“He who masters the nasal tip, masters rhinoplasty” [1]
The nasal tip is arguably the most difficult aspect of rhinoplasty to master. The complex architecture of the nasal tip cartilages, ligaments, and soft tissue envelope of the nose are difficult to control surgically. Nasal tip dynamics, which can affect both function and aesthetics, are influenced in subtle and sophisticated ways by surgical maneuvers. Combined with the variability in healing and skin contracture that occurs after rhinoplasty it becomes nearly impossible to predict outcomes of rhinoplasty with complete certainty.
Numerous methods to understand and reproducibly alter the nasal tip have been described. Of the multitude of techniques and theories described, the one that has been the most widely cited and easily understood is the tripod concept of nasal tip dynamics first described by Jack R. Anderson in 1969 [2]. Although this concept is simple and valid, it does not reflect the more nuanced understanding we have of nasal tip dynamics today. In order to more comprehensively describe nasal tip dynamics, addressing such variables such as the lobule and lengthening of the medial or lateral crural footplates, the senior author proposed the M-Arch model in 2006 and subsequently described its use in describing nasal tip dynamics in the context of specific applications of rhinoplasty patients [3-5].
The M-Arch model is an expansion of the tripod concept devised to better understand the relative effects of tip-altering maneuvers on the major nasal parameters of length, projection, rotation, and lobule refinement. Ultimately, the tip defining point (TDP) is one of the most important variables to control to master the nasal tip. To better understand the M-Arch model, a review of nasal tip anatomy and dynamics is warranted.
Nasal Tip Anatomy and Dynamics:
The nasal tip is classically described as having major and minor support mechanisms. The major support mechanisms are the size, shape and resilience of the medial and lateral crura of the lower lateral cartilages, the fibrous attachment of the medial crura to the caudal border of the cartilaginous septum, and the fibrous attachment of the cephalic border of the alar cartilages to the caudal border of the upper lateral cartilages [6]. Although these classic descriptions found in rhinoplasty textbooks are important for beginning to understand nasal tip anatomy and dynamics, a simpler way to describe and understand the nasal tip is possible. Simply stated, the nasal tip is an assembly of cartilage and ligamentous connections draped by the skin and soft tissue envelope.
The nasal tip deserves further mention as there are a multitude of definitions. The nasal tip has been described as the conjoined medial crural (MC) and lower lateral cartilage (LLC) complex. The nasal tip defining point (TDP) is the most anterior projection of the tip cartilages, usually corresponding to the apex of the lobular arch anatomically, and is typically identified externally where the light reflex is seen on the nasal tip (Figure 1). The nasal base includes the nasal tip in addition to the columella, alar side walls, and nasal sill. The nasal lobule includes the soft tissue anterior to the nostril apex, caudal to the supratip break of the nasal dorsum and tip junction, and anterior to the lateral alar side walls. The thickness and nature of the skin and soft tissue envelope (S-STE) are critical to the degree of definition reflected in the lobule.
The cartilaginous structure of the nasal tip composed by the configuration of the lower lateral cartilages and their interplays with surrounding structures are the key elements when utilizing the tripod theory and the M-arch model. The M-Arch, herein used to describe the configuration of the nasal tip, is composed of the conjoined medial, intermediate, and lower lateral cartilages. The medial crura start at the posterior septal angle where ligamentous attachments hold the footplates firmly. The medial crura then extend anteriorly to the angle at the apex of the nostril where each crus joins with the intermediate crus, defined as the portion of the tip cartilage that extends from the angle to the tip-defining point. From here, each lateral crus extends from the tip-defining point laterally to its junction at the pyriform fossa (hinge area).
Nasal tip dynamics also are related to a significant degree by the natural curvature of the lower lateral cartilages, especially in the region of the intermediate crura where the medial crura and lateral crura meet, creating a “sprung horseshoe” configuration. The opposing vectors of force include the anterior-inferior thrust of the lower lateral crura against the anterior-superior thrust of the medial crura. The summation of the vectors of oppositional forces yields the projection and rotation of the nasal tip. The tip defining point, nasal length, projection, and rotation are defined when considering the soft tissue and ligamentous contributions to the compromise of these rivalling forces (Figure 2).
