Each nose is unique with its own characteristics. The patient has an expectation considering to communal perception of beautiful nose, while, the surgeon’s goal is to create a nose that will be admired by the patient, the community, and the surgeon him/herself. There is no doubt that, understanding the patient’s goals is the major issue to meet the patient’s expectations.
Tip rhinoplasty is the most challenging but least understood part of the rhinoplasty operation. The initial challenge comes when the surgeon attempts to define the preoperative deformity of the nose. Facial analysis is critical for the diagnosis of the deformities and creating the ideal nasal tip. The surgeon relies on some personal judgment and a set of rules, proportions, angles, geometric relationships. Besides, he/she takes a number of variables including the strength of the cartilages, preexisting scarring, and the patient’s age, sex, ethnicity and skin quality into account. Then, he/she integrates aesthetic and anatomical standpoints to formulate a preliminary operative plan. In order to perform a successful tip rhinoplasty, the surgeon should know specific deformities and different techniques. Finally, the surgeon selects the most conservative technique from his/her armamentarium that will provide most reliable and favorable cosmetic result for the individual deformity with least amount of tissue distortion and disruption of tip-supporting mechanisms. While achieving the aesthetically beautiful nasal tip, the nasal function has to be protected as well. The experience, which means the surgeon’s ability to predict the long term outcome of these techniques is also important to sculpt an ideal nasal tip.
In order to facilitate the understanding of tip surgery, the chapter will begin with the essentials of tip anatomy, aesthetics, and analysis. Then specific tip deformities, tip rhinoplasty incisions, and approaches will be discussed. Finally, foundation of tip surgery and the tip suturing techniques will be given in detail with an in-depth discussion.
ANATOMY OF THE NASAL TIP
The surface anatomy of the nasal tip reflects the complex contours of the underlying framework and draping of skin. Recognition of the normal nasal tip anatomy is essential for precise facial analysis and eventually achieving successful rhinoplasty. The nasal tip is formed from skin, subcutaneous tissue, alar (lower lateral) cartilages, and the caudal cartilaginous septum. The subcutaneous tissue of the tip is generally thicker and richer from sebaceous glands than the rest of the nose. The thickness of the tip may show great individual variability. However, the surgeon has least control on this variant. While a finely sculpted tip appearance cannot be given to thick skinned patients, even minor asymmetries and irregularities might be visible in extremely thin-skinned individuals despite the best efforts of the surgeon.1 These limitations should be known by the surgeon in order to select the appropriate technique, and should be frankly discussed with the patient to make them have realistic expectations.
The complex contours of the alar cartilage largely define the nasal tip shape and support. Alar cartilage consists of three crura (medial, middle and lateral), and each of these two segments with distinct junction points of aesthetic importance. The shape of the alar cartilage looks like a flying bird: The wings composed by lateral crura, the body by the domes and the feet by the medial crura (Figure 1).1,2,3 The medial crus is the primary component of the columella, consisting of lower footplate segment and superior columellar segment. The superior columellar segment is the narrowest part of the columella and is vertically oriented. There is a correlation between the visual length of the nostril and superior columellar segment’s length. The shape of the medial crura may be straight, or divergent with a symmetrical or reciprocal curve. Medial crura are covered by soft tissue and this cover can affect the columellar appearance. If the distance between the medial crura are wide and soft tissue is thin, the appearance of tip is bifid; but if the soft tissue is thick, the appearance of columella is wide.
| 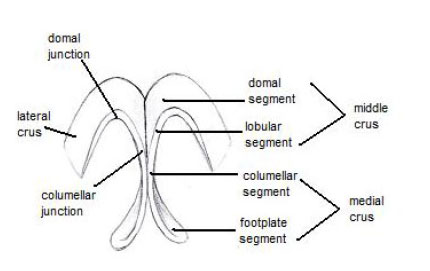 | Figure 1 | ||
 | ||||
| Figure 1 |
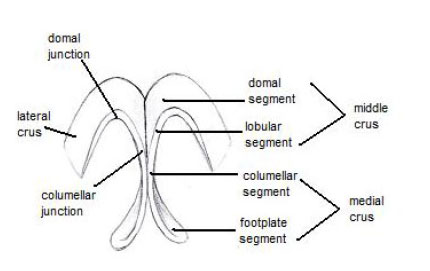
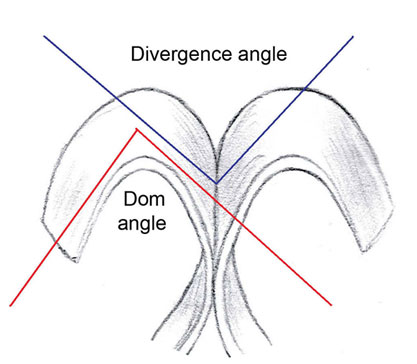
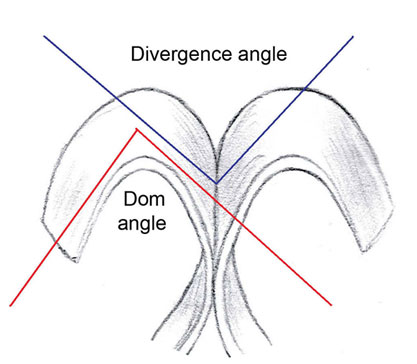
The middle crus consists of lobular and domal segments. Lobular segment follows the pattern of columellar segment of the medial crus. Variations in length of lobular segment are correlated with tip shapes and cause disproportionate nostril- lobular ratio. Domal segment is located between the lobular segment of middle crus and medial segment of lateral crus. The dome angle is the angle between the medial and lateral crus at the dome on each side (Figure 2).1,2,3 Caudally, the domal segment has a distinct domal notch which is correlated with the shape of soft triangle of the lobule. The change of the angulation and convexity of the domal segment directly affects the appearance of the tip. Cephalically, the domal segment is wide and adjoined to the opposite domal segment at the midline. Lateral crus begins at the domal junction and ends at the sesamoid cartilages chain which are placed in piriform aperture. The sesamoid complex is a chain of smaller cartilages that support the lateral crus, the septal cartilage, their ligaments and the maxillary spine. Generally the shape of the lateral crus is convex and curves slightly internally at the lateral end. While the lateral crus arches laterally, it moves cephalically as well. This lateral crural convexity causes a nice arch in the nasal tip.1,2,3 Ideally, the lateral crus curves laterally at an angle of 45º or more from midline and is directed towards the lateral canthus.4 More cephalically oriented lateral crus may cause fullness in the lower third of nose, underprojection of the tip, and parenthesis tip deformity5.
