Abstract
Nasal projection is a vitally important consideration during pre-operative planning, during rhinoplasty surgery itself and post-operatively it is a major determinant of the final result. A technique to create visual aids for analyzing a nose, particularly with regard to planning the ideal tip tip position, using a modified Guyoron approach is described The rhinoplasty surgeon must understandthe concepts of nasal projection and how surgical incisions and approaches may result in unplanned changes in this parameter. The techniques for increasing or decreasing tip projection to produce a tip position that matches an ideal dorsal height and line are described, The relationship between tip projection and rotation and the nasal dorsum are explored.
Introduction
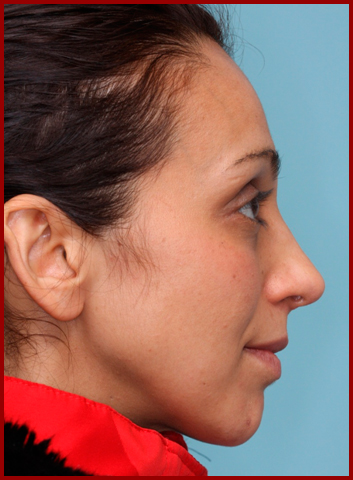
Modern rhinoplasty aims to achieve a non-surgical appearance for the nose with a size that is in harmony with the face. The surgeon’s goal with pre-operative analysis should be to determine the ideal position for the nasal tip after having understood and defined the ideal position for the nasion. The aim of surgery should then be to achieve these ideal landmark positions and then set the dorsal line between them. Modern rhinoplasty techniques have increased the surgeon’s ability to control tip projection. This facilitates a more balanced approach to rhinoplasty rather than a purely reductionist approach whereby the tip is routinely reduced and then the dorsum lowered to match the tip1-3. This can result in excess nasal reduction and a flat nose, particularly if the tip was underprojected. Alternatively if tip overprojection is not recognized and the dorsum is reduced, an un-natural “ski-slope” appearance may result. The patient seeking a smaller nose may be disappointed to hear the surgeon wants to bring the nose into balance with the rest of the face by increasing projection. It is thus an area that warrants special attention and careful discussion with the patient. During surgery projection should always be paramount in the surgeon’s mind for optimal results. This is only possible if the surgeon has a firm grasp of the concepts of nasal projection, including the skills necessary to ascertain the ideal nasal parameters for a particular face4,5 and the surgical techniques for changing tip projection.
Anatomy
The most relevant anatomy to support an understanding of nasal projection includes:
The major tip support mechanisms according to Dr. Tardy5,6:
- The size, shape and resilience of the lower lateral cartilages.
- The medial crural footplate attachment to the caudal border of the quadrangular cartilage.
- The attachment of the upper lateral cartilages (caudal border) to the alar cartilages (cephalic border).”
The minor tip support mechanisms
- The Interdomal “ligament”.
- The cartilaginous septal dorsum.
- Sesamoid complex extending the support of the lateral crura to the pyriform aperture.
- Attachment of the alar cartilages to the overlying skin and musculature.
- Nasal spine.
- Membranous septum.
These structures have traditionally been incorporated into the Tripod theory to understand and predict tip projection7 and rotation changes after alteration of the structures that form the tripod legs. Although useful as a teaching tool, the nasal tripod is not resting on the bony pyramid as the theory would suggest, but rather is suspended over the anterior septal angle and is attached to the fixed septal cartilaginous framework of quadrilateral cartilage and upper lateral cartilages by ligamentous tensile support and additional tethering to to the nasal bony base. This allows the tip to recoil to its normal position if the tip is pushed in with a finger6. The concept of nasal tip tensegrity (tensile-integrity) allows for a better understanding of the dynamic spring-loaded nature of the nose. In architectural and engineering terms, tensegrity is the study of the compressive (acting to compress, or in this case collapse the tip) and tensile (acting to lengthen, or hold the tip up) forces that are acting on a structure. It is the balance of the tensile and compressive forces that gives form and stability to any structure, including the nasal tip. It is helpful to understand the nasal projection as a function of nasal tensegrity in order to restore resilience, support and function intraoperatively.6 Tip projectionand techniques to change it cannot be considered in isolation from from tip rotation8,9. Both have to be considered at the same time as techniques to alter one may alter the other whether changing the length of the medial or lateral crura of the tip cartilages themselves or changing the length or projection of the cartilaginous septum .The consistency of the relation has led to the development of useful algorhithms for surgical deprojection of the tip9. Therefore when assessing the position of the nasal tip and how to change projection and rotation the surgeon must consider intrinsic lower lateral cartilage anatomy such as the length of the medial and lateral crura and extrinsic anatomical factors, particularly the size and shape of the cartilaginous septum and upper later cartilages.