One can begin to understand the complexity of nasal tip surgery, considered by many to be the most challenging aspect of rhinoplasty, which in and of itself is considered to be the most difficult of the facial plastic surgery procedures to consistently achieve predictably excellent results. Regardless of the philosophical or technical approach adopted, a thorough understanding of the nasal tip using the M-Arch model and its applications can be a powerful and reliable tool for the rhinoplasty surgeon.
Tripod Theory and M-Arch model:
The most commonly taught method for understanding nasal tip surgery and tip dynamics is based on Jack Anderson’s tripod theory. The nasal tip is likened to a tripod, where the paired medial crura form one leg and each of the lateral crura forms the other legs of the structure (Figure 3). When originally described in the 1960’s, rhinoplasty was mainly a reductive procedure and therefore only shortening of the middle and/or the lateral legs of the tripod was considered. By shortening the middle or lateral legs of the tripod, the tip would invariably be deprojected. The degree of shortening of each of the legs will definitively alter the position of the tip defining point, and thereby define the new nasal length, projection, and rotation. In accordance with the context of the era when this theory was described, the vast majority of the maneuvers performed lead to tip deprojection and increased tip rotation with shortening of the lateral crus, or tip deprojection and counter-rotation with shortening of the medial crus. The only exception to this was the Goldman type maneuver to increase tip projection effected by vertical division of the lateral crura lateral to the dome, and medialiazing this “borrowed” cartilage to increased the length of the medial crura.
Some applications of the tripod theory that are still applicable and important to understand are changes to the middle and lateral legs that can produce tip deprojection and alter rotation. For example, the middle leg of the tripod can be modified by excising the posterior septal angle or shortening the conjoined medial crura at their footplates. A vertical arch division would be a more powerful move to shorten the middle leg of the tripod. All of these maneuvers performed alone shorten the medial crura and without modifying the lateral legs of the tripod, would result in graduated amounts of tip deprojection, counter-rotation, and increased nasal length.
The lateral crura, representing the lateral legs of the tripod, can be approached in a similar graduated fashion. The lateral crura can be effectively “shortened” by simply releasing them at their junction with the pyriform aperture by incising through each lateral crus foot at the hinge area. The more lateral crus that is excised or overlapped, the more tip deprojection and rotation will result. Shortening the lateral crus alone without modifying the middle leg of the tripod would result in graduated amounts of tip deprojection, rotation, and decreased nasal length. This maneuver in isolation is used less now because of the potential for in-flaring of the hinge into the vestibule causing obstruction. The rhinoplasty surgeon must take the length of both the middle and lateral legs of the tripod into consideration as the summation of the altered vectors of each will determine the resultant location of the tip defining point.
Over the last 30 years, rhinoplasty has become significantly more sophisticated. The use of both autologous and alloplastic grafting in rhinoplasty has significantly increased in the practices of most rhinoplasty surgeons [7]. Although nasal length, projection, and rotation are the three most important factors to consider for favourable rhinoplasty outcomes, superior results are obtained when careful attention is paid to the intermediate crura, lobule, base, columella, and alar margin. As such, an extension and elaboration of the tripod theory was devised to address some of the emerging techniques and concepts in modern day rhinoplasty.
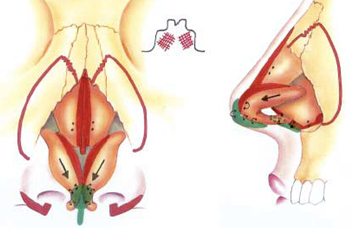
The M-Arch model is an elaboration and extension of the tripod theory which recognizes the importance of the length of each the medial, intermediate, and lateral crura as well as their overall length. Changes in the length of these subdivisions of the continuous parabolic lower lateral cartilages will produce changes in length, projection, rotation, and lobular definition. The M-Arch model recognizes the importance of changes that may occur by vertical division anywhere along the axis of the arch. This will produce variable yet reproducible changes in the aforementioned nasal parameters in addition to the lobule, ala-columella relationship, and lobule-base relationship. The lobule is represented by the domal arch, defined as the intermediate crura and the anterior-most aspect of the lateral crura (Figure 4).