|  | Figure 2 | ||
 | ||||
| Figure 2 |
The entire alar cartilage shows great variability both among individuals and from side to side in the same individual. Its shape and length primarily affect the nasal tip aesthetics. Any modification at the lateral crus change the rotation, projection and shape of the nasal tip.1,2,3,6
Sheen7 defines four landmarks on the nasal tip: the point of differentiation (supratip breakpoint), right dome, left dome, columella-lobular junction (columella breakpoint). An aesthetically pleasing nose demonstrates a supratip breakpoint corresponding to a subtle depression cephalad to the nasal tip that visually distinguishes the tip from the nasal dorsum. Anatomically, the supratip break is a consequence of the projection difference between the domes of the lower lateral cartilages and the dorsal septal plane. This breakpoint is important aesthetically because it illustrates the nasal tip volume and marks the nasal bridge length. Dome or tip defining point is the most projected portion of the transition zone between the medial and lateral crus. The ideal axis of dome defining point is 45º from the midline. The line that connects two domes is called interdomal distance, showing how narrow or wide the nasal tip will appear on anterior view. Columella breakpoint marks the transition from columella to tip lobule. The columella should have a gentle double break (Figure 3).1,2,7,8 A straight columella due to inappropriate shortening of the septum causes unattractive appearance.
|  | Figure 3 | ||
 | ||||
| Figure 3 |
Sheen7 describes two important anatomical concepts to the surface aesthetics: the angle of divergence and the angle of rotation. The angle of divergence shows the separation between the middle crura which is 60° ideally, and an important factor in determining type of the tip deformity (Figure 2). The angle of rotation is measured at the columella breakpoint, and its average range is 50°-60° (Figure 3).7,8
Postoperative loss of tip support and projection is one of the most important iatrogenic sequels of rhinoplasty. Surgeon must know the major and minor tip support mechanisms and principals of intraoperative tip dynamics, and preserve or restructure the nasal tip integrity during surgery. Major mechanisms of tip support include the size, shape and elasticity of the medial and lateral crura, the attachment of the medial crural footplates to the caudal septum, and the attachment of cephalic margin of the lateral crura to the caudal margin of upper lateral cartilages. Minor tip supports include dorsal cartilaginous septum, membranous septum, interdomal ligaments, nasal spine, alar sidewalls, and the attachments to the skin. Radical excision of alar cartilages or other support attachments lead to loss of tip support and eventual tip ptosis. If any of the major tip support mechanisms is weakened during surgery, compensatory rearrangement should be done. 1,9,10
PREOPERATIVE EVALUATION
Careful analysis of the nasal tip and related facial futures is the first step of a successful tip rhinoplasty. Preoperative evaluation combines the patient’s concerns and anatomic properties with a set of rules, proportions, angles, geometric relationships. Besides, a number of variables such as the strength of the cartilages, skin quality, preexisting scarring, the patient’s age, sex, and ethnicity are taken into account during the evaluation.
Since tip analysis can be extremely complex and subjective, Daniel8,11 evolved 6 clinical characteristics to facilitate the decision on tip analysis: volume, definition, width, shape, position, rotation, and projection.
Volume
The size of the lateral crura determines the volume. If the lateral crus is too convex, the result is a rounded tip, and if it is too long in cephalic-caudal axis, the result is downward rotated tip.8,11
Tip Definition
Definition implies the degree of detail, refinement and angularity of the tip. Definition means giving shape to the dome-defining point, columella breakpoint, and supratip breakpoint. It is anatomically determined by the adjacent relationship between the slightly convex lateral crura and more convex domal segment with its surface expression revealed or obscured by the skin. Besides the shape of alar cartilages, skin has critical importance for tip definition.8,11
Width
The interdomal distance between the two tip defining points determines the width of nasal tip. Main reason of the excess width, in most cases, is the over-prominence of the lateral and middle crural junctions in the midline. The excess of soft tissue is responsible only in a few number of the cases. 2,8,11
Shape
Certain combinations of anatomical deformities determines the tip shape (see tip deformities).
Projection
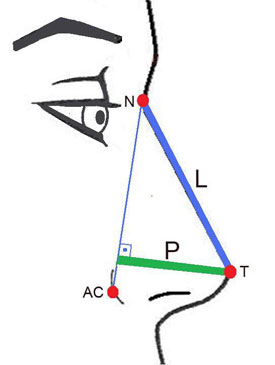
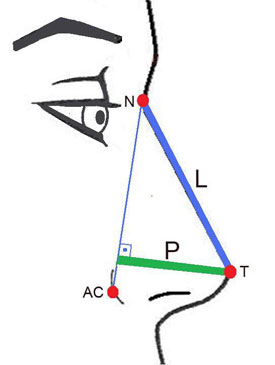
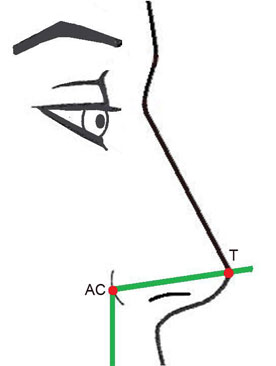
Tip projection is the distance between nasal tip and alar crease. According to Byrd12, tip projection should be the two-thirds (0,67) of the ideal dorsal length. Another method to evaluate projection was described by Goode13, a right triangle is created by drawing lines from the nasion to the alar-facial groove; a second line perpendicular to this through the tip defining point which measures tip projection; and a line from the nasion to the tip, which measures nasal length (Figure 4). With this method the ideal ratio of tip projection to nasal length is 0,55 to 0,6:1.
