Introduction
Nasal tip refinement techniques have continued to evolve over recent decades.1 Reshaping of the tip of the nose must be carefully and precisely performed, as there are numerous aesthetic and functional implications. In this article, we focus on a transformative nasal tip technique called the Cranial Tip Suture, originally described in a 210 patient series by Drs. Kovacevic and Wurm in 20142.
Traditionally, the simplest approach to refinement of the nasal tip was the cephalic trim, an excision of the cephalic margin of the lateral crus. Often performed endonasally, this eliminated some of the bulk along the cephalic edge of the tip and helped refine the supratip. Over-aggressive cephalic resection can result in pinching of the sides of the tip and external valve stenosis, creating an unfavorable transition from the tip to the alar subunits of the nose. Numerous suture techniques such as intradomal, transdomal, hemidomal, and oblique domal sutures have been developed to allow for further tip refinement and reshaping without excessive cartilage removal.
The intradomal suture prevents splaying of the domal tips and results in improved lower lateral cartilage (LLC) symmetry3. It is particularly useful in weak domal cartilages and can be performed via endonasal or open approach. A suture is placed between the medial third of the LLC, just posterior to the junction of the intermediate and lateral crura along their cephalic borders (~3-4 mm)4. A challenge with this technique is placement at equal points on each dome to enable transverse alignment of the cartilages, and not overtightening the suture to avoid excessively narrowing the tip.
The transdomal suture is a horizontal mattress centered on the width of the LLC at nasal tip and results in narrowing of the dome, as well as defining the axes of the nasal tip in the cranial and caudal plane3. It converts the broad, obtuse angle of the LLC at the tip to a narrowed, sharp angle of about 60-90º. The limitation of this traditional transdomal suture is that both the caudal and cephalic portions of the dome are narrowed to roughly the same extent. This can create an unfavorable shadowing lateral to the dome along the cephalic margin of the lateral crus. Or if the transdomal suture is not tightened enough, the degree of cephalic definition and flattening are limited. The transdomal suture alone does not provide the ideal longitudinal rotation effect of the lateral crus.
A modification of this is the oblique domal suture, which involves angling the horizontal mattress along the access of the LLC to increase eversion in the axial plane1. This provides a better rotational effect on the lateral crus, bringing the cephalic margin down and the caudal margin up, maintaining a strong alar rim contour. However, the oblique domal suture may not recruit the lateral crus as far laterally, limiting the tensioning and flattening effects which would be desired. Additional maneuvers such as lateral crural strut grafts may be needed for lateral crural flattening and strengthening in these cases.
Another take on nasal tip contouring, similar to the transdomal suture, is the hemidomal suture5. With this method, a simple interrupted suture is placed ~2-3 mm posterior to tip, along the cephalic end of the dome. The result is approximation the cephalic edges of the medial and lateral crura, flattening of the LLC in the axial plane. This avoids excessive narrowing of the domes and prevents any resulting concavity or inversion of the alar rims that can be seen with the transdomal technique.
An additional method that narrows the domal arch and corrects tip asymmetry is vertical domal division6. It can particularly useful in primary or revision rhinoplasty cases in which there is significant LLC/dome asymmetry. However, it is avoided by some surgeons due to the difficulty in recreating a natural appearing dome and soft triangle facet. Some surgeons have utilized an extended shield graft in front of the divided domes to redefine the tip defining points. There may also be a negative impact on nasal airflow. An airflow study with this method found diminished flow in about 10% of patients following vertical dome division, but no subjective correlation was identified7. It can be modified with a partial division of the dome, which may achieve similar results, while avoiding nasal valve weakening and airflow impairment8.
Below, we describe the cranial tip suture (CTS) technique of Kovacevic, et al.2 We will review its benefits, including predictable and consistent tip refinement, external valve stabilization, and ease of placement. The characteristics of the ideal nasal tip will be discussed. Associated tip maneuvers are also reviewed to optimize the tip refinement and stability attained with CTS placement.
Characteristics of the Ideal Nasal Tip
Before considering the techniques needed to achieve the ideal tip aesthetic, it is helpful to define exactly what we are trying to achieve. The ideal nasal tip should be symmetrical, with domes at the same height and anterior-posterior position. The cephalic margins of the lateral crura should be symmetrical and relatively flat, without significant fullness. The alar rims ideally become strong and flat, without depressions lateral to the domes. This look can occur with traditional tip defining techniques that isolate the tip as a separate unit from the alar units with a deepening or caudal extension of the alar creases. Patients often describe this look as a tip which appears “ball-like.” The soft triangle facets should be soft, symmetrical, and subtle. Slight infratip rotation with a double break of the columella can be an attractive feature. Many patients prefer a slight supratip break as well.