Vertical arch division (VAD) is an important concept when utilizing the M-Arch model. Vertical division can be performed anywhere along the arch (Figure 5). Any division lateral (cephalad) to the tip defining point will produce rotation, decreased nasal length, and deprojection. Any division medial (caudad) to the tip defining point will produce counter-rotation, increased nasal length, and deprojection. Divisions that occur near the tip defining point will more preferentially affect rotation, whereas divisions near the crural feet will preferentially effect deprojection and subsequently nasal length. This phenomenon can be explained by examining the anatomy of the M-Arch. The greatest vertical dimensions are at the crural feet whereas the greatest horizontal dimensions are at the intermediate crura and anterior most aspect of the lateral crura (Figure 6). The degree of change in the nasal parameters of length, projection, and rotation is unique to each patient. Accurate diagnosis and analysis of the M-Arch, especially of the specific lengths of each of its component parts, in the context of the underlying bony skeleton and overlying skin and soft tissue envelope enables to rhinoplasty surgeon to more accurately predict the surgical results with a higher degree of confidence. Recently, the senior author demonstrated that changes in the nasal parameters may be over or underestimated in the case of cephalically oriented lower lateral cartilages [8].
Applications of the M-Arch Model:
Once the nasal anatomy has been properly assessed, the M-Arch Model can be utilized to predictably effect changes in nasal tip projection, rotation, and nasal length. Additionally, lobular refinement, changes in the alar-columellar relationship, and alteration of the lobule-nasal base relationship can be performed.
Maintaining M-Arch Length:
When the length of the lower lateral cartilages is deemed to be appropriate, the M-Arch model can be employed to specifically address improving rotation, lobular definition, changes in the alar-columellar relationship, and/or alterations of the lobule-nasal base relationship. Specific maneuvers to address these parameters include tip suturing techniques, lobular scoring, or horizontal division of the arch in the cephalic region of the lateral crus.
When utilizing tip suturing in the context of the M-Arch Model, it is important to recognize the difference between open vs endonasal approach rhinoplasty. Although either method can be used with any of the described methods, one must consider that when performing either approach a variable amount of tip support is lost by the very nature of the approach, thus effecting minor deprojection in most cases. Thus, when solely performing some of the tip suturing methods described, the effect is simply lobular refinement without significant changes to tip projection, rotation, or length. The suture methods utilized while maintaining the length of the M-Arch which will improve definition of the lobule include the single dome unit, double dome unit, and intermediate crural sutures (Figure 7). In this video, increased lobular definition and narrowing of the columella is performed with a medial-intermediate crural suture (Video 1). Lobular scoring can also be performed in a cross-hatched fashion in conjunction with single dome or double dome unit sutures to allow for a natural break in the lobular region of the M-Arch for further tip definition (Video 2).
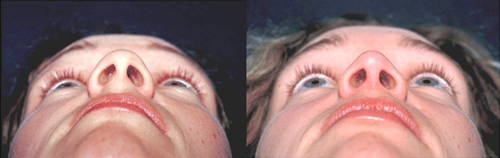
The young woman in Figure 8 complained of bulbosity and bifidity and of her nasal tip. She was a model and was quite tall, and therefore her tip projection, rotation, and nasal length were deemed to be within normal limits (Figure 8 A, C, E). She did demonstrate increased scatter of the nasal tip light reflex on frontal view. Her submental view demonstrated that her tip cartilages were indeed bifid, causing wideness of the columella and less than ideal lobule-nasal base ratio. Application of the M-Arch Model intraoperatively revealed symmetrical broad domal arches that were of appropriate length. Lobular refinement was achieved without affecting the remaining nasal parameters by performing single dome unit sutures, an intermediate crural suture, and conservative cephalic trim of the lateral crura (Figure 8G). A columellar strut was placed to maintain tip projection. Postoperative results show significant improvement in lobular definition without major changes in tip projection, rotation, or nasal length (Figure 8B, D, F).