|  | Figure 4 | ||
 | ||||
| Figure 4 |
Position
Tip position is defined as the location of the tip along the dorsal line (N-T) and has great importance in shortening the long nose (Figure 4). The changes at radix can dramatically affect the dorsal line, which creates an illusion that tip position has been altered.8,11
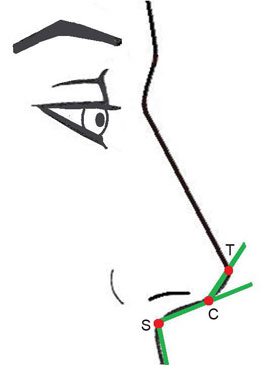
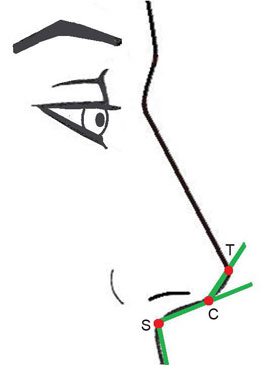
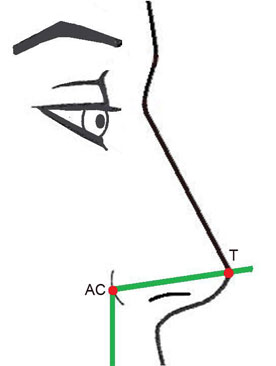
Rotation
Tip rotation is defined as upward or downward movement of the tip along a circular arc consisting of a radius centered at the alar crease extending to the tip defining point. Since the nasolabial angle can be greatly affected by adjacent structures (Figure 3), tip rotation can be better evaluated with tip angle11. The tip angle is the wide angle between the vertical line passing through the alar crease and a second line that is drawn from the alar crease to nasal tip, on lateral view (Figure 5). The ideal tip angle is 105º in females and 100º in males. 11
|  | Figure 5 | ||
 | ||||
| Figure 5 |
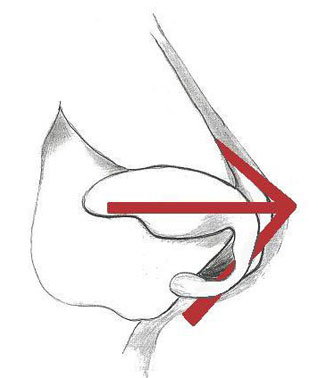
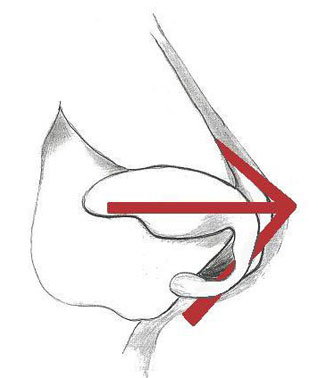
Tripod concept:
Since 1960’s, Anderson’s tripod concept has been the main theory used to explain the nasal tip dynamics and the effects of various surgical procedures on tip rotation and projection.14 The central leg of the tripod is formed by the medial crura and the other two legs are formed by the lateral crura (Figure 6). Selective increase or decrease in the length of the tripod legs can be used to adjust the degree of desired tip projection and/or rotation. Shortening the central leg (conjoined medial crus) decreases projection and rotation, whereas shortening the two superior legs (lateral crura) increases rotation and decreases projection. 1,6,9,10,14
|  | Figure 6 | ||
 | ||||
| Figure 6 |
SPECIFIC TIP DEFORMITIES
Accurate diagnosis of the underlying problem is the first step for successful tip rhinoplasty. The surgeon should be aware of specific deformities, different techniques to correct these, and choose the most conservative technique individually. The common tip deformities causing broad or wide tip appearance, and treatment options are summarized below:
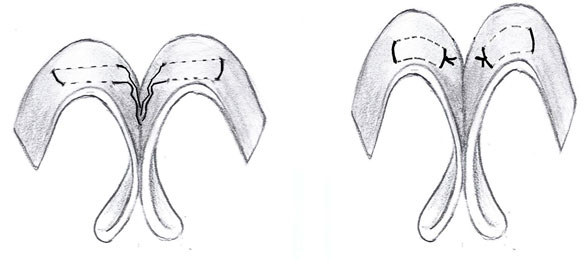
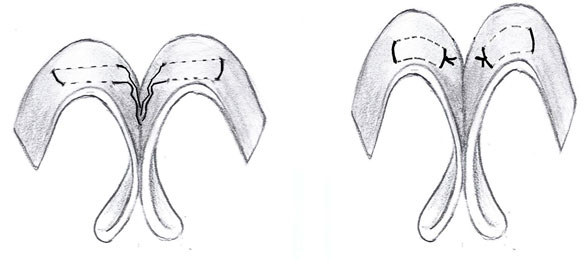
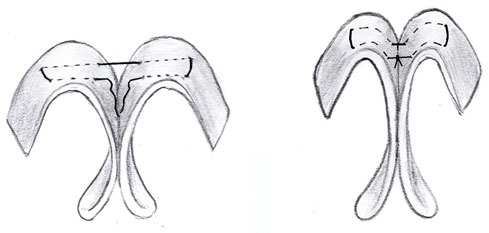
Bifid tip: In the bifid tip, alar cartilages are placed apart and prominently convex, so a dimple appears between them (Figure 7 a, b). Angle of divergence is variable. Treatment may have three steps: 1. Excision (cephalic trim) of over-prominent alar cartilages especially at middle crura and remove any intervening soft tissue 2. Suture techniques to converge the middle crura which cause disappearance of bifidity. 3. Crushed cartilage grafts for filling the soft tissue defect if needed. 2,8,15,16
| a.  | b.  | Figure 7 | |||
a.  | ||||||
b.  | ||||||
| Figure 7 |
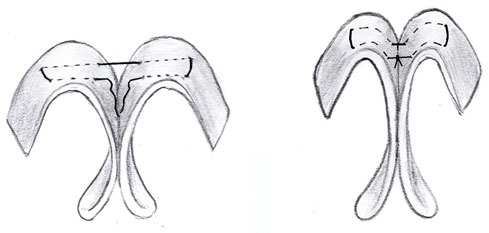
Bulbous tip: It is diagnosed as having prominent, high volume alar cartilages, and light reflexes at the lateral border of the alar cartilages, instead of the tip point (Figure 8 a, b). Anatomically the flat domal segment is in continuity with a broad convex lateral crura. Surgical highlights are to decrease volume, augment the domal definition and to decrease lateral crura width. Tip suture techniques are sufficient for these purposes. 11,15,16
| a.  | b.  | Figure 8 | |||
a.  | ||||||
b.  | ||||||
| Figure 8 |
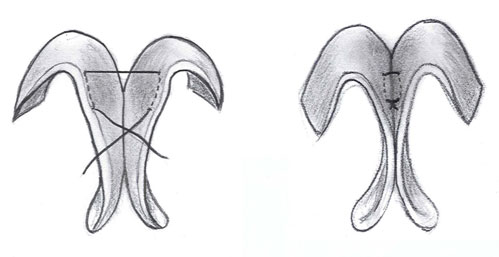
Boxy tip: The boxy tip has a characteristic broad, rectangular shape (Figure 9 a, b) especially on basilar view. Rohrich and Adams17 defined three types of boxy tip anatomically. Type 1, which has increased angle of divergence (greater than 30°), and normal domal arc (4mm or less); Type 2, which has normal angle of divergence (30° and less) and wide domal arc; and Type 3, which has increased angle of divergence and wide domal arc. The goal of the operation for correction of the boxy tip is to create a triangular nasal tip at the basal view by repositioning the tip defining points, making angulation to the domes and giving new shape to the lateral crura. A columellar strut may be necessary in order to make a rigid tip support and restore columella angle. Interdomal or transdomal tip suture techniques following the cephalic trimming of alar cartilages are favored, but cartilage resection techniques can be used as alternative if the cartilages are not pliable enough to comply. Lateral crural spanning sutures may be used to correct lateral alar convexity. Weakness in the alar rims or lateral crura can be strengthened with alar rim grafts or lateral crural strut grafts if necessary. 15,17,18
| a.  | b.  | Figure 9 | |||
a.  | ||||||
b.  | ||||||
| Figure 9 |
Ball tip: Large convex alar cartilages give the tip round and circular appearance on anterior view (see the case example). Ball tip has ideal angle of divergence.5 Too large alar cartilages and ill defined shapes are major surgical problems. If the lateral crura are more convex along their cephalic rims, excision of a cephalic strip corrects the ball appearance. Major excision of the middle crura may lead to a significant decrease in projection. Transdomal suture techniques can be used if cephalic excision of cartilages comes inadequate for correction.
