Introduction
Many patients presenting for rhinoplasty evaluation complain that their noses are too large. A subset of these patients complains of a bulbous shape to the end of their nose which they find unpleasing. They may also note nasal obstruction. Proper management of these patients requires identification of the anatomical factors contributing to the bulbous nasal tip and employment of individually tailored surgical techniques that focus on volume reduction and aesthetic refinement while preserving and, when necessary, enhancing tip support.
Anatomy
The bulbous nasal tip is characterized by excess volume in the nasal tip and supratip regions. The overall effect is that the lower third of the nose appears to have developed out of proportion to its neighboring structures. Depending on the thickness of the skin and the strength of the cartilage, the bulbous tip may be well defined or round and amorphous. Frequently the gracefully curving brow-tip aesthetic line is interrupted. The excess volume can come from excess skin and soft tissue, excess cartilage, or a combination of both.
While a thick skin and soft tissue envelope can help to hide subtle imperfections and tip cartilage irregularities following rhinoplasty, it can also create unwanted fullness throughout a nose. This is especially true in the nasal tip region where nasal projection is at its maximum. Thickening of the skin, fibromuscular layer (the nasal SMAS), or fibrofatty tissue can all contribute to a bulbous nasal tip. The lower lateral cartilages are typically loosely approximated at the midline by the interdomal ligament; excess interdomal volume pushes the domes laterally, increasing the angle of domal divergence and contributing to a bulbous tip.
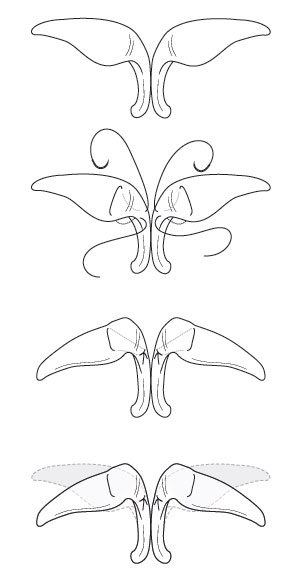
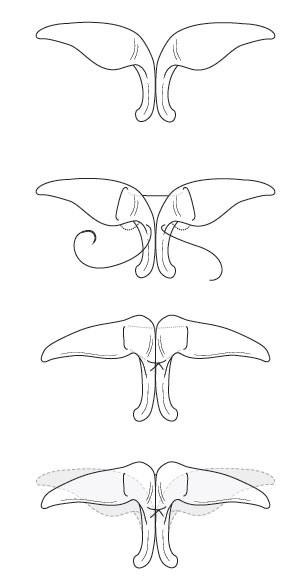
The lower lateral cartilages contribute greatly to the overall shape of the lower third of the nose. The intermediate and lateral portions of the lower lateral cartilages can contribute to a bulbous nasal tip through their relative size and orientation. Overly wide intermediate crura contribute excess volume in the infratip area and create excess domal width. The lateral crura of the lower lateral cartilages contribute most directly to a bulbous nasal tip. Most of the excess bulk that defines a bulbous tip comes from excess vertical height of the lateral crura (from the caudal margin to the cephalic margin). The shape and orientation of the lateral crura are another contributing factor. The lateral crura can be overly convex, which contributes to the overall roundness of the tip and can contribute to external nasal valve obstruction by narrowing the nasal vestibule. In addition, the lateral crura may be vertically oriented in the bulbous tip. This creates the parenthesis deformity which is evident in affected patients on frontal view (Figures 1 and 2).
|  |  |  |  | Before | After | Figure 1 and 2 | ||||||||
 |  | ||||||||||||||
 |  | ||||||||||||||
| Before | After | ||||||||||||||
| Figure 1 and 2 | |||||||||||||||
The proper management of the bulbous nasal tip depends on the accurate identification of the anatomic factors involved in a given nose. Sound rhinoplasty techniques focus on decreasing nasal tip volume and increasing definition while enhancing nasal tip support.
Management
Management principles for the bulbous nasal tip focus on decreasing the size and refining the overall shape. These steps can be combined with other rhinoplasty techniques depending on the need to alter nasal projection, length, and rotation. The goal is to produce an aesthetically pleasing nasal tip that functions well and is in balance with the rest of the face. A combination of tissue excision and shaping techniques via either endonasal or open approaches can be used depending on the preferences of the individual surgeon.