Decreasing M-Arch Length:
The M-Arch length can be decreased to alter projection by performing a vertical division anywhere along the length of the arch and/or excising the arch at the foot of the medial or lateral crus. Simple excision at either of the feet of the crura would be performed without alteration of the intermediate crura in situations where lobular definition is satisfactory and requires no changes. More commonly, the tip is overprojected and asymmetrical, and the arch length may be decreased by performing a vertical lobule division (VLD) in the intermediate crural region, thereby correcting asymmetries and effecting deprojection with the same maneuver (Video 3). VLD can be performed near the angle of the medial and intermediate crura, thus effecting primarily vertical shortening and deprojection, or closer to the tip-defining point, effecting primarily shortening, narrowing, and refinement of the lobule (Figure 5). Although the vertical lobular division is the workhorse in our practice for decreasing the M-Arch length, shortening can be performed closer to the medial or lateral crural feet in order to effect tip deprojection as well. However, the anatomical configuration of the nasal tip cartilages are such that shortening in the regions of the lateral or medial crural feet, where a greater vertical component exists, will have greater effects on rotation and counter-rotation, respectively (Figure 5).
The woman in Figure 9 presented with complaints of her nose being too large and unrefined. Specifically she felt that her nose was overprojected and that her tip was amorphous. Lateral view demonstrated dorsal convexity, excessive tip projection and tip counter-rotation and subsequent increased nasal length. Frontal view demonstrated a bulbous nasal tip with significant scatter of light at the tip defining point. Submental view confirmed a bifid, bulbous nasal tip with a wide columellar base (Figure 9 A,C,E). Her skin was thick, and therefore more aggressive reductive maneuvers were planned to achieve the desired refinement of her lobule and supratip. Application of the M-Arch Model revealed a broad and elongated M-arch having excessive length primarily of the lateral crura. Shortened intermediate and medial crura contributed to her decreased lobule to columella ratio and gave the appearance of abnormal columellar height. Excessive breadth of the domal arches gave the appearance of tip bulbosity. (Figure 9E)
Several reductive tip maneuvers were employed to effect specific desired changes with her M-arch (Figure 9F). Vertical lobular division within the intermediate crura with 5 mm of overlap was employed to shorten the arch length, accomplishing preferential shortening of the intermediate crura in reference to the medial crura to restore a more natural lobule-to-columella ratio. This maneuver also produces excellent lobular refinement. The excessive lateral crural length, overprojection, and counterrotation were treated utilizing the most powerful rotator of the nose—the lateral crural overlay technique. Final tip refinement was accomplished with single dome unit sutures following scoring of the dome regions to create new tip-defining points bilaterally (Video 2). A columellar strut had been placed to maintain and strengthen the stability of the modified arch.
Increasing M-Arch Length:
When the tip defining point needs to be set forward in an underprojected nose, the M-Arch Model may be employed to produce this effect. The concept to be applied is that the short M-arch length needs to be lengthened, this performed selectively for the medial, intermediate, or lateral crura as deemed necessary to achieve ideal length, projection, rotation and lobule refinement. The specific techniques that can be used include placement of a columellar strut, suture techniques, lateral crural steal, vertical lobular division lateral to the tip defining point without re-suturing the arch (Goldman), and tip grafting. Apparent increases of the M-Arch can be performed by augmenting the nasolabial angle with cartilage or further lowering of the supratip region.