Tip grafts may be used to maintain appropriate tip definition and projection. If a low, flat dorsum or excessive narrowing of the nasal base by the alar wedges is the reason for tip ball appearance, raising the dorsum can solve the problem.19 If the thick subcutaneous tissue and skin is the underlying problem, removal of excess subcutaneous tissue can be helpful. Cephalically oriented lateral crura can also cause the ball tip appearance and should be corrected accordingly.20
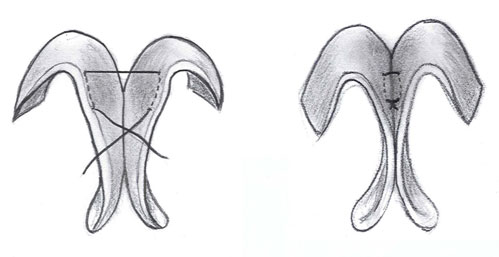
Parenthesis Tip: This deformity is caused by the malposition of the alar cartilages. Cephalically oriented, bulbous lateral crura typically create a “parenthesis” appearance on frontal view (Figure 10 a, b). Lateral crura are placed 30° from midline and directed towards the medial canthus, instead of the normal oblique orientation of 45° from midline towards the lateral canthus. There is a broad, flat, weakened nasal tip. Basal perimeter’s shape is square. Nasal valve insufficiency, underprojection and boxy tip may attend the cephalically oriented lateral crura. Patients with cephalic positioning of the lateral crura require a completely different approach to change the nasal tip contour. In patients with bulbous, cephalically positioned lateral crura, one can perform a cephalic trim and dissect the lateral crura from the vestibular skin, suture lateral crural strut grafts to the undersurfaces of the lateral crura, and then reposition them into caudally positioned pockets. If the cephalically positioned lateral crura are flat and do not contribute to tip bulbosity or middle vault width, they can be left in position, using alar batten or lateral crural grafts to support the lateral nasal wall.20
| a.  | b.  | Figure 10 | |||
a.  | ||||||
b.  | ||||||
| Figure 10 |
Bulky tip: The bulky tip is characterized with thick skin with a heavy nasal base which is imbalanced with the rest of the nose (Figure 11 a, b). It has no definition or other tip characteristics, but merely volume.
| a.  | b.  | Figure 11 | |||
a.  | ||||||
b.  | ||||||
| Figure 11 |
The skin and subcutaneous tissues are very thick and cannot be thinned enough even with open debulking. Underlying alar cartilages may be in normal shape but they cannot take part in appearance because of the thick skin cover. Suture techniques are usually not efficient and rigid tip grafts are needed to sharpen the tip contours. Since narrowing the rest of the nose makes the bulky tip appearance more significant, lateral osteotomies and dorsal lowering should generally be avoided. Alar base reduction must include sufficient amount of outer skin excision. Patients should be informed to have limited expectations because of the skin quality.8,10
In addition to the above mentioned tip deformities, the patients with excessively thin skin require a specific attention. Extremely thin skin has limited subcutaneous tissue and cannot camouflage even minor skeletal irregularities or contour deficiencies. These patients also tend to have undesirable, unnatural appearance due to progressive skin retraction over several years.10 Solid, sharp contoured grafts and cartilage resections are not preferred since even small irregularities will be prominent. Fascia grafts or crushed cartilage grafts are useful to camouflage the deformities and avoid an operated nose appearance.11,21,22
OPERATIVE PROCEDURE
Cosmetic adjustment of nasal tip involves a combination of incisions, approaches, and tip altering maneuvers for a desired postoperative result. There is no single procedure that can successfully correct every deformity in an aesthetically pleasing fashion. Therefore the surgeon must be skilled in various approaches and maneuvers for a wide range of nasal anatomic combinations.
Incisions
Nasal incisions are used to provide access to the underlying structures in rhinoplasty procedure. Inter-cartilaginous incision is located between the upper and lower lateral cartilages. Recently, this incision has begun to be placed 1 to 2 mm. caudal to the valve on the lateral crura side to prevent nasal valve stenosis. Inter-cartilaginous incision weakens the major tip supporting mechanism between the upper and lower cartilages. Intra-cartilaginous (trans-cartilaginous) incision is located in the vestibular skin and the lateral crus, 4-5 mm cephalic to the caudal margin of the lateral crus. It is useful when making a cephalic strip resection of the lower lateral cartilages to achieve greater tip rotation. The intra- and inter-cartilagenous incisions can be combined with a hemi or full transfixion incision for access to the anterior septal angle and dorsum. Infra-, cartilaginous (marginal) incision follows the caudal border of the lower lateral cartilages. 10,23
Approaches
Approach is the specific anatomical dissection providing surgical exposure of the skeletal structures. Intranasal (nondelivery, delivery) or external (open) surgical approaches can be used for tip rhinoplasty. The choice of approach is based on the complexity of the tip deformity, and experience of the surgeon.
1. The Nondelivery Approaches
The nondelivery approaches can be performed either via transcartilaginous (transcartilaginous approach) or intercartilaginous (retrograde approach) incisions to make cephalic trimming of the lateral crura with least dissection, tissue manipulation and damage to tip support structures. 8,10 Nondelivery approaches allow conservative volume reduction and little tip rotation without destruction of domes. They are most effective in patients with good domal configuration, minimal tip bulbosity, medium skin thickness, tip cartilage symmetry, and only requiring modest volume reduction of the cephalic margin of the lateral crura.
2. The Delivery Approach
In case of more severe (widely arched, bifid, or bulbous) tip deformities, delivery approach provides better exposure that allows more radical tip alterations such as suture narrowing and interrupted strip techniques. Delivery approach involves inter-cartilaginous and infra-cartilaginous incisions with anterior delivery of the lower lateral cartilages out of the nostril as a bipedicled chondrocutaneous flap. Direct visualization of alar cartilages is the advantage of this approach but destruction of cartilages and alteration of domal configuration are the risks of this procedure. 10,23
3. Open / External Rhinoplasty Approach
The open approach provides maximal exposure for accurate diagnosis of the deformity and careful alignment of the structures. It involves bilateral marginal incisions connected by a transcolumellar incision at the midcolumella. In order to obtain an ideal scar, midcolumellar incision is shaped as inverted-V, as recommended by Goodman and Charbonneau24. All difficult problems requiring advanced tip work are best handled under direct visualization through open approach. It allows precise placement of sutures and grafts. The main disadvantage of this procedure is potential scar formation at columellar incision site. However, if the incision is properly placed and sutured, the scar is rarely noticed and almost disappears with time. Although the open approach does not divide any major tip support mechanisms, the wide surgical dissection site heals with more scar tissue that may create forces to pull structures in unwanted directions. Therefore, extra support with grafting is more important in open approach. Although rare additional tip edema seen especially in patients with thick skin, can be relieved by subdermal steroid injections. 6,10,23
TIP RHINOPLASTY AND SUTURE TECHNIQUES
There is variety of surgical options when performing a cosmetic tip rhinoplasty. The unique tip anatomy of each individual rhinoplasty patient, aesthetic judgment and experience of the surgeon, and the patient’s expectations determine the selection of the techniques used in nasal tip surgery. The surgeon should know and aptitude the options, and choose the techniques that will provide the most reliable and favorable cosmetic result for the individual deformity with least amount of tissue distortion and disruption of tip-supporting mechanisms.