Analysis
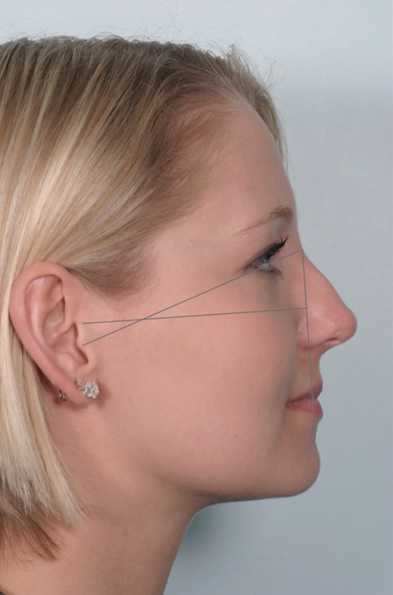
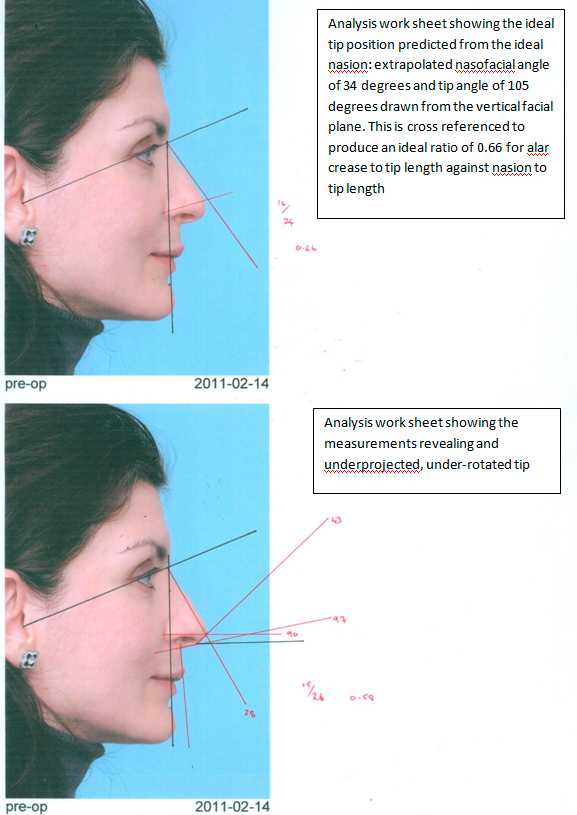
The authors prefer a modification of the approach described by Guyuron in 1987 10,11. Guyuron described “a simple technique to draw an aesthetically pleasing and very proportionate profile outline of the nose”10 based on detailed soft-tissue cephalometric analysis of 1619 life-sized photographs and makes for some worthwhile reading.
The authors have modified this to allow a more practical application in modern aesthetic practice.
After the initial consultation, large half page layouts of the standard rhinoplasty photos and manipulated images are printed onto high quality paper. The patients are photographed holding a ruler which can be calibrated to allow measurement of distance between anatomical landmarks.
The ideal nasion position is defined as 10-13mm anterior to the anterior corneal plane and between the supratarsal crease and lash line in forward gaze. If the nasion is within this parameter, it is used, otherwise an ideal radix point is marked (point N).