In our practice we almost always place a columellar strut to act as a lengthener and strengthener of the medial crura (Figure 10). Placement of the strut alone does not typically effect significant increased projection, although it will maintain projection and create a foundation for the base of the nose (Video 4). Suture techniques can be used alone to effect increased tip projection to a small degree—these include the previously discussed intermediate crural, single dome unit, and double dome unit sutures. In the endonasal approach, the septocolumellar suture, similar to the tongue-in-groove technique, can be an effective method to set the medial crural footplates forward on the septum and effect maintained or increased tip projection (Figure 11). The most powerful method to increase tip projection with simple suture techniques is to perform the lateral crural steal maneuver. In this maneuver, the vestibular skin is freed just as if a lateral crural overlay were being performed. The lateral crus is “stolen” and medialized, where a single dome unit suture is placed within the lateral crus to create the the new tip defining point (Figure 12, Video 5). Although used by fewer surgeons today, the Goldman maneuver is historically a well-utilized method to increase projection by performing vertical division of the arch lateral (cephalad) to the tip-defining point and medializing the lateral crural remnants. Caution must be exercised when performing this maneuver as it breaks the structural integrity of the arch and can lead to valve collapse or tip pinching.
When there is not enough cartilage in the M-Arch either due to congenital reasons or previous resection, tip grafting may be employed. Certain grafts can be used to increase the lengths of the intermediate and/or lateral crus. Specific grafts that may be used include a modification of Jack Sheen’s “shield graft” that we term the infratip lobule graft placed caudal to the tip defining point. It creates increased projection, length, counter-rotation and lobule definition. The cartilage augmentation projection (CAP) graft is placed cephalad to the tip defining point to create increased projection, apparent rotation of the infratip lobule, decreased length, and lobule definition (Figure 13). Both grafts can be placed together when needed. It is our recommendation these be sutured together to achieve maximal control of the newly created tip-defining point (Video 6). If, after all these maneuvers, further tip projection is desired, apparent increase of the M-Arch can be performed with nasolabial angle (NLA) grafting and/or supratip lowering. NLA grafting will provide apparent projection and rotation (pseudo-rotation). It is our preference to use cartilage in this region. Supratip lowering will also produce apparent increased projection and pseudo-rotation.
A young woman presented complaining of her nose being too small and unrefined. Frontal view demonstrated an amorphous, unrefined tip (Figure 14A). Lateral view revealed excessive dorsal convexity and tip rotation but less than ideal tip projection and length (Figure 14C). From the submental view it was apparent that her tip was bifid and trapezoidal in configuration (Figure 14E). Application of the M-Arch Model revealed that her overall arch length was deficient. Specifically, the intermediate and lateral crura were short. Therefore, a combination of lateral crural steal, infratip lobule and CAP grafts were employed to effect projection, counter-rotation, increased length and lobular refinement (Figure 14 G, Video 6). Horizontal excision of the cephalic margin of the lower lateral cartilages was performed to further produce lobular refinement, taking care to preserve 8 mm of lateral crura to prevent alar notching or collapse. Postoperative photographs demonstrate improved tip projection, counter-rotation, length and lobule refinement (Figure 14B, D, F).
Conclusions:
The M-Arch Model is an elaboration and extension of the tripod theory that can be employed to predictably effect changes in the three most important parameters of the nasal tip—tip projection, rotation, and nasal length. By using the M-Arch Model in the context of the bony and skin and soft tissue components of the nose, excellent aesthetic results can be produced without compromising nasal function. By being a lifelong student of rhinoplasty and always critically appraising one’s own results, the rhinoplasty surgeon can effectively utilize this model in the context of his or her own surgical skills to produce excellent results. An incremental employment of the maneuvers discussed is recommended in order to fully understand and appreciate their effect. We have found the M-Arch Model to be extraordinarily valuable in rhinoplasty planning and in achieving consistently satisfying results.
Figure 1. Tip defining point light reflex which is ideally 6-8 mm wide in the Caucasian female.