The destructive techniques such as morselizing, scoring, and interrupted strip techniques may decrease the intrinsic strength of alar cartilages and often lead to distortions of the lobule due to wound contraction forces. The failure of these techniques motivated a philosophy of preserving all or most of the alar cartilage and using grafts to alter the shape, projection and the position of the tip, and provide extra support as well. However, the grafting techniques carry the potential risks of asymmetries, visible irregularities, malpositioning, and displacement. For these reasons, suture techniques have been adopted as the primary method for recontouring of alar cartilages. The suture techniques reduced the need for grafts, allowed the surgeon to manipulate the tip with high degree of precision and better long term clinical outcome.
Although the suture techniques are as old as rhinoplasty operation, they have been popular after the second half of 1980s. Joseph25 occasionally used sutures named “orthopedic suture” to secure the tip cartilages to the caudal septum which is called today as columella-septal sutures. Dome-type sutures were first introduced in 1926 by Sebileau and Dufourmentel26. McCollough and English27 reintroduced and Tardy et al.28 popularized a single bidomal spanning suture passed through the both the intermediate and lateral crura using endonasal approach.
Daniel29 introduced these techniques to the open approach rhinoplasty and implemented a separate suture to shape each dome, namely dome creation suture (current transdomal suture). Tebbetts30 introduced lateral crural spanning suture and also leaded to replace the scoring and resection philosophy with that of the suture control. Supreme results of the tip suture techniques with a variety of names allowed surgeons to manipulate the nasal tip shape with high degree of precision. A number of suture algorithms was also described to correct specific wide or broad tip deformities. In 1989, Tebbets presented the first specific sequence of suture placement, and published a systematic approach in 1994. Later, Daniel31 proposed an algorithm combination of columellar, domal creation, and domal equalization sutures, called “three stich tip technique” for the wide variety of tip deformities. Rohrich and Adams17 proposed a suture algorithm specifically designed for the boxy tip that basically involved limited domal and cephalic trim, followed by transdomal and/or interdomal sutures. Gruber and Friedman16 advocated four suture algorithm for bulbous or wide tip: , transdomal, interdomal, lateral crural mattress, and columella-septal sutures.
Tip suture techniques can effectively control the shape and curvature of the alar cartilage while preserving its all structural integrity. They are immediately visible intraoperatively, and can be reversed, or adjusted. They can be successfully used for the patients with poor definition, excessive width, inadequate projection, and plunging tips. The techniques can be combined with other techniques such as tip grafts, lateral crural struts, alar rim grafts to achieve the desired goal as well. It is relatively difficult to obtain an optimal result with suturing techniques alone, in patients with thick skin, overprojected tips, and compromised alar cartilages.11,16,17
Principles of Suture Techniques
Prior to contouring the nasal tip, stabilizing the nasal base will ensure that tip projection will be maintained postoperatively. The surgeon must stabilize the base of the nose with a columellar strut, suturing the medial crura to the caudal septum. Columellar strut is placed in a pocket dissected between the medial crura just above the nasal spine and 1-2 mm below the domes. Columellar strut as an independent but integral part of tip rhinoplasty provides excellent support to tip, increases tip rigidity, gives strength and rigidity to columella, rectifies any buckling of medial crura. The size of the strut varies in size to adjust tip projection and rotation to fit nasal requirements11,16,23.
Following the stabilization of the tip, domal definition usually becomes the next goal. In patients requiring limited refinement of the nasal tip, conservative cephalic resection of the lateral crura provides subtle narrowing of the tip and supratip.
The other effects of cephalic resection are increasing tip rotation and decreasing tip projection. Since maintaining a complete (uninterrupted) strip of alar cartilage and preserving the majority of alar cartilage warrant little risk of postoperative deformity secondary to loss of tip support, preserving at least 5 to 7 mm of complete strip of alar cartilage is preferred10,16. If indicated, cephalic trim of the lateral crura is performed primarily medially and usually should not be extended into the lateral third of the lateral crus to avoid excessive supra-alar pinching and lateral wall collapse. The amount and strength of the cartilage is important for its successful manipulation with sutures as well. It is difficult to use the sutures to reshape the overresected cartilage especially when there is little cartilage to grasp and/or the cartilage is too weak to support the new shape. Prophylactic placement of alar batten grafts in a pocket just medial to the supra-alar crease may be needed to prevent collapse of the lateral wall16,18,20.
Most of the postoperative problems secondary to the suture techniques are often the confirmations of intraoperative suspicions and preventable with easy prophylactic maneuvers. For example, the mild or moderate pinching observed intraoperatively may become more prominent and may cause alar collapse years after the surgery as a result of the scar contracture process that shrinks the skin envelope over the modified tip structure. Tying the knots not too tight, and/or prophylactic placement of lateral crural strut or alar batten graft will prevent such problems and potential revision surgery.
Frequently 5-0 sutures are preferred for delicate cartilages. The choice of suture type is important. The nonabsorbable sutures have a potential for late complications such as infection, foreign body reaction, and extrusion especially in cases with poor soft tissue coverage above the suture. If the absorbable suture material is lost earlier than the time needed to maintain the shape due to intrinsic forces, the reshaped cartilage is naturally prone to return to its initial position. The permanence of cartilage reshaping does not depend on durability of suture material after the formation of scar tissue. Since 2 to 12 weeks are enough for the formation of scar tissue that will maintain the shape in place, long lasting absorbable suture materials (e.g. polydioxanone) can be preferred to stabilize the reshaped cartilage as effective as nonabsorbable sutures without causing potential complications.32
When the patient has strong cartilages or maximal change is desired, undermining the vestibular skin beneath the domal segment and subcutaneous passage of the suture (without penetrating the skin) is recommended.