After the lower lateral cartilages are exposed, the tip is inspected to determine the relative volume contributions from the subcutaneous tissues and the shape and size of the lower lateral cartilages. If excess subcutaneous tissue is present on the skin, it can be carefully excised. However, one should take special care to preserve the skin’s delicate blood supply and not overly excise the nasal SMAS which is important for dynamic function of the nose. Excessive injury to this intrinsic musculature may result in nasal valve collapse necessitating grafting techniques. Excess soft tissue in the interdomal region can be excised and later used as a graft to camouflage and soften the edges of cartilage grafts in thin skinned individuals. Most patients will have excess width of the lateral crura. This can be managed by resecting the cephalic edge of the lateral crus, taking care to leave an uninterrupted strip of cartilage that is a minimum of 6 to 7 mm wide. Doing so helps to ensure that the lower lateral cartilages will retain adequate strength in the post-operative period to resist the contractile forces of the healing skin and soft tissue envelope and prevent upward retraction or buckling of the crura and nasal valve collapse. The surgeon should remember that a cephalic trim may also serve to increase the rotation of the nasal tip; if this is not desired, adjunctive techniques designed to derotate the nasal tip may be needed. Transection of the lateral crura with resection or overlapping of the cartilage in the horizontal dimension may also be needed to decrease bulbosity (Figure 3). The surgeon should repair the transected cartilage with long-lasting absorbable or permanent suture to avoid post-operative alar collapse. This technique may be combined with a cephalic trim to narrow or rotate the tip. Once volume reduction has been achieved, the surgeon may proceed with maneuvers to refine the nasal tip shape and positioning.
|  |  | Figure 3a | Figure 3b | 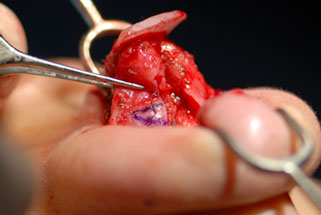 |  | Figure 3c | Figure 3d |  | Figure 3e | ||||||||||||
 |  | |||||||||||||||||||||
| Figure 3a | Figure 3b | |||||||||||||||||||||
 |  | |||||||||||||||||||||
| Figure 3c | Figure 3d | |||||||||||||||||||||
 | ||||||||||||||||||||||
| Figure 3e | ||||||||||||||||||||||
Suture techniques provide a powerful means of reshaping and defining the nasal tip. Following a cephalic trim, a nasal tip can remain ill-defined because of excess horizontal divergence of the intermediate crura. An intradomal suture is used to decrease the angle formed between the lateral crus and the intermediate crus (Figure 4). This suture can narrow the nasal dome, reduce convexity of the lower lateral cartilage, and slightly increase tip projection. A 4-0 or 5-0 suture is used in a horizontal mattress fashion in the region of the intermediate crus. The knot should be placed on the medial side of the dome such that it can be hidden in the interdomal area. If this technique does not provide enough definition of the nasal tip, a transdomal suture can be applied (Figure 5). This suture is useful in cases of uneven domal height or excess interdomal width. After the surgeon sets the desired height and symmetry of the domes, the intermediate crura are sewn closer together a point just proximal to the domes. This suture also serves to slightly increase tip projection. Care must be taken not to overly narrow the nasal tip with this technique. Along with excisional and suture techniques aimed at refining the nasal tip, cartilage grafts can, and in most cases should, be used to reinforce the structure of the nasal tip, ensuring a strong, lasting result.
| Interdomal Suture | Transdomal Suture | 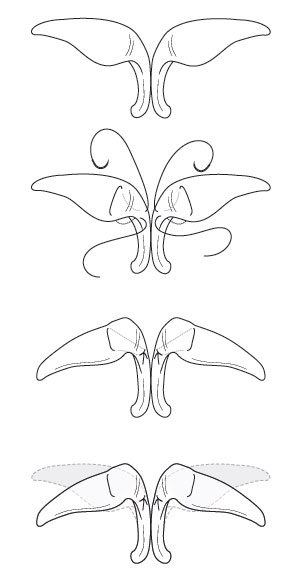 | 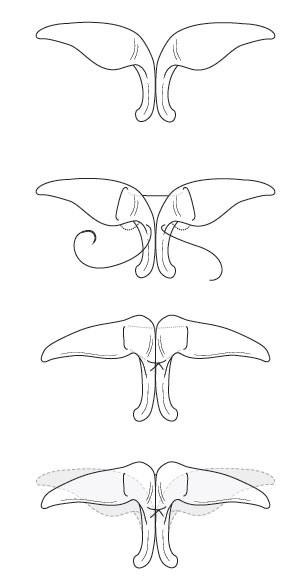 | Figure 4 | Figure 5 | ||||||
| Interdomal Suture | Transdomal Suture | |||||||||||
 |  | |||||||||||
| Figure 4 | Figure 5 |
A number of cartilage grafts can be used in the management of the bulbous nasal tip. Grafts may be harvested from the nasal septum, from the pinnae, or from rib cartilage, depending on the nature and amount of cartilage that is available and required. Recently, irradiated homologous costal cartilage has proven a stable, safe, and reliable source of grafting material if
http://companyofangels.co.uk/tag/cheap-cialis-online.php
adequate autologous sources are not available. It is critical to stabilize the nasal base and to provide tip support, typically with a columellar strut. These grafts should be made from the strongest cartilage available, preferably from the septum or rib. A pocket is dissected between the medial crura to just above the nasal