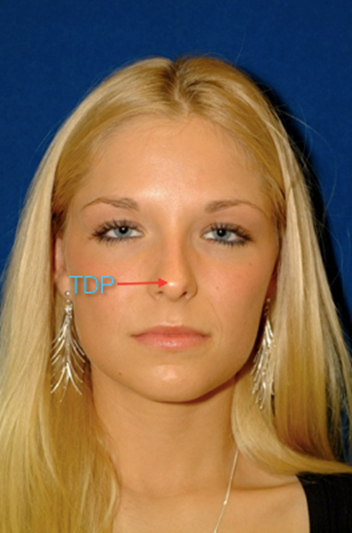
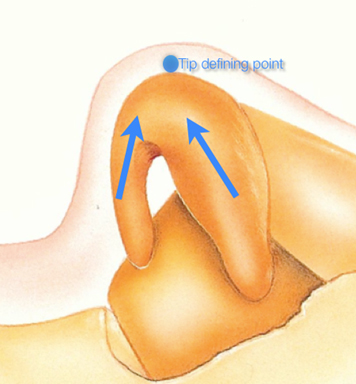
Figure 2. Dynamics of the M-Arch showing the thrusting forces (arrows) that define the dynamics of the lower lateral cartilages.
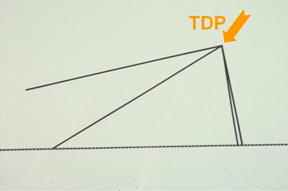
Figure 3. Tripod theory: the conjoined medial crura form one leg of the tripod while the lateral crura represent the other two legs of the tripod.
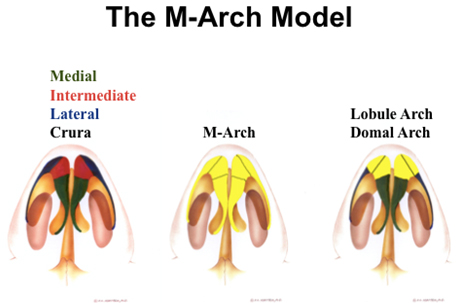
Figure 4. The M-Arch Model: The M-Arch is comprised of the medial, intermediate, and lateral crura. The lobular arch is an arch within an arch, representing the intermediate crura and the anterior most aspect of the lower lateral cartilages.

Figure 5. Vertical arch division (VAD): May be performed anywhere along the M-Arch. VAD can be performed near the angle of the medial and intermediate crura, thus effecting primarily vertical shortening and deprojection, or closer to the tip-defining point, effecting primarily shortening, narrowing, and refinement of the lobule. Division and overlap near the tip defining point will preferentially affect rotation, whereas division near the feet of the lateral and medial crura will preferentially affect projection.
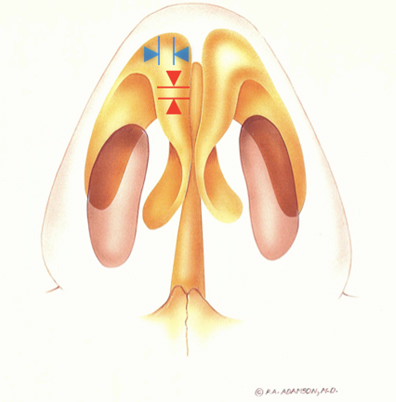
Figure 6. Anatomy of the M-Arch: Within the lobule, the greatest vertical components are near the crural feet (red arrows) while the greatest horizontal components are at the intermediate crura and anterior aspect of the lower lateral cartilages (blue arrows).
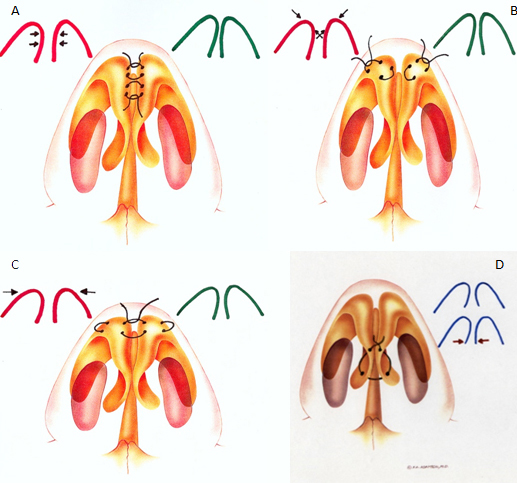
Figure 7. Tip suturing techniques: A.) Medial and Intermediate crural sutures B.) Single dome unit suture C.) Double dome unit suture D.) Medial crural transfixion suture
Figure 8. Maintaing the M-Arch. Photographs demonstrating pre (A, C, E) and 1 year postoperative (B, D, F) photographs of young woman requesting lobular refinement. Rhinoplasty diagrams (G) demonstrate conservative cephalic trim, placement of a columellar strut, and single dome unit sutures. Postoperative photographs demonstrate improved lobular refinement.