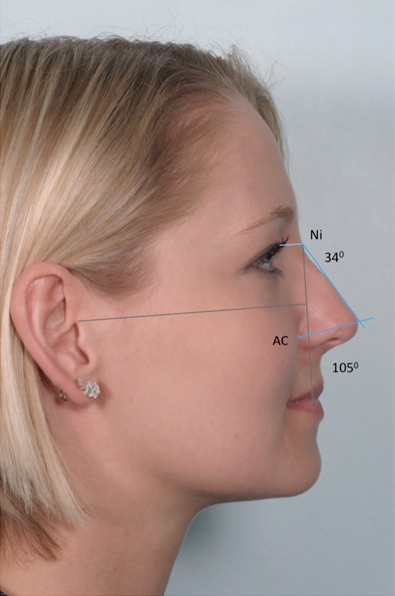
The midpoint of the tragus is used to connect to the marked nasion position (point N). A vertical line dropped inferiorly from the ideal nasion point at 69 degrees (67 – 73 degrees range)is drawn and marks the vertical facial plane (VFP).
The Nasofacial angle is drawn next from N to the nasal tip and is measured in relation to the VFP. In male noses, this should be 36 degrees and in female noses this should be 34. If not, the ideal dorsal profile is drawn using the stated angles.
The tip angle is outlined next, drawn from the midpoint of alar crease to the tip. This angle should measure 100 degrees from the VFP in males and 105 degrees in females.
The ideal tip position is found where the ideal nasofacial angle line and the ideal tip angle line intersect.
Tip projection can be cross-checked. The distance from the alar crease to the tip should be approximately 66% of the distance from the nasion to the tip.
Tip projection may be separated into equal thirds for further analysis12. The components are from the alar crease to the subnasale, from the subnasale to the columella breakpoint and from the columella breakpoint to the tip. Analysis must determine whether disorders of tip projection are due to extrinsic anatomical structures such as the anterior nasal spine and septum or intrinsic tip structures namely the length of each of the three crura of the lower lateral cartilages.
Planning surgery
When planning an intervention, it is helpful to think in terms of the Tensegrity model6,13 as described aboveThis concept, originally developed for the architectural industry, divides forces into either compressive, that which intends to shorten, and tensile forces, which intends to lengthen. Objects under compressive force often needs to be bulky and heavy and inherently strong, such as slabs of concrete, while those in tension are often lighter, such as cables. Put together they form an aesthetic and functional balance such as in the case of a suspension bridge. It is important to understand the stability is due to the way the entire structure distributes and balances mechanical stresses14. That is, the components are already under stress before any load is carried. This is called pre-stress. The rigid struts are tensing the cables and the cables are compressing the struts. These forces equilibrate throughout the structure and enable it to be stable.
Similarly, the nasal tip needs to provide a stable and patent internal nasal valve, take the significant load of the soft tissue envelope and resist postoperative scar contracture. To accomplish this the nasal tip needs to have strong cartilaginous structural support from the medial and lateral crurae, the nasal septum, the upper lateral cartilages and the nasal spine that can bear the compressive load. These are held together by tensile components, the most important of which are the intercrural ligament and the attachments between the medial crura and the cartilaginous septum 6,14.. Where the surgeon alters the nasal tensegrity, both structural and tensile reconstruction is needed, and in the right balance. This is achieved by using a layered closure approach, preserving or reconstructing and re-enforcing structural components and holding the tip pre-stressed under tension in the desired position while the midline intercrural ligament is reconstructed6. This chapter is focused on nasal projection and deprojection, but attention should also be paid to creating the ideal radix with regard to both its supero-inferior position and its projection prior to addressing the tip position9.
Dissection
Tip projection is best considered and established utilizing a graduated and step wise approach to the lower lateral cartilages and their supporting structures16-22. This approach offers the best trade-off between optimal results and increasing risk of secondary changes and complications. At the conclusion of surgery the tip should project at least 5mm anterior to the anterior septal angle, especially in thick skin20 in order to achieve a pleasing tip/supratip relationship.