Subcutaneous suture protects the surrounding skin, which is an important barrier for external infective agents. Since this barrier is not intact in transcutaneous (penetrating the skin) suturation, it carries higher infection and extrusion risks that may in turn result early loss of suture materials. In addition, the direct contact between facing cartilage surfaces in the subcutaneous suturation technique promotes fibrotic tissue formation, stabilizes the reshaped cartilage, and may better protect the shape. In contrast, the presence of skin or mucosa on the undersurface of the cartilage in the transcutaneous suturation may impede the fibrocartilaginous proliferation and consequent stabilization of the reshaped cartilage.32
SUTURE TECHNIQUES
Each tip characteristic can be achieved using a specific suture. Different types of sutures were introduced to manipulate the tip. The different names have also been used for the some similar sutures in the literature. Proper selection of appropriate technique or combination of techniques require understanding the impact of the manipulations on tip structures and eventually on appearance. The most commonly used tip suture techniques -see the video for the senior author’s (OC) technique-, their indications, functions, and side effects are discussed hereafter:
Medial Crural Fixation Suture
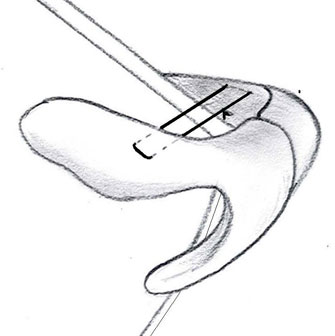
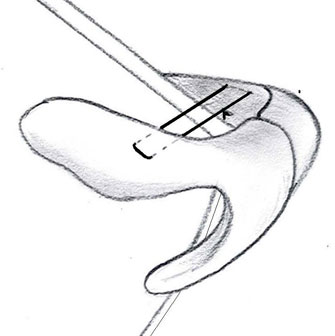
Medial crural fixation suture is used to fixate the medial crura to columellar strut and provide foundation for subsequent suture contouring of the domes and lateral crura. The suture stabilizes the aligns the base of the alar arches, and equalizes the initial projection of the domes. First a needle is inserted to secure the position of the crura and the strut, then a horizontal mattress suture is placed through the both medial crura and the strut (Figure 12). The domal symmetry can be adjusted and tip projection can be increased as necessary. Usually two sutures are preferred to accomplish the fixation: first one is placed at the point below the divergence of the middle crura not to narrow the divergence angle, second one is placed at the base of the columella. In order to avoid obliterating of the natural flare of the caudal borders, the suture is placed in the midportion of the medial crura. 11,33
|  | Figure 12 | ||
 | ||||
| Figure 12 |
Transdomal (Dome Creating, Dome Binding, Domal Definition) Suture
In most primary rhinoplasty cases, the problem is convex lateral crura/flat dome. For such cases, transdomal sutures are very effective to flatten the lateral crura and decrease the horizontal contribution to the bulbous nasal tip contour. These sutures narrow the tip, increase tip rotation and projection. Sutures are usually positioned 2-3 mm on either side of the required tip defining point, inserted in a horizontal mattress fashion, and the knots are tied medially between the domes (Figure 13). Using two separate single dome sutures is usually preferred to prevent the normal divergence of the intermediate crura.
|  | Figure 13 | ||
 | ||||
| Figure 13 |
After placement of the single dome sutures, an interdomal or a double dome suture (a suture that pinches both domes together) (Figure 14) may be used to further narrow the tip by bringing the domes close together. However, these attempts to unify the domes tend to obliterate the normal columella lobular (double break) angle and may eliminate the desirable divergence between the intermediate crura.11,20,34-36
|  | Figure 14 | ||
 | ||||
| Figure 14 |
The objectives of the transdomal sutures are narrowing the dome angle and creating flat lateral crura. The stiffness of the lateral crura and tightness of the sutures are important variables in obtaining optimal results with transdomal sutures. As with all sutures, the suture should be tied only as tight as required, for an optimal and natural result. If the patient has stiff cartilages, too tight dome sutures may cause pinching of the domes and lateral wall collapse which might become more prominent within time after surgery. Retying the knots looser or placement of lateral crural strut or alar batten graft will prevent the problem. If the patient has soft cartilages, increasing the tightness of transdomal sutures may pinch or buckle the dome, increase the convexity of the lateral crus laterally and eventually increase the resistance of the bulbosity. Combining the placement of lateral crural strut with the transdomal sutures may be useful to stiffen and decrease the bulbous appearance of lateral crus.11,20,34-36
The transdomal sutures may cause the lateral crura caudal margin to displace below its cephalic margin. This may compromise the support of the alar lobule and alar margin and result in loss of the normal transition from tip lobule to alar lobule. In such patients, alar rim grafts may be used to support the alar margin and create a defined ridge between the tip and alar lobule.20,36,37 A modification of the transdomal suture, named as hemitransdomal suture, which passes only the posterior part of the cephalic end of the dome may be useful to minimize the pinched tip.38 Transdomal sutures may change the location of tip defining point more cephalically as well. Tip defining point can be adjusted by final trimming of the cephalic middle crura and/or with tip grafts.
Interdomal Suture
The interdomal suture is a simple vertical interrupted suture placed in between the domes of the middle crura. The suture is usually placed at a level approximately 3-4 mm posterior to the dome, preserving the normal separation between the domes (Figure 15). This suture is primarily useful to set the width between the domes: increasing the tightness of the suture decreases the distance between the domes. It narrows the tip, also increases tip projection. This suture should not be tied too tightly; otherwise, the domes will come too close together, natural divergence between the intermediate crura will be eliminated and columellar lobular angle will be blunted. 11,20
|  | Figure 15 | ||
 | ||||
| Figure 15 |
Domal Equalization (Domal Stabilization) Suture
Once domal definition is satisfied, domal equalization suture may be used to insure the symmetry and narrow the tip deficiency. A simple interrupted buried suture is placed between the cephalic ends of domal segments (Figure 16). The suture enables correction of subtle changes in mild tip asymmetry and irregularities in domal height and provides subtle narrowing of the interdomal distance.11,39
|  | Figure 16 | ||
 | ||||
| Figure 16 |
Lateral Crural Spanning Suture
Lateral crural spanning sutures are best used to correct lateral crural convexity that are present bilaterally and located more than 5-6 mm lateral to the dome point (boxy tip configuration). Initially the convexity of the lateral crura identified, and a needle is placed across both lateral crura. Then horizontal mattress suture is inserted and tightened incrementally. The one arm of the suture can be passed through the dorsal septum to increase cephalic rotation of the tip complex (Figure 17). The width and slope of the supratip can be adjusted by changing the tightness of the suture as well. The notching of the alar rims should be avoided, and a lateral crural strut may be required to prevent this problem. The technique applies equal force to both lateral crura. If there is asymmetry between the lateral crura due to intrinsic kinks, bends or dense segments in one of the alar cartilage, this technique can not produce symmetry. Unilateral lateral crural spanning suture from lateral crural convexity to the dorsal septum, or a lateral crural mattress suture can be used for such cases.11,33,40
|  | Figure 17 | ||
 | ||||
| Figure 17 |
Lateral Crural Mattress Suture
This suture is designed to shape and reposition the lateral crus, especially reducing its convexity. If the transdomal sutures do not reduce convexity of the lateral crus, lateral crural mattress suture may be used to obtain a flat lateral crus. The area of maximal convexity of the lateral crus is grasped with a forceps, perpendicular to the axis of the lateral crus, a suture is passed through the lateral crus on one side of the forceps, then the other side of the forceps and tied. The width of the mattress should be approximately 6-8 mm for optimal result (Figure 18). The suture not only narrows and improves the lateral crura bulbosity, but also increases the tip projection. Overtightened suture may cause notching of the alar rim.16,40
|  | Figure 18 | ||
 | ||||
| Figure 18 |
Columella-Septal Suture
Columella-septal suture is used to adjust the tip height and/or rotation. A mattress suture is passed from the caudal surface of columella at the point of divergence of the intermediate crura and extended through the caudal septum (Figure 19). The suture reestablishes the tip strength and integrity, helps to threat hanging columella, provides tip rotation and little tip projection, and may reduce the overprojected tip.16,33 The projection and rotation can be adjusted depending on the location and the tightness of the suture on caudal septum. Daniel described two variations (rotation and projection sutures) of the columella-septal suture to specifically address the rotation and projection.11 However, usually a single columella-septal suture can control the desired tip projection and rotation if placed correctly.
