Abstract
Many skilled surgeons are hesitant to apply the Goldman technique to their patients in fear of the consequences on the external nasal valve and overall to the nasal patency due to the fact, that it is an irreversible technique. In this study we prove that these fears are unjustified because both the aesthetic and the functional nasal measurements 10 years postoperatively are satisfying and within the normal limits.
Introduction
One of the most challenging tasks in modern day rhinoplasty is the achievement of an aesthetic and functional nasal tip. Many techniques have been proposed throughout the years for the reconstruction of the nasal tip and most of them concentrate on multiple-suture methods1,2 and the placement of grafts3 and their results in most cases of overprojected or boxy tips have been remarkable. But if these methods prove to be inadequate what is the next step for an experienced rhinoplasty surgeon that wishes to deliver a functional and aesthetically pleasing result?
In 1957 the Goldman technique was first introduced in the rhinoplasty world by the homonymous surgeon Irving B. Goldman4. In his paper “The importance of the mesial crura in nasal tip reconstruction” Goldman first described the vertical division of the domes of the alar cartilages and the creation of two independent flaps the lateral and the medial crura. By the elaborate trimming of these flaps both at the scroll area and at the dome region, the reconstruction of the height, shape and the rotation of the nasal tip is achieved.
Nowadays it has been observed that the majority of the rhinoplasty surgeons resort to mοre conservative methods for the improvement of tip abnormalities and have set aside more aggressive techniques like the “Goldman technique” fearing unpredictable post-operative results both at the shape of the nasal tip (notching, pinching of the tip, bossae and tip asymmetries) and at its function (external nasal valve)5. The Goldman technique is executed via the endonasal approach as it is originally described. Therefore all major tip support mechanisms are disturbed. Adherents to this method argue that by transecting the domes, the continuity of the lower lateral cartilages is disrupted and the lateral nasal wall is more susceptible to collapse6 (destruction of the external nasal valve).
Throughout this report and with the disclosure of the surgical outcomes and the functional measurements of a large series of patients who had undergone surgery with the Goldman technique by our senior author Athanasios Skouras, we will try to eradicate any misconceptions regarding the Goldman technique and prove that in the hands of a skilled and experienced surgeon who has the fully understanding and respect of the basic principles that concern the nasal tip, the Goldman technique is a powerful tool for severe tip abnormalities (such as drooping tip, broad nose, overprojected or underprojected tip) without compromising the integrity and the function of the external and internal nasal valve as it is feared by many rhinoplasty surgeons. With our research we aimed to prove that by using the Goldman technique, the functional outcome of the nose not only isn’t violated, but on the contrary it is improved, and the same applies to the aesthetic result. The fact that since its first introduction in the 1957 is still performed invariably, shows that it is a timeless method.
Materials and methods
The study included 89 patients (32 males and 57 females) that underwent functional septorhinoplasty using the Goldman technique between 2007-2009 by our senior author. For each patient we were provided from our senior authors’s database pathological clinical findings, operative techniques, pre and post operative photos and complications. This study included only the patients that underwent primary rhinoplasty and the Goldman technique was performed and not revision cases.
This study has one of the longest follow up periods ever presented in an article, given the case that it includes patients with a 10-12 year long postoperative follow up period.
All patients were re-examined after 1,3 and 10 years postoperatively in order to estimate both the aesthetic outcome and the nasal patency in the long term.
Operative technique
At all the patients the closed approach was used.
With this approach, the lower nasal cartilages are delivered with the marginal and transfixion incision. The cephalic part of the lower cartilages is released with the intercartilaginous incision. After their delivery, the width of the lateral crura is reduced cephalically until the remaining crura is at least 5-8 mm. Then, after marking the apex of the dome, the lower lateral cartilage is divided vertically, 1.5 mm laterally to the apex of the dome, creating two independent flaps, the lateral and the medial. The dissection includes the underlying skin. In cases of an overprojected tip, the height of the central cartilage-cutaneous flap (consisting of the medial crura with the overlying skin) is reduced and the nasal tip is deprojected. After the dissection of the alar cartilages the lateral crura should be trimmed in order to avoid overlapping with the new dome and ensure that it lines up in continuance with the edge of the new dome cartilage. Then the two media crura are sutured together with absorbable PDS 5-0 sutures. The sutures are placed in three key points during the joint of the medial flaps: one at the base of flap in order to provide stability, one in the middle and the last one and most crucial one is placed 2-3 mm below the apex to simulate the natural curvature of the two domes and to avoid the formation of an unnatural pinched or thin tip.