Incisions and approaches
Incisions should be planned with projection in mind. Where the plan is to retroproject the tip, the transcolumella incision should be placed slightly anterior from the standard (and if the tip projection is to be increased, the incision should be placed slightly lower on the columella) as the scar will be less prominent8.
Fa ull transfixion and intercartilagenous incisions can be used to contribute to retroprojection if necessary.6. The authors prefer the open approach15but a full transfixion incision can still be used to access the septum and to facilitate retroprojection when required. The amount of lateral dissection depends on the goal of surgery, but should allow adequate exposure and access. The scroll area once dissected, allows for greater freedom of movement of the lower lateral cartilages. When lower lateral strut grafts are planned, the vestibular skin will also need to be dissected from the lower lateral cartilages. During the dissection the surgeon needs to mentally plan ahead as reconstruction of the divided tensile components of the nose will be necessary later. In open approach surgery separation of the medial crurae of the lower lateral cartilages (tip split), particularly if combined with elevation of bilateral septal flaps, will release many tensile elements such as the interdomal ligament and the attachments of the medial crural footplates to the septum producing retroprojection.
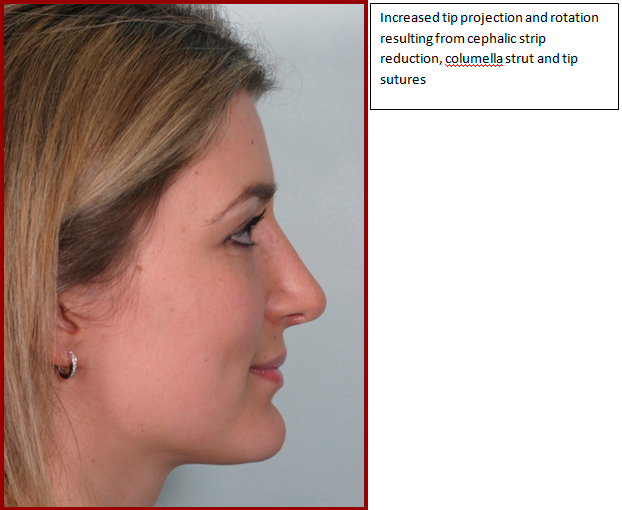
Resection of the cephalic strip
Resection of a cephalic strip of lateral crura will release the lower lateral from the upper lateral crura and may result in retroprojection. The authors advise preserving at least a 6mm strip of lower lateral cartilage for structural integrity. The technique must be used with great caution when the lateral crura are malpositioned, running in a more cephalic orientation, as in the parenthesis tip, where the lateral crurae make an acute angle (less than 30 degrees) with the nasal septum. Alar rim retraction and alar margin weakness will be exacerbated. The lateral crurae should be repositioned preferably with lateral crural strut grafts. Tip projection manouevres in these cases are highly complex.
Dorsal reduction
The authors have previously published a case series of female Northern European rhinoplasty patients23. “In our series 81% of patients had a hump and 54% had an overprojected tip. If overprojection is not recognised and a hump aggressively lowered, the nose will look excessively concave and unnatural with a “ski-jump” appearance in the lateral view and a washed out, flattened appearance in the middle third on frontal view. This will particularly be of concern in the thin skinned patient who made up a quarter of our patients. Skin will shrink wrap more in these patients and as in all patients such shrinkage will occur more over the bony dorsum than the suratip area.”23
Anterior nasal spine reduction
Overdevelopment of the anterior nasal spine and / or the posterior septal angle will increase the columella labial angle and create the illusion of an over-rotated tip. Finding the ideal position of the subnasale will help to determine whether these two anatomical structures are overdeveloped or whether the nose is short. This helps the surgeon decide whether reduction of the anterior nasal spine and posterior septal angle is appropriate. Such a reduction would be incorrect if the tip is intrinsically over rotated due to excessively long medial crura or extrinsically over rotated due to a short nasal septum23.
