissection. Intermediate crural division or direct suture fixation to a columellar strut are important for long term correction. As the buckled intermediate crura adds no projection to the nasal tip, division is often the preferred method.
Prior to intermediate crural division for any purpose, the surgeon must set the lateral crural length on both sides with the placement of the dome suture. After division, it becomes much harder to determine lateral length symmetry, as the lateral crura are free to spin and move in all planes. Therefore, dome binding and unification with midline verification is always done before intermediate crural divisions, regardless of whether an open or closed approach is being used. The senior author prefers to perform lobular division techniques in the intermediate crus, rather than the lateral crus, due to the ease of stabilization using the columellar strut.
When facial asymmetry is present, these techniques are even more important. When looking at the base view, a recession of one nostril is often seen.31 This will make the likelihood of length asymmetries very high. A subalar graft is often placed on the deficient side and, as a result of lateral crural steal on the opposite side to medialize the tip, a contour graft is typically needed on the contralateral crura. Unilateral intermediate crural division is commonly done in these patients.
8. The endgame goal for under the skin appearance
The endgame for any surgeon represents the confluence of their experience correlating cartilage appearance to ultimate result. Knowing those correlations and what the cartilage should look like allows for complex cases to be simplified. For the senior author, the following factors in the nasal tip are necessary for case completion.
- Triangular dome shape and dome apposition
- Loose separation of the intermediate crurae
- Slight curvature of the infratip lobule
- Caudal lateral crural projection in relation to cephalic lateral crurae (causing a continuous light reflex along the alar margin)
- Lateral crural length equalization
- Alar grafting for facial asymmetry and correction of base view
When these relative components combine as a whole, a Rhinoplasty surgeon can be confident in the aesthetic outcome of simple or complex cases.
References:
1. Nahai F. Your Favorite Technique: Time for a Change? Aesthetic Surgery Journal. 2012; 32(7) 135-136
2. Nahai F. Evidence-Based Medicine in Aesthetic Surgery. Aesthetic Surgery Journal. 2011;31(1):135-136
3. Daniel RK. The nasal tip: anatomy and aesthetics. Plas Reconstr Surg 1992;89:216-24
4. Ketcham A, Dobratz E. Normal and Variant Anatomy of the Nasal Tip. Facial Plastic Surgery. 2012;28(02):137-144
5. Byrd HS, Hobar PC. Rhinoplasty: a practical guide for surgical planning. Plast Reconstr Surg. 1993;91(4):642-656
6. Crumley RL, Lanser M. Quantitative Analysis of Nasal Tip Projection. The Laryngoscope. 1988;98(2):202-208
7. Devcic Z, Rayikanti BA, Hevia JP, Popenko NA, Karimi K, Wong BJF. Nasal tip projection and facial attractiveness. The Laryngoscope. 2011;121(7):1388-1394
8. Zelnik J, Gingrass RP. Anatomy of the alar cartilage. Plast Reconstr Surg. 1979;64(5):650-653
9. Sheen J., Sheen A.P. Aesthetic Rhinoplasty. Ed.2. St. Louis: The C.V. Mosby Co.; 198
10. Baker SR. Suture contouring of the nasal tip. Arch Facial Plast Surg. 2000;2(1):34-42
11. Wang Z, Wang N, Yang H, Bai S. [Investigation of the layers and vascular density of the soft tissue in the inferior nasal portion]. Zhonghua Zheng Xing Wai Ke Za Zhi. 2007;23(1):65-68
12. Çakır B, Öreroğlu AR, Doğan T, Akan M. A Complete Subperichondrial Dissection Technique for Rhinoplasty With Management of the Nasal Ligaments. Aesthetic Surgery Journal. 2012;32(5):564-574.
13. Rohrich RJ, Pulikkottil BJ, Stark RY, Amirlak B, Pezeshk RA. The Importance of the Upper Lateral Cartilage in Rhinoplasty: Plastic and Reconstructive Surgery. 2016;137(2):476-483
14. Sepehr A, Alexander AJ, Chauhan N, Chan H, Adamson PA. Cephalic Positioning of the Lateral Crura: Implications for Nasal Tip-plasty. Archives of Facial Plastic Surgery. 2010;12(6).
15. Çakır B, Öreroğlu AR, Daniel RK. Surface Aesthetics in Tip Rhinoplasty: A Step-by-Step Guide. Aesthetic Surgery Journal. 2014;34(6):941-955
16. Constantian MB. Elaboration of an Alternative, Segmental, Cartilage-Sparing Tip Graft Technique: Experience in 405 Cases: Plastic and Reconstructive Surgery. 1999;103(1):237-253.
17. Adamson PA, McGraw-Wall BL, Morrow TA, Constantinides MS. Vertical Dome Division in Open Rhinoplasty: An Update on Indications, Techniques, and Results. Archives of Otolaryngology – Head and Neck Surgery. 1994;120(4):373-380
18. Gunter JP, Friedman RM. Lateral Crural Strut Graft: Technique and Clinical Applications in Rhinoplasty: Plastic and Reconstructive Surgery. 1997;99(4):943-952.
19. Constantian MB. The incompetent external nasal valve: pathophysiology and treatment in primary and secondary rhinoplasty. Plast Reconstr Surg. 1994;93(5):919-933
20. Constantian MB. The Boxy Nasal Tip, the Ball Tip, and Alar Cartilage Malposition: Variations on a Theme- A Study in 200 Consecutive Primary and Secondary Rhinoplasty Patients: Plastic and Reconstructive Surgery. 2005;116(1):268-281
21. Losquadro W, Bared A, Toriumi D. Correction of the Retracted Alar Base. Facial Plastic Surgery. 2012;28(02):218-224.
22. Bruintjes TD, Van Olphen AF, Hillen B, Huizing EH. A functional anatomic study of the relationship of the nasal cartilages and muscles to the nasal valve area. The Laryngoscope. 1998;108(7):1025-1032.
23. Totonchi A, Guyuron B. Alar Rim Deformities. Clinics in Plastic Surgery. 2016;43(1):127-134.
24. Bloom JD, Ransom ER, Miller CJ. Reconstruction of Alar Defects. Facial Plastic Surgery Clinics of North America. 2011;19(1):63-83
25. Rhinoplasty Dissection Manual. Rhinoplasty Analysis. Retrieved from https://www.therhinoplastycenter.com/rhinoplasty-dissection-manual
26. Hilger Facial Plastics Clinic. Grafting in Rhinoplasty. Retrieved from https://www.hilgerfacialplastic.com/media/publications/rhinoplasty-grafting
27. Cakir B., Oreroglu A., Daniel R. Surface Aesthetics and Analysis. Clin Plastic Surg 43(201) 1-15.
28. Touriumi DM. New Concepts in nasal tip contouring. Arch Facial Plast Surg 2006; 8(3) 156-85
29. Westreich R, and Lawson W. The Tripod Theory of Nasal Support Revisited: The Cantilevered Spring Model. Arch Facial Plast Surg. 2008;10(3):170-179.
30. Westreich R.MD, Courtland H., Nasser P., Jepsen, K. Ph.D., and Lawson W. M.D.-D.D.S. Defining Nasal Cartilage Elasticity: Biomechanical Testing of the Tripod Theory based on a Cantilevered Model. Arch of Facial Plastic Surgery. 2007; 9(4): 264-270.
31. Burstin D., Frasier M., and Westreich R.. The Effect of Facial Asymmetry on Nasal Deviation. Chapter, Facial Plastic Surgery Journal. 2012.