When the tip support is weak, usually in noses with a short or deviated septum or with medial crura that are short or curved and footplates that do not reach down to the nasal spine, a columellar strut is placed between the medial crura.
When the surgeon estimates intraoperatively, that the intrinsic strength of the lateral crus is weak, he sutures a straight cartilaginous graft (ideally septal) onto the lateral segment of the lateral crus reaching the hinge area, to avoid postoperative collapse and functional compromise.
The lateral flaps are sutured in place with the overlying skin (closure of the marginal incision) using Vicryl 6-0 absorbable sutures both to ensure their approximation to the medial flaps and to avoid their displacement or malposition.
Aesthetic outcome
The pre- and postoperative photos were evaluated by an independent observer using the following five parameters:
1. Satisfactory tip projection
2. Tip shape (triangular vs. trapezoid)
3. Tip symmetry
4. Appropriate tip rotation
5. Presence and distance of tip defining points
Tip projection was evaluated using the Goode ratio and tip rotation with measurement of the nasolabial angle (950–1000 for females and 900–950 for males). The distance between the tip-defining points was considered improved when it had decreased by at least 2 mm postoperatively. For each patient, a score of -1, 0, or 1 was given for each of the five parameters depending on whether they had deteriorated, stayed the same, or improved respectively with the Goldman technique. The maximum score for each patient was 5, which showed postoperative improvement in all five categories, and the minimum score was -5.
The evaluation of the aesthetic outcome was based on the same parameters and methods that were used on our previous paper concerning the Goldman technique25.
Functional outcome
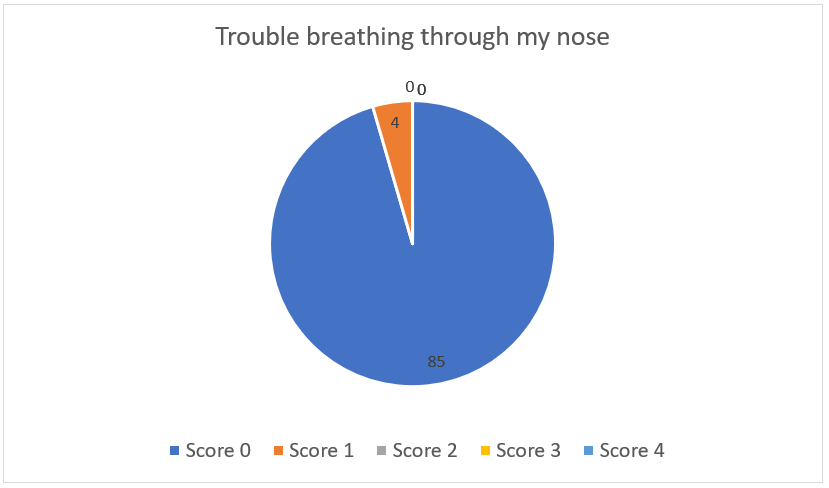
Patients were evaluated for subjective symptoms with the validated NOSE scale and objective measurements with a PNIF – instrument (a portable hand – held inspiratory flow meter).