| A | B |
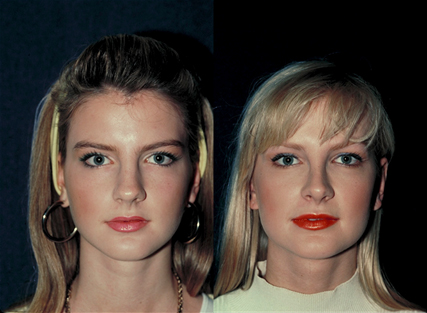
| C | D |

| E | F |

| G | H |
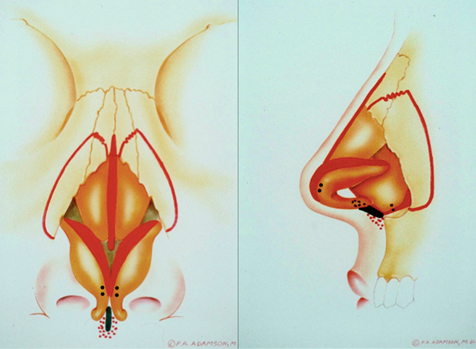
Figure 9. Decreasing the M-Arch. Photographs demonstrating pre (A, C, E) and 1 year postoperative (B, D, F) of a young woman complaining of her nose being too large and her tip too unrefined. Rhinoplasty diagram (G) demonstrates vertical lobular division, lateral crural overlay, lobular scoring, columellar stut, and single dome unit sutures. Postoperative photographs demonstrate improved lobular refinement, tip deprojection and increased tip rotation.
| A | B |

| C | D |

| E | F |

| G | H |
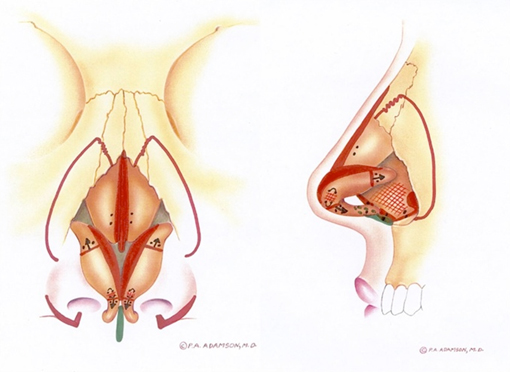
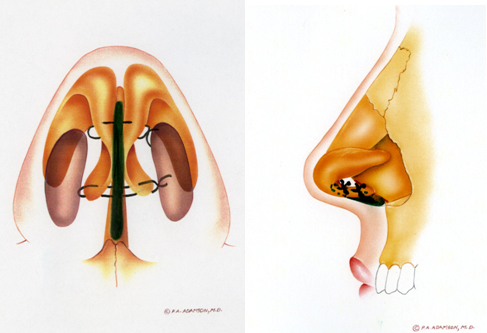
Figure 10. Columellar strut: Lengthener and strengthener of nasal tip.
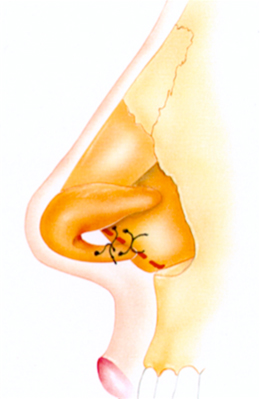
Figure 11. Septocolumellar suture (Tongue-In-Groove). Utilized to set tip defining point manually by suturing medial crura to desired location on caudal septum.