Tip sutures
The authors have found the tip sutures as described by Rollin K. Daniel12,20 and John Tebbetts24 to be very useful in fine-tuning the tip position as well as shape. Tip sutures are reversible and can be thrown and their effect assessed prior to knotting. They can also be removed and repositioned later in the surgery if subsequent maneuvers alter their effects
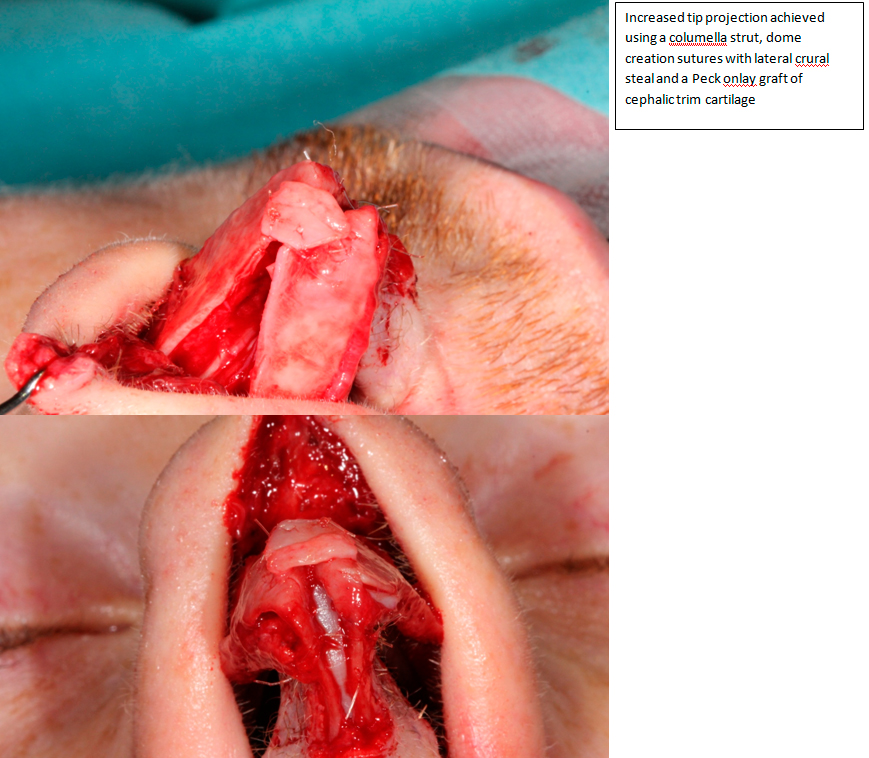
Dome creation sutures12 can lead to an increase in projection by essentially a lateral crural steal. As part of a layered closure and to improve tensegrity, suturing the medial crurae to the columella strut graft allows for pre-stressing the tip and stabilizes tip projection. Suturing the medial crurae to the septum or septal extension graft allows for adjustment of projection in the “tongue and groove” technique17.
Interrupted strip techniques
Division of the medial or lateral crurae (or indeed both) with overlapping and suturing is able to powerfully retroproject the tip, but the tripod model should be borne in mind as rotation will be a significant secondary change9.