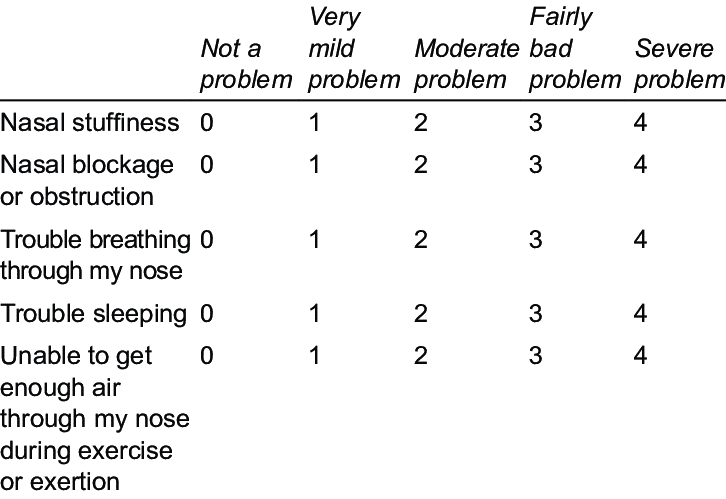
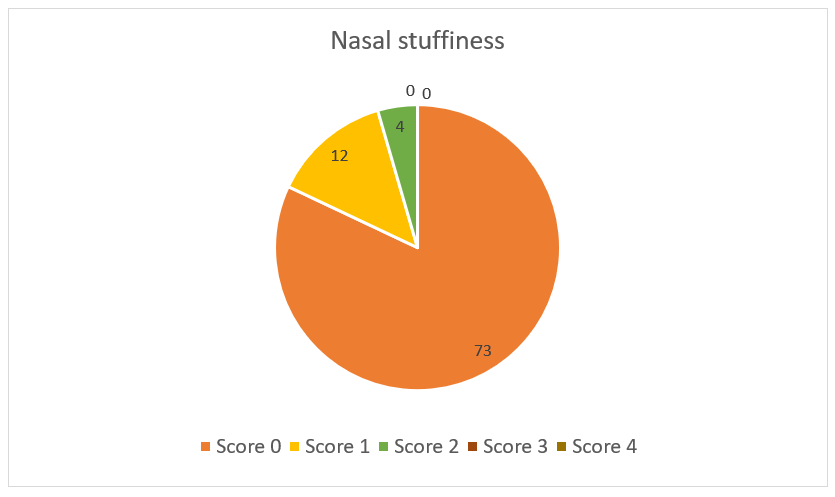
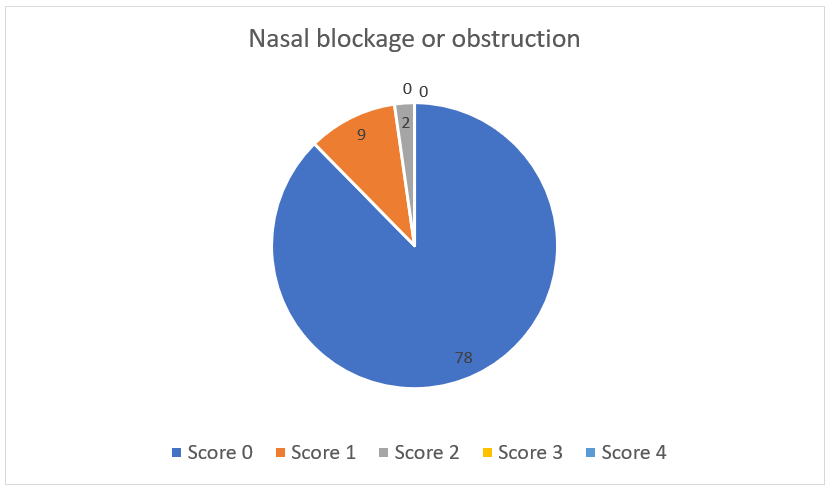
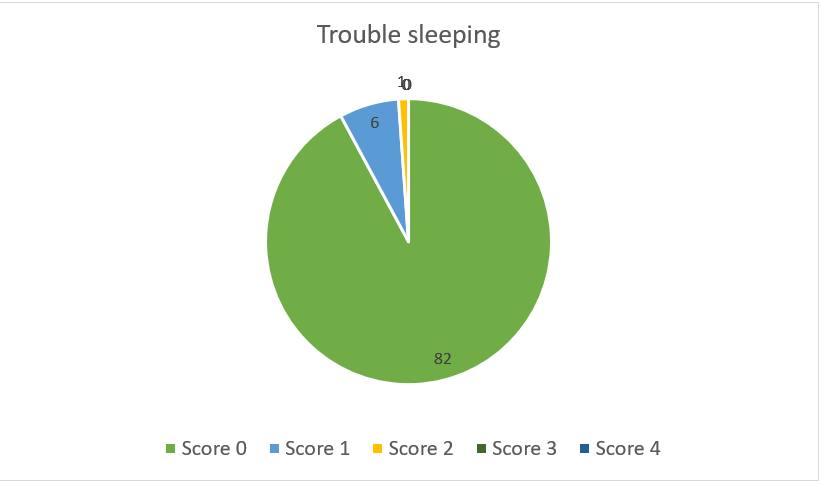
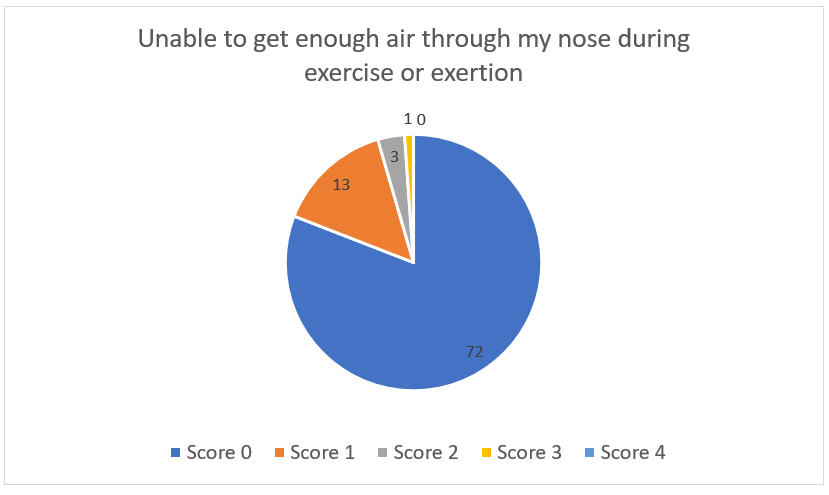
The NOSE scale is a subjective quality of life instrument specific to nasal obstruction. It asks the patients to rate on a 0-4 scale, over the past month their feelings on five separate questions, such as nasal blockage, trouble sleeping, ability to get enough air through the nose during exercise (fig.1). The answers are summed up and the total score is multiplied by 5 for a maximum score of 100 (0: asymptomatic, 100: total nasal blockage)7. The NOSE scale is a patient-centered questionnaire capable of evaluating nasal obstruction following rhinoplasty8.
The PNIF instrument (fig.2) was presented by Youlten in 1980. It is an inexpensive, fast, portable and simple technique. It is reproducible and as good an indication of objective nasal patency as formal rhinometry. It measures the peak nasal inspiratory flow of the patient during a hard and fast inhalation through the face mask, keeping the mouth closed, starting from the end of a full expiration. The patient must be standing because PNIF measures are higher when standing than sitting. Three PNIF measurements are performed and the best is used for the evaluation. PNIF has been recommended by many authors as a valuable objective instrument for the evaluation of subjective nasal obstruction9.

PNIF measurements are significantly correlated and associated with the NOSE scale and they are recommended for the evaluation of nasal patency in patients that experience alar collapse during forced inspiration10.
Results
For the purposes of this paper, patients that underwent surgery during 2007-2009 and the Goldman method was used on them, were selected. They were evaluated throughout the decade at three crucial points: one year post-op, three years and finally 10 years after their surgery had occurred. During the one and three years follow up period both the aesthetic and functional outcome were evaluated through the subjective methods described previously but at the ten year post-op period the PNIF instrument was introduced providing us with an objective measurement method.