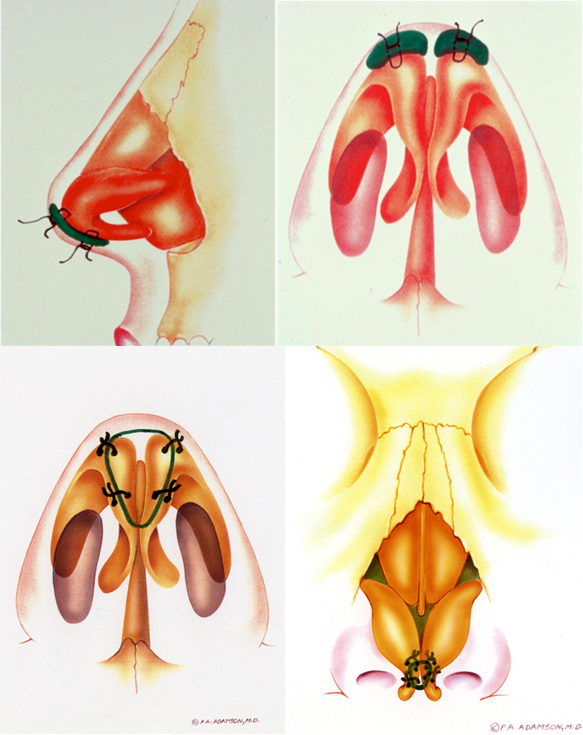
Figure 12. Tip grafting. A.) Infratip lobule graft will effect projection, counterrotation, and lobule refinement. B.) Cartilage augmentation projection (CAP) graft will yield projection, rotation, and lobule refinement.
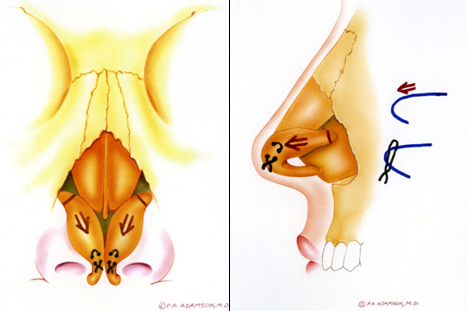
Figure 13. Lateral crural steal: A. The lateral crura is freed from the underlying vestibular skin, detached at the hinge region, and advanced forward. B. A single dome unit suture is placed, effecting medialization of the lateral crura into the intermediate crura, producing increased projection.
Figure 14. Increasing the M-Arch. Photographs demonstrating pre (A, C, E) and 1 year postoperative (B, D, F) of a young woman complaining of her nose being too short and her tip too unrefined. Rhinoplasty diagrams (G) demonstrate columellar strut, lateral crural steal, and placement of a cartilage augmentation projection (CAP) graft and infratip lobule graft. Postoperative photographs (B, D, F) demonstrate improved projection, tip counterrotation, and lobular refinement.
| A | B |

| C | D |

| E | F |
| G | H |
Videos:
References:
- Fomon S. Cosmetic surgery—Principles and Practice. Philadelphia: Lippincott, 1960.
- Anderson JR. The dynamics of rhinoplasty. In: Bustamant GA, ed. Proceedings of the Ninth International Congress of Otorhinolaryngology, Mexico City, August 10-14, 1969. Amsterdam, the Netherlands: Exceprta Medica; 1970
- Adamson PA, Litner JA, Dahiya R. The M-Arch model: a new concept of nasal tip dynamics. Arch Facial Plast Surg2006;8:16–25
- Adamson PA, Litner JA. Applications of the M-Arch Model in nasal tip refinement.
Facial Plast Surg 2006;22(1):42-48 - Adamson PA, Funk E. Nasal tip dynamics. Facial Plast Surg Clin N Am 2009;17(1):29-40
- Papel ID et al. Facial Plastic and Reconstructive Surgery. Third ed. New York, NY: Thieme; 2009.
- Sepehr A, Chauhan N, Alexander AJ, Adamson PA. Evolution in nasal tip contouring techniques: a 10-year evaluation and analysis. Submitted to Arch of Facial Plast.
- Sepehr A, Alexander AJ, Chauhan N, Chan H, Adamson PA. Cephalic positioning of the lateral crura : implications for nasal tip-plasty. Arch Facial Plast Surg 2010;12(6)379-84.