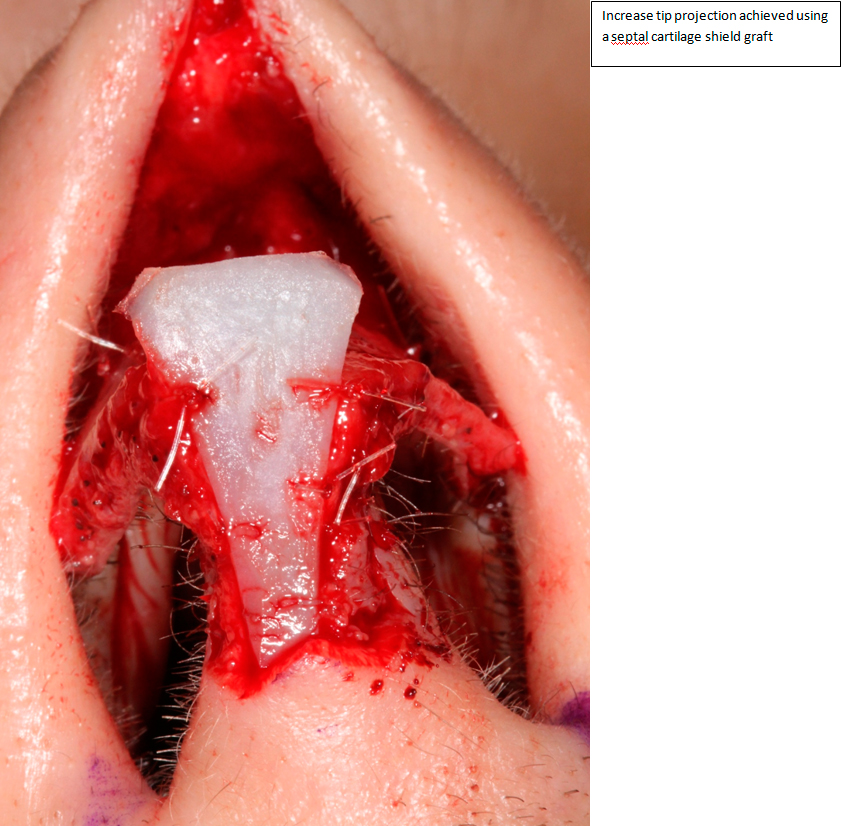
Dome division
This technique is utilized if the domes are asymmetrical and the above techniques fail to improve on this or if excess cartilage is present in the arch of the lower lateral cartilage. The domes are resected, and the tip area covered by a shield graft as described by Calvin Johnson 25.
Structural grafts
Compressive structures may be augmented with grafts such as columella struts, shield grafts and Lateral crural strut grafts to augment projection and prevent retroprojection.
The under projected tip
The limiting factor in tip projection is the soft tissue envelope, which poses an ever increasing load the higher the tip is projected. This is especially so if the nose has been subjected to previous trauma or surgery with contraction of the soft tissue envelope. The tensegrity model provides for a combination of strong compressive and tensile forces to be able to withstand the load of the soft tissue envelope.
Septum
The septum provides the foundation on which tip surgery is performed. The caudal end of the septum may be strong enough or may need reinforcement with a columella strut or a caudal extension graft. The dorsal aspect of the septum is best supported with extended spreader grafts. Combinations of the grafts mentioned will help reinforce the L-strut. The tip can be attached to and positioned on this stable foundation.
Sutures
Dome creation sutures12 can increase projection by essentially a lateral crural steal. Suturing the medial crurae to the columella strut graft allows for improved tensegrity and tip projection. Suturing the medial crurae to the septum or septal extension graft allows for even greater control and projection in the “tongue and groove” technique17.
Tip grafts
Shield grafts have been proposed to be of benefit to increase projection, but this should be limited to patients with a thick skin envelope as over time the graft tends to become visible. A blocking/buttress graft will ensure the shield graft does not bend posteriorly when the skin is replaced over the tip and hence improves projection 26. Lateral crural onlay grafting to further camouflage the edges has been described19. Tip onlay (Peck) grafts will augment projection and aid tip definition26.
Lateral crural strut grafts27
The lateral crural strut grafts have been gaining widespread application in cases of external valve collapse and improving the tensegrity of the lateral crus. They are a powerful adjunct to prevent long term alar retraction and are able to aid repositioning of the lower lateral crurae. They are capable of an increase in projection as per the tripod theory. By extending the grafts medially they also help in tip definition. They add structure and make tensegral sense. The authors are increasingly using lateral crural strut grafting. Due to the extensive dissection involved compressive splints are advocated by some surgeons8.
Rim grafts28
Rim grafts are less powerful and more delicate than lateral crural strut grafts, but play an important role in preventing notching of the alar rim. They add structure without adding bulk due to their extra-anatomical positioning. The authors advise a low threshold for using them, but they are not powerful enough on their own to correct a notched alar rim.
Conclusion
Nasal projection is an important aspect of the assessment of any patient requesting a rhinoplasty. Special attention should be paid to the pre-operative photographs and actual measurement made as described as part of the analysis. Intra-operatively techniques to both increase and decrease projection should be applied in a graduated step wise approach. The surgeon needs to constantly re-evaluate as secondary changes may occur after every step. Rotation and projection in particular are closely linked.