From our database 89 patients that the Goldman technique was performed on them were reviewed. The patients individual features are shown in Table 1. A total of 51 cases (57.3%) involved noses that suffered from an overprojected tip, whereas 38 cases (42.7%) had a bulbous tip.
As mentioned before all of our cases were primary rhinoplasty. From the total of the 89 patients, 57 (64%) were female and 32(36%) patients were males within a mean age of 38 (20-57).
During our follow-up period and at the tree years landmark complications were observed at six (6.7%) patients (Table 2). Alar collapse was considered the result of an excessive cephalic reduction od the lateral crura. Tip underprojection resulted from the larger than needed reduction of the height of the media crura and finally, the pinched tip occurred in a woman with a very thin skin. All six patients underwent reoperation with successful results.
In detail, the patient that presented the pinching of the tip underwent surgery and an onlay grafted and diced cartilage was placed. Diced cartilage can serve as a camouflage for noses with very thin skin and can be used in general to patients with thin skin that the Goldman technique is needed. It is important to note that to prevent the pinching of the tip, the lateral crus after its height reduction must line up with the edge of the new dome cartilage.
Furthermore, in the two cases that had deprojection of the tip due to excessive reduction of the media crura, a collumlellar strut between the media crura as well as diced cartilage that was harvested from the ear above the two domes was the senior’s author solution and it provided the patients with an increased tip projection.