Surgical Technique
In a typical open rhinoplasty, a “top down” approach is utilized by the senior surgeon (UM). To approach the septum, the lower lateral cartilages are separated after elevation of the skin and soft tissue envelope. Following the bony and cartilaginous profile reduction and osteotomies, the septoplasty and spreader graft placement are performed. In nearly all open rhinoplasties, a caudal septal extension graft (typically side-to-side) is placed, securing it to both the caudal septum and spreader graft with PDS sutures. The tip position is stabilized by attaching the medial crura to the caudal septal extension graft with a tongue-in-groove (septocolumellar) 5-0 Prolene or 5-0 PDS suture. The cephalic trims are then performed, reducing lateral crural width to between 8 and 10 mm. After establishment of tip support/position as well as the lateral crural width, the cranial tip sutures are placed.
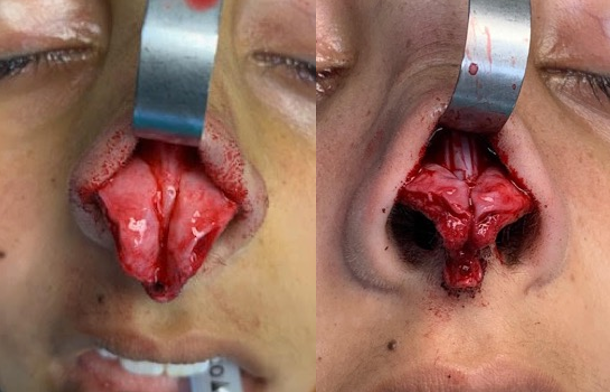
The cranial tip suture technique is essentially a variation of the traditional domal suture. The primary difference is that the bites through the medial portions of the intermediate crura are performed as a horizontal mattress whereas the lateral crural bites are in a vertical mattress, oriented just along the cephalic margin. A 5-0 Prolene suture on a P-3 needle is recommended for cranial tip sutures.
The initial step of the cranial tip suture technique is to free the vestibular skin for a few mm in each direction from the undersurface of the domes. This allows for a pocket beneath the domes for the permanent sutures to sit, preventing them from passing through the vestibular skin into intranasal positions. One jaw of a smooth Adson forceps is then passed through the tunnel under the dome and the second jaw passes above the dome. This allows the surgeon to establish the dome location precisely and symmetrically in each LLC. This can be very useful in cases of dome asymmetry, whether postsurgical or congenital.
The first bite of the cranial tip suture is made just posterior to the anterior edge of the medial portion of the intermediate crus. This entry point is approximately 3 mm inferior to the dome. The needle then passes superolaterally towards the lateral portion of the intermediate crus. The exit point is approximately 3 mm lateral to the dome, ~1 mm from the cephalic margin. The second entry point is 3-4 mm lateral to this point, passing again 1 mm from the cephalic margin of the LLC. This needle pass then exits inferior to the dome again, this time posterior to the initial entry point. Six or seven knots are tightly thrown to ensure that the Prolene suture does not become untied. The identical four-point technique is then performed on the opposite LLC, taking care to pass above and below the dome at symmetrical points.
Figure 1: Cranial tip suture entry and exit point locations (additional credit: Jeff Sharon)
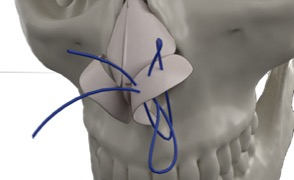
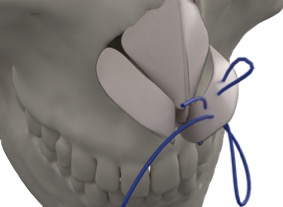
Figure 1: Cranial tip suture entry and exit point locations (additional credit: Jeff Sharon)
Video 1: Cranial Tip Suture Placement
Associated Tip Techniques
After placement of the two cranial tip sutures, the domes must be brought together at the same height. A 5-0 PDS horizontal mattress suture is placed through the infradomal segment of each intermediate crus, above and below the lower bites of the CTS. This helps to establish tip support and projection, unifying the tip. The 5-0 Prolene sutures between the domes serve as spacers, keeping the domes slightly apart to avoid a uni-tip.