References
- Romo T, Soliemanzadeh P, Choe KS, Sclafani AP. Reduction Structured Rhinoplasty. Facial Plast Surg 2003;19:317-324
- Daniel RK, Lessard ML. Rhinoplasty: A graded aesthetic-anatomical approach. Annals of Plastic Surgery 1984;13:436-451
- Daniel RK. The nasal tip. In: Daniel RK. Rhinoplasty: Aesthetic Plastic Surgery. Boston: Little, Brown And Co; 1993:227-234
- Davis RE. Rhinoplasty and concepts of facial beauty. Facial Plast Surg 2006;22:198-203
- Tardy ME. Surgical anatomy of the nose. New York:Raven Press;1990
- Dyer WK. Nasal tip support and its surgical modification. Facial Plast Surg Clin N Am 2004;12:1-13
- Goode RL. A method of tip projection measurement. In: Powell N, Humphrey B, eds. Proportions of the Aesthetic Face. New York: Thieme-Stratton; 1984:15-39
- Toriumi DM. Personal communication.
- Soliemanzadeh P, Kridel RWH. Nasal tip overprojection: Algorithm of surgical deprojection techniques and introduction of medial crural overlay. Arch Facial Plast Surg 2005;7:374-380
- Guyuron B. Precision Rhinoplasty. Part I: The role of life-sized photographs and soft-tissue cephalometric analysis. Plast Reconstr Surg 1988;81:489-499
- Guyuron B. Precision rhinoplasty. Part II. Plast Reconstr Surg 1988;81:500-505
- Daniel RK. Mastering Rhinoplasty. A comprehensive atlas of surgical techniques with integrated video clips. New York:Springer;2010:101-154
- Pugh A. An Introduction to Tensegrity. Los Angeles:University of California Press;1976
- Ingber DE. The architecture of life. Scientific American 1998;1:48
- Adamson PA, Litner JA. Open Rhinoplasty. In: Papel ID, ed. Facial Plastic and Reconstructive Surgery.3rd ed. New York: Thieme; 2009:529-546
- Guyuron B. Predictive rhinoplasty. In: Daniel RK. Rhinoplasty: Aesthetic Plastic Surgery. Boston: Little, Brown And Co; 1993:109-111
- Lo S, Rowe-Jones J. Suture techniques in nasal tip sculpture: current concepts. The Journal of Laryngology and Otology 2007;121:807-815
- Johnson CM, Godin MS. The tension nose: Open structure rhinoplasty approach. Plastic and Reconstructive Surgery 1995;95:32-1052
- Toriumi DM. New Concepts in Nasal Tip Contouring. Arch Facial Plast Surg 2006;8:156-185
- Daniel RK. Rhinoplasty. An atlas of surgical techniques. New York: Springer; 2004:132-136
- Gruber R, Friedman G. A suture algorithm for the broad or bulbous nasal tip. Plast Reconstr Surg 2002;110:1752-1764
- Tardy ME, Walter MA, Patt BS. The overprojecting nose. Anatomic component analysis and repair. Facial Plast Surg 1993;9:306-316
- Rowe-Jones J, Van Wyk FC. Special considerations in northern European primary aesthetic rhinoplasty.Facial Plast Surg 2010;26:75-85
- Tebbetts JB. Primary rhinoplasty. Philadelphia:Mosby;2007
- Johnson CM Jr., Toriumi DM. Open structure rhinoplasty. Philadephia:Saunders;1990
- Peck GC. Techniques in Aesthetic Rhinoplasty (2nd Ed). Philadelphia:Lippincott;1990
- Gunter JP, Friedman R. Lateral crural strut graft: technique and clinical applications in rhinoplasty. Plast Reconstr Surg 1997;99:943-52
Rohrich RJ, Raniere J, Ha RY. The alar contour graft: correction and prevention of alar rim deformities in rhinoplasty. Plast Reconstr Surg 2002;109:2495-505