Finally, for the three cases that presented with alar collapse and external valve insufficiency, the senior author chose the placement of a lateral crura cartilage strut graft harvested from the auricle to correct this complication. This deformity occurred due to excessive cephalic trimming of the lateral crura and we believe that it can be prevented if the rhinoplasty surgeon is more conservative.
As mentioned before, the pre- and postoperative photos were evaluated by an independent observer using the five parameters presented in Table 3. The mean evaluation score for these five parameters according to the scale of -5 to +5 shows a significant postoperative improvement.
For the functional outcome, the subjective symptoms of the patients were evaluated with the NOSE scale and the results are presented for each parameter with the corresponding pie chart. For the NOSE evaluation scale, we lack the pre-operative measurements but we believed that the post-operative results are satisfying and show that our patients did not experience deterioration concerning the nasal obstruction.
Ultimately, in Table 4 the PNIF values are presented. All of our patients during the 10 years evaluation had PNIF measurements above average. For the female patients the measurements were fluctuated from 80L/min to 130L/min. for the male patients of our study the lowest PNIF outcome was 100L/min and the highest 140 L/min, proving that throughout the years when the Goldman method is performed after careful consideration and not too aggressively, little impact has on the nasal patency. The three patients that during the three years follow up period experienced functional compromise due to alar collapse and underwent revision rhinoplasty, were females and the PNIF measurements ranged from 80-95 L/min.
Finally, in figures 3-7 we present the answers of our patients to the Nose scale questionnaire.
Additionally, it is remarkable to mention that from these cases with the satisfying PNIF score, three patients had been suffering from Chronic Obstructive Pneumopathy and despite that their results were within normal range.
| Table 1 Characteristics of patients treated with the Goldman technique | |
| Characteristics | Value (n%) |
| Age: years (range) | 38 (20-57) |
| Sex: | |
| Male | 32 (36%) |
| Female | 57 (64%) |
| Primary rhinoplasty | 89 |
| Underlying tip deformity: | |
| Overprojected tip | 51 (57,3) |
| Bulbous tip | 38 (42.7) |
| Table 2 Compications observed in patients treated with the Goldman technique | |
| Complication | No. of patients |
| Alar collapse | 3 |
| Tip underprojection | 2 |
| Pinching of the tip | 1 |
| Table 3 Mean evaluation score for the parameters studied in rhinoplasties | |
| Parameter | Mean evaluation score (scores ranged from -1 to +1) |
| Tip projection | 0.96 |
| Tip shape | 0.82 |
| Tip symmetry | 0.92 |
| Tip rotation | 0.79 |
| Presence and distance of tip defining points | 0.72 |
| Table 4 Mean PNIF values obtained | |
| Sex: | Score (L/min) |
| Males | 125 (100-140 L/min) |
| Females | 102 (80-130 L/min) |
Discussion
With the publication of his paper Irving Goldman provided the world of rhinoplasty a powerful tool that could help any experienced rhinoplasty surgeon transform the nasal tip. Tip abnormalities are considered the greatest challenge a rhinoplasty surgeon has to face in the careful modification of the nasal tip without disturbing the structure of the nose or its function (external valve) and they have to be performed only by skillful and experienced rhinoplasty surgeons that respect its delicate balance.
The purpose of this report is to demonstrate through our results, both for the aesthetical and functional outcome of the nose, that the Goldman technique despite the general belief does nothing to deteriorate the functional capacity of the nose or its appearance. With our previous report25 we have already proven the long-term aesthetic efficacy of this method. With this report we aimed at proving the aesthetic stability in an even longer postoperative period and combine it with results from the functional examination of the nose during the same period.
The Goldman tip procedure is performed via an endonasal cartilage delivery approach and on his first article Irvin Goldman emphasizes the importance of the media crura in tip repair. Nevertheless, the procedure can be performed and through the external approach but all the cases that this paper is referring to, were conducted with the endonasal approach by our senior author A. Skouras. Before our senior author came to the decision of applying the method to each patient, he took each case carefully under consideration. The division of the alar cartilages was performed when all the other suturing techniques did not provide a both pleasing aesthetically and functional result. Tip asymmetry, overprojection or underprojection, the bulbous tip, rotation deformities od the tip and the heavy skin are crucial indications for the experienced rhinoplasty surgeon to apply the Goldman technique. Furthermore, it is mentioned by Simons and coworkers14 that the aging nose that leads to a ptotic tip due the lack of skin tightness, bone resorption or the disassociation of the upper and lower cartilages, can benefit from this method. Also, Friedman et al15 found this technique extremely helpful in revision cases with the asymmetries or overprojection of the nasal tip.