If the reapproximation of the lower lateral cartilages results in domes which have too much of a vertical (cephalad-caudal) component, the domes can be trimmed along their cephalic edge. The domes should be roughly 6-7 mm in this dimension to create a natural and refined tip shape on profile view. Shaving one or both domes can also create better symmetry if one dome is slightly leading in front of the other.
An alar spanning suture is then placed to bring the lateral crura together and further increase tip support. This buried 5-0 PDS suture is placed immediately behind the domes, near the lateral-most bite of the CTS. It is critical to avoid placing this suture too far laterally, as this may have a tendency to rotate the lateral crura cephalically, malpositioning them. This alar spanning suture works in conjunction with the CTS to tension the lateral crura and improve external valve patency.
If further tip projection and infratip length are desired, a shield graft works very well with the cranial tip sutures. This graft can be comprised of septal, rib, or ear cartilage. When placed with the leading edge of the graft further projecting than the domes, the tip defining points are redefined. This maneuver is particularly helpful in medium or thicker-skinned patients, as the transition from the flat lateral crura to the projecting shield graft can have a profound tip defining effect.
Rim grafts can be useful with cranial tip sutures, especially in revision cases in which the lateral crura are flimsy. In our experience, the CTS maintain the integrity of the caudal edges of the lateral crura, obviating their need in most primary cases.
Lastly, the cranial tip sutures and domes are camouflaged with a soft tissue graft. This can be temporalis or rectus abdominus fascia. We also harvest Pitanguy’s ligament, the intercrural fat pad, and a portion of the nasal SMAS (in medium and thick-skinned patients) as a free soft tissue graft during the opening of the nose. This free nasal SMAS graft is secured at the end of the case over the tip, infratip, supratip, to reduce the incidence of bossae. Even though the knots of the CTS are buried between the domes, the SMAS graft further ensures their coverage. If the supratip break is too pronounced after the domes are brought together, this soft tissue graft can soften it.
Discussion
The senior author (UM) has utilized this Cranial Tip Suture technique in 425 primary and revision rhinoplasty cases over the past 2.5 years. This technique has resulted in a noted improvement in tip shape, symmetry, predictability, and external valve function. Cranial tip sutures allow the rhinoplasty surgeon to follow somewhat of an algorithm to create the consistently perfect nasal tip shape. Asymmetries of the domes, lateral crura, and intermediate crura are all easily corrected with CTS and the associated tip maneuvers we described above.
The value of the rotational effect of dropping the cephalic margin of the lateral crus while maintaining the strength and shape of the caudal margin cannot be overstated. This avoids the unfavorable tip shadowing, rim collapse, and alar crease deepening of over-aggressive LLC resection or traditional domal/interdomal sutures. In our experience, cephalic trims tend to be more conservative, if needed at all, when used in conjunction with the CTS. Resection of the scroll is also less likely to be needed.
The tensioning effect of CTS placement is also important to consider. The lateral crus is drawn medially as the cranial tip suture is tightened, creating a “canvas and tentpole” effect over the caudal septum +/- caudal septal extension graft. This lateral crural tensioning effect is well-described by Davis et al., providing improved external valve patency without the need for additional structural grafts such as lateral crural struts9. This inferomedial transposition of the lateral crura can have a lateral crural steal effect, as the CTS can define the dome at whatever position is desired. The alar spanning suture combined with the CTS has a “butterfly effect” on the lateral crura, which further improves the external valves.
Choice in suture can utilize absorbable and nonabsorbable materials, but permanent suture is preferred. In our practice, this is a 5-0 Prolene suture with a P-3 needle. Kovacevic, et al. initially used PDS suture for the CTS technique, but switched to non-absorbable suture after noticing two patients required revision surgery due to a loss of lateral crural flattening after 6 months. They reported sustained results in the remaining patients after this change in suture material. In our experience, we have not seen CTS related infections or extrusions in over 400 cases. The sutures are buried between the domes after the infradomal suture placement and then further covered by the soft tissue onlay. We do irrigate the nose thoroughly intraoperatively and use perioperative IV and oral antibiotic prophylaxis in all nasal cases.
Below we illustrate two primary and one revision case in which cranial tip sutures plus the associated tip techniques were utilized.
Clinical Cases

21-year-old female with a long-standing history of difficulty breathing through both sides of her nose, and history of two nasal bone fractures in the past while playing college lacrosse.