|  | Figure 19 | ||
 | ||||
| Figure 19 |
CASE EXAMPLE
A 30 years old male patient presented with the concern of wide and droopy nasal tip. The examination revealed middle vault collapse, too large (both in vertical and horizontal direction), ball shaped, convex lateral crura, and underprojected, droopy tip (Figure 20 a, b, c)
| a.  | b. 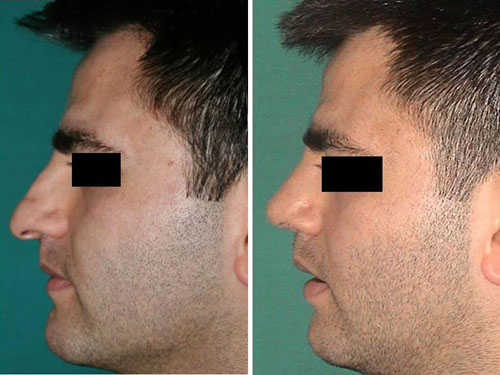 | c.  | d.  | Figure 20 | |||||
a.  | ||||||||||
b. 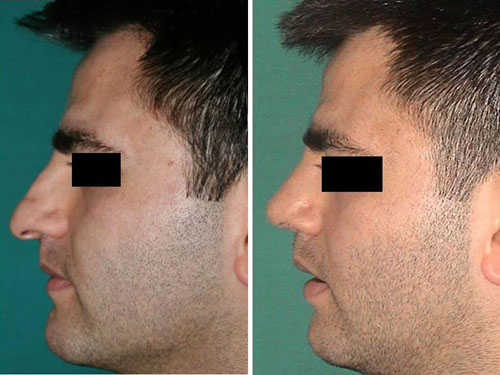 | ||||||||||
c.  | ||||||||||
d.  | ||||||||||
| Figure 20 |
Operative Technique (Figure 20 d):
Open approach
Caudal septal resection for droopy tip
Minimal bony hump reduction by rasping
Spreader grafts to correct the middle vault collapse
Stabilization of the nasal base with columellar strut and middle crural fixation suture prior to tip sculpturing
Tip definition with cephalic trimming of lateral crura, and underlying placement of lateral crural strut to prevent alar collapse
Transdomal, and double dome sutures for additional tip refinement, projection, and rotation. Columella-septal sutures to increase the rotation
Moderately crushed cartilage onlay grafts for concealing dorsal irregularities, and significantly crushed cartilage onlay tip graft to soften the tip contour.
REFERENCES
1. Larrabee WF, Makielski KH, Henderson JL. Nose. In: Surgical anatomy of the face, 2nd edition. New York: Lippincott Williams &Wilkins; 2004. p. 147-166.
2. Daniel RK. The nasal tip: Anatomy and aesthetics. Plast Reconstr Surg. 1992; 89(2): 216-224.
3. Steela NP, Thomas RJ. Surgical anatomy of the nose. In: Stucker FJ, et al. editors. Rhinology and Facial Plastic Surgery. Heidelberg: Springer-Verlag Berlin; 2009. p. 5-13.
4. Sepehr A, Alexander AJ, Chauhan N, Chan H, Adamson PA. Cephalic positioning of the lateral crura: implications for nasal tip-plasty. Arch Facial Plast Surg 2010; 12(6): 379-384.
5. Constantian MB. The boxy nasal tip, the ball tip, and alar cartilage malposition: variations on a theme. A study in 200 consecutive primary and secondary rhinoplasty patients. Plast Reconstr Surg 2005; 116(1): 268-281.
6. Whitaker EG, Johnson CM Jr. The evolution of open structure rhinoplasty. Arch Facial Plast Surg 2003; 5(4): 291-300.
7. Sheen JH, Sheen AP. Aesthetic Rhinoplasty. St. Louis, Mosby –Year Book Inc; 1987.
8. Daniel RK. The Nasal Tip. In: Daniel RK editor. Aesthetic Plastic Surgery Rhinoplasty. Boston: Little, Brown and Company,1993. p. 215-281.
9. Tardy ME. et al. Rhinoplasty. In: Cummings CW, editor. Otolaryngology Head and Neck Surgery. St Louis, Mosby–Year Book Inc; 1998. p. 949-999.
10. Tardy ME, Toriumi DM, Hecht DA. Philosophy and Principles of Rhinoplasty. In: Papel ID et al, editors. Facial Plastic and Reconstructive Surgery. New York: Theeme Medical Publishers, Inc; 2002. p. 369-389.
11. Daniel RK. Tip. In: Rhinoplasty: An Atlas of Surgical Techniques. New York, Springer-Verlag New York Inc; 2002:59-139.
12. Byrd HS, Hobar PC. Rhinoplasty: A practical guide for surgical planning. Plast Reconstr Surg 1993; 91(4):642-654; discussion : 655-656.
13. Goode RL. A method of tip projection measurement. In: Powell N, Humphrey B,editors. Proportions of the Aesthetic Face. New York, NY: Thieme-Stratton Inc; 1984. p. 15-39.
14. Anderson JR. A reasoned approach to nasal base surgery. Arch Otolaryngol 1984; 110(6): 349-358.
15. Daniel RK. Surgical techniques for broad, boxy, and ball tips. Op Tech Plast Reconstr Surg 2000; 7(4): 213-223.
16. Gruber RP, Friedman GD. Suture algorithm for the broad or bulbous nasal tip. Plast Reconstr Surg 2002: 110(7):1752-1764; discussion :1765-1768.
17. Rohrich RJ, Adams WP Jr. The boxy nasal tip: classification and management based on alar cartilage suturing techniques. Plast Reconstr Surg 2001; 107(7):1849-1863; discussion: 1864- 1868.