In conclusion when major changes to the projection, direction and the overall shape of the tip are proven to be inevitable the vertical dome division is required a philosophy that conforms to the thought of Toriumi and Tardy16 :”If cartilage suturing techniques prove to be inadequate, then more aggressive techniques such as dome division can be used.”
Ironically the “golden” method that is used to improve severe tip abnormalities is also accused of causing them. The complications associated with the technique are underprojection, bossae, tip asymmetries, alar retraction and valve collapse. These negative post-operative results may occur in the cases that excessive cartilage excision was performed. After the delivery of the lower cartilages, their cephalic trimming and the division of the domes the lateral crura that remains should be at least 5-8mm. Our senior author rarely reduces their width under 8mm which allows the nasal tip to maintain its structure in combination with a firm media crura.
Throughout the years of performing the Goldman technique, it has proven to be a reliable option in the correction of severe tip abnormalities without compromising the functional capacity of the nose.
Many rhinoplastic surgeons refrain from performing the Goldman technique fearing that the loss of continuity of the lower cartilages might lead to the destruction of the external nasal valve. Therefore, the purpose of this study is to prove that the Goldman technique when performed properly, does not compromise the patency of the external nasal valve in the long term and does not lead to nasal obstruction.
The estimation of PNIF gives a direct measure of nasal obstruction17. In adults, PNIF is higher in males than females and values increase with height and decrease with age as it is shown in many studies9,11-13. (Table 5)
| Table 5 Mean PNIF values obtained by different studies in adult population | ||
| Mean PNIF (L/min) in males | Mean PNIF (L/min) in females | |
| Ottaviano et al. (2006)9 | 143 +/- 48.6 | 121.9 +/- 36 |
| Blomgren et al. (2003) 11 | 145 | 128 |
| Bouzgarou et al. (2011) 12 | 174 +/- 54 | 126 +/- 33 |
| Klossek et al. (2009) 13 | 104.6 +/- 54.8 | 80.8 +/- 33.4 |
PNIF, peak nasal inspiratory flow
PNIF is used to estimate nasal valve collapse18-22 and the outcome of nasal surgery24. Many authors suggest its use as a valuable objective instrument for the evaluation of subjective nasal obstruction23.
The NOSE scale is a patient reported outcome measure (PROM). It is the most widely used and accepted PROM and helps surgeons to assess nasal obstruction in rhinoplasty 8.
In our study we used the correlation of NOSE scale and PNIF for the estimation of the nasal patency. Menger et al in their study10 «surgery of the external nasal valve: the correlation between subjective and objective measurements» reported that since PNIF was significantly correlated and associated with the NOSE-scale, this objective test is recommended for the evaluation of nasal patency in patients that experience alar collapse during forced inspiration.
Unfortunately, during our first interaction with our patients during 2007-2009 we had not introduced in our pre-operational check the NOSE and PNIF measurements thus depriving us the opportunity to compare pre- and post-operative results. But with the elaborate examinations of the post-operative results we have come to a safe conclusion that the Goldman technique doesn’t deteriorate the nasal patency. All of our patients in our ten years post-operative examination through both objective and subjective measurements proved that their nasal breathing was sufficient. Even in our revision cases that the alar collapse occurred, the patients 7 years later provided us with exceptional results both aesthetically and functionally.
The Goldman technique should not be feared by an experienced rhinoplasty surgeon. After careful consideration and examination of each case every surgeon can perform it as long as he respects the nasal anatomy and delicacy of the nose.
Conclusion
Throughout this paper and our experience through our interaction with our patients in the long term we have come to the conclusion that the Goldman technique is a safe method to apply in major tip deformities and does not compromise the aesthetic or the functional outcome when performed with prudence.
To the best of our knowledge our paper is the only one that has such a long term follow-up period and proves through our results the functional and aesthetic efficacy of the Goldman technique.