Exam:
- Slight deviation of the tip to the right side with deviation of the nasal bones and the middle vault towards the left
- Right upper lateral cartilage narrowing
- Large dorsal hump and bulbous tip with divergent domes
- Normal tip rotation and projection
- Significantly deviated nasal septum towards the right and at the mid septum and at the base of the caudal septum
- Enlarged inferior turbinates and narrow internal valves, approximately 50-70% obstructed
- Breathing improves with the Cottle maneuver
Operative highlights:
- Left-sided caudal septal extension graft placed high on the caudal septum
- Cephalic trim performed bilaterally, reducing the width of lateral crura from 10 to 8 mm
- 5-0 Prolene cranial tip sutures
- 5-0 PDS alar-spanning suture
- 5-0 Prolene septocolumellar suture
- Free nasal SMAS graft placed over the tip, infratip, and columella

24-year-old female who was bothered by her tip droopiness, dorsal hump, and nasal overall size.
Exam:
- Narrowing of the middle vault with mild deviation of the nasal bones to the left
- Convex profile with tip ptosis and normal projection
- Wide sills with mild alar flaring
- Medium skin thickness
- Caudal septum is deviated to the left
Operative highlights:
- Right sided spreader graft
- Right-sided caudal septal extension graft
- 5-0 Prolene cranial tip sutures
- 5-0 PDS alar-spanning suture
- 5-0 Prolene septocolumellar suture

48-year-old transgender male-to-female patient with difficulty breathing through both sides of her nose, worse on her right side. She previously had a rhinoplasty with a silicone implant placement in 1997. The implant extruded and she had a revision surgery with Gore-Tex and ear cartilage placement in 2006.
Exam:
- Palpable implant on the dorsum, which was deviated towards the right side
- Collapse of her bilateral upper lateral cartilages, worse on the right side
- Convex profile that is prominent at the rhinion as well as the anterior septal angle
- Thick skin and a pollybeak deformity with an underprojected, over-rotated tip with a 105-degree angle
- Alar retraction bilaterally, worse on the left side
- Indented Weir scars from prior surgeries
- Right side of the airway approximately 60-70% obstructed
Operative highlights
- Rib cartilage harvest
- Removal of extensive fibrosis and GoreTex grafts
- Bilateral extended spreader grafts
- Caudal septal extension graft
- Shield graft
- Left-sided rim graft
- 5-0 Prolene Cranial tip sutures
- 5-0 Prolene septocolumellar suture
- 5-0 PDS alar spanning suture
- Replacement of fibrosis/free nasal SMAS graft over shield graft
Conclusion
Overall, cranial tip sutures offer numerous benefits for refinement of the tip, including consistent and reproducible tip shape, external valve stabilization, and ideal tip/alar transitions. They can be combined with other tip techniques for optimal tip shape and stability. They represent a tremendous advancement in our management of the nasal tip in rhinoplasty.
References
- Toriumi DM. New concepts in nasal tip contouring. Archives of facial plastic surgery. 2006;8(3):156-185.
- Kovacevic M, Wurm J. Cranial tip suture in nasal tip contouring. Facial Plastic Surgery. 2014;30(6):681-687.
- Gruber RP, Weintraub J, Pomerantz J. Suture techniques for the nasal tip. Aesthetic Surgery Journal. 2008;28(1):92-100.
- Corrado A, Bloom JD, Becker DG. Domal stabilization suture in tip rhinoplasty. Archives of facial plastic surgery. 2009;11(3):194-197.
- Dosanjh AS, Hsu C, Gruber RP. The hemitransdomal suture for narrowing the nasal tip. Ann Plast Surg. 2010;64(6):708-712.
- Boccieri A, Sciuto S, Cervelli V, Pascali M. Dome division: A viable technique today? Facial Plastic Surgery. 2016;32(6):664-670.
- Conrad K, Solomon P, Chapnik JS. Impact of vertical dome division on nasal airflow. The Journal of otolaryngology. 2000;29(3):162.
- Pellarin L, Santos Bosaipo C, Magalhães Suguri V, Lobato Gregório L, Gregório L. Partial domal division: A technique for tip refinement. Plastic and Reconstructive Surgery – Global Open. 2019;7(4):e2214.
- Davis, Richard. Lateral crural tensioning for refinement of the wide and underprojected nasal tip: Facial Plastic Surgery Clinics of NA. 2015;23(1):23-53.