18. Tebbetts, JB. Secondary tip modification: Shaping and positioning the nasal tip using nondestructive techniques. In: Primary Rhinoplasty: A New Approach to the Logic and the Techniques. St. Louis: Mosby- Years Book , 1998. p. 261-441.
19. McKinney P. Management of the bulbous nose. Plast Reconstr Surg 2000; 106(4):906-917; discussion: 918-921.
20. Toriumi DM. New concepts in nasal tip contouring. Arch Facial Plast Surg 2006; May-Jun;8(3): 156-85.
21. Tarhan E, Cakmak O, Ozdemir B, Akdogan V, Suren D. Comparison of AlloDerm, fat, fascia, cartilage and dermal grafts in rabbits. Arch Facial Plastic Surg, 2008, 10 (3): 187-193.
22. Cakmak O, Buyuklu F. Crushed cartilage grafts for concealing irregularities in rhinoplasty. Arch Facial Plast Surg 2007; 9(5): 352-7.
23. Quatela VC, Slupchynskyj OS. Surgery of the nasal tip. Facial Plast Surg 1997; 13(4):253-68.
24. Goodman WS, Charbonneau PA. External approach to rhinoplasty. Laryngoscope 1974; 84(12): 2195-2201.
25. Joseph J. Nasenplastick und sonstige Gesichtsplastik nebst einen Anhang ueber Mammaplastik. Leipzig: Verlag von Curt Kabitzsch, 1931.
26. Sebileau P and Dufourmentel L. Correction Chirurgicale des Difformites Congenitales et Acquises de la Pyramide Nasale. Delavigne, France: Librairie Louis Arnette,1926: 92–106.
27. McCollough EG, English JL. A new twist in nasal tip surgery: An alternative to the Goldman tip for the wide or bulbous lobule. Arch Otolaryngol 1985; 111(8) : 524-529.
28. Tardy ME Jr, Cheng EY, Jernstrom V. Misadventures in nasal tip surgery. Analysis and repair. Otolaryngol Clin North Am 1987; 20(4):797-823.
29. Daniel RK. Rhinoplasty: Creating an aesthetic tip. A preliminary report. Plast Reconstr Surg 1987; 80(6) : 775-783.
30. Tebbetts JB. Shaping and positioning the nasal tip without structural disruption: A new, systematic approach. Plast Reconstr Surg 1994; 94(1) : 61-77.
31. Daniel RK. Rhinoplasty: a simplified, three-stitch, open tip suture technique. Part I: primary rhinoplasty. Plast Reconstr Surg 1999; 103 (5): 1491-1502.
32. Cagici A, Cakmak O, Bal N, Yavuz H, Tuncer İ. Effects of different suture materials on cartilage reshaping. Arch Facial Plastic Surg, 2008, 10 (2): 124-129.
33. Baker SR. Suture Contouring of the Nasal Tip. Arch Facial Plast Surg 2000; 2: 34-42.
34. Tardy ME Jr, Patt BS, Walter MA. Transdomal suture refinement of the nasal tip: long-term outcomes. Facial Plast Surg 1993; 9(4): 275-84.
35. Pedroza F. A 20-year review of the “new domes” technique for refining the drooping nasal tip. Arch Facial Plast Surg 2002; 4(3) :157-63.
36. Toriumi DM, Checcone MA. New concepts in nasal tip contouring. Facial Plast Surg Clin North Am 2009; 17(1):55-90.
37. Constantian MB. The incompetent external nasal valve: pathophysiology and treatment in primary and secondary rhinoplasty. Plast Reconstr Surg. 1994; 93(5): 919-31; discussion 932-3.
38. Dosanjh AS, Hsu C, Gruber RP. The hemitransdomal suture for narrowing the nasal tip. Ann Plast Surg 2010; 64: 708-712.
39. Corrado A, Bloom JD, Becker DG. Domal stabilization suture in tip rhinoplasty. Arch Facial Plast Surg 2009; 11(3):194-197.
40. Tebbetts JB. Primary Tip Assessment and Modification. In: Primer Rhinoplasty A New Approach to the logic and the Techniques. St. Louis, Missouri, Mosby–Year Book Inc; 1998. p. 99-133.
Figure Legends:
Figure 1: The anatomical components of an alar cartilage.
Figure 2: The divergence and dome angles.
Figure 3: Nasolabial and tip rotation angles. T: tip, S: subnasale, C: columellar breakpoint.
Figure 4: Goode ratio for the evaluation of tip projection. P: projection, L: length, T: tip, N: nasion, AC: alar crease.
Figure 5: Tip angle for the evaluation of tip rotation. T: tip, AC: alar crease.
Figure 6: Tripod concept.
Figure 7: Pre and 2 years postoperative photographs (a: anterior, and b: oblique views) of a patient with bifid tip deformity. The patient had broad tip due to wide divergence angle. A columellar strut was placed, cephalic trimming of the alar cartilages including the middle crura, placement of medial crural fixation, transdomal, interdomal and columella-septal sutures were applied.
Figure 8: Pre and 1 year postoperative photographs of a patient with bulbous tip deformity (a: anterior, and b: lateral views). The patient had prominent lateral crura. A columellar strut was placed, cephalic trimming of the alar cartilages, placement of medial crural fixation, transdomal and columella-septal sutures were applied. A thin layer of crushed cartilage onlay tip graft was placed as well.
Figure 9: Pre and 3 years postoperative photographs (a: anterior, and b: lateral views) of a patient with boxy tip deformity. The patient had wide, rectangular shaped lateral crura. Placement of columellar strut, cephalic trimming of the alar cartilages, placement of medial crural fixation, transdomal, double dome and columella-septal sutures, and crushed cartilage onlay tip graft were applied.
Figure 10: Pre and 1 year postoperative photographs of a patient with parenthesis tip deformity (a: anterior, and b: oblique views). The patient had cephalicaly oriented lateral crura directed to the medial canthus (blue arrow), instead of lateral canthus (red arrow). The lateral crura were dissected from the vestibular skin, lateral crural strut grafts were placed and they were repositioned into caudally positioned pockets to correct the malposition. Columellar strut and crushed cartilage onlay tip grafts were used as well.
Figure 11: Pre and 2 years postoperative photographs (a: anterior, and b: oblique views) of a patient with bulky tip deformity due thick skin. Debulking of the subcutaneous fat, placement of columellar strut, transdomal suture, and sharp contoured shield graft were used for tip refinement.
Figure 12: Medial crural fixation suture.
Figure 13: Transdomal suture.
Figure 14: Double dome sutur.
Figure 15: Interdomal suture.
Figure 16: Domal equalization suture (marked as red).
Figure 17: Lateral crural spanning suture.
Figure 18: Lateral crural mattress suture.
Figure 19: Columella-septal suture.
Figure 20: Pre and 2 years postoperative photographs (a:anterior, b:lateral, and c: oblique views), and the Gunther Diagram (d) of a patient with ball tip appearance. See the text (Case Example) for the details.