Pre-operative photo 2008



Post-operative photo 2020



Pre-operative photo 2008



Post-operative photo 2020
References
- Behmand RA, Ghavami A, Guyron B (2003) Nasal tip sutures part I: the evolution. Plast Reconstr Surg 112:1125
- Guyron B, Behmand RA (2003) Nasal tip sutures part II: the interplays. Plast Reconstr Surg 112:1130
- Leach JL, Athre RS (2006) Four-suture-tip rhinoplasty: a powerful tool for controlling tip dynamics. Otolaryngol Head Neck Surg 135:227–233
- Goldman IB (1957) The importance of the mesial crura in nasal tip reconstruction. Arch Otolaryngol 65:143–147
- Tebbets JB (1999) Rethinking the logic and techniques of primary tip rhinoplasty. Otolaryngol Clin N Am 32:741–754
- Vertical Dome Division Rhinoplastyhttps://emedicine.medscape.com/article/841313-overview#a12
- Stewart MG, et al (2004) Development and validation of the Nose Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg 130:157-163
- Okland, T.S., Kandathil, C., Sanan, A. et al. (2020) Analysis of Nasal Obstruction Patterns Following Reductive Rhinoplasty. Aesth Plast Surg 44: 122. https://doi.org/10.1007/s00266-019-01484-5
- Ottaviano G, Fokkens WJ (2016) Measurements of nasal airflow and patency: a critical review with emphasis on the use of peak nasal inspiratory flow in daily practice. Allergy 71: 162-174
- Menger DJ, Swart KMA, Trenite Nolst GJ (2014) Surgery of the external nasal valve: the correlation between subjective and objective measurements. Clin. Otolaryngol. 39, 150– 155
- Blomgren K, Simola M, Hytonen M, Pitkaranta A. Peak nasal inspiratory and expiratory flow measurements–practical tools in primary care? Rhinology 2003;41:206–210.
- Bouzgarou MD, Ben Saad H, Chouchane A, Cheikh IB, Zbidi A, Dessanges JF et al. North African reference equation for peak nasal inspiratory flow. J Laryngol Otol 2011;125:595–602.
- Klossek JM, Lebreton JP, Delagranda A, Dufour X. PNIF measurement in a healthy French population. A prospective study about 234 patients. Rhinology 2009;47:389–392.
- Davis AM, Simonas RL, Rhee JS (2004) Evaluation of the Goldman tip rocedure in modern-day rhinoplasty. Arch Facial Plast Surg 6:301-307
- Friedman WH, Rosenblum BN, Krebs FJ (1987) The Goldman tip in secondary rhinoplasty. Plast Reconstr Surg 79:339-343
- Toriumi DM, Tardy ME (1995) Cartilage suturing techniques for correction of nasal tip deformities. Ope Tech Otoryngol Head Nech Surg 6:265-273
- Clarke RW, Jones AS, Richardson H. Peak nasal inspiratory flow–the plateau effect. J Laryngol Otol 1995;109:399–402
- Larsen K, Oxhøj H, Grøntved A, Kristensen S. Peak flow nasal patency indices in patients operated for nasal obstruction. Eur Arch Otorhinolaryngol 1990;248:21–24.
- Holmstrom M, Scadding GK, Lund VJ, Darby YC. Assessment of nasal obstruction. A comparison between rhinomanometry and nasal inspiratory peak flow. Rhinology 1990;28:191–196.
- Barnes ML, Lipworth BJ. Removing nasal valve obstruction in peak nasal inspiratory flow measurement. Ann Allergy Asthma Immunol 2007;99:59–60.
- Poirrier AL, Ahluwalia S, Kwame I, Chau H, Bentley M, Andrews P. External nasal valve collapse: validation of novel outcome measurement tool. Rhinology 2014;52:127–132
- Hellings PW, Nolst Trenite GJ. Improvement of nasal breathing and patient satisfaction by the endonasal dilator Airmax (R). Rhinology 2014;52:31–34.
- Kjaergaard T, Cvancarova M, Steinsvag SK. Does nasal obstruction mean that the nose is obstructed? Laryngoscope 2008;118:1476–1481.
- Balikci HH, Gurdal MM. Use of peak nasal inspiratory flowmetry and nasal decongestant to evaluate outcome of septoplasty with radiofrequency coblation of the inferior turbinate. Rhinology 2014;52:112–115.
- Skouras A, Asimakopoulou F-A, Skouras G, Divritsioti M, Dimitriadi K. Use of the Goldman Technique to Correct Both the Overprojected and the Broad Nasal Tip. Springer Science+Business Media, LLC and International Society of Aesthetic Plastic Surgery 2011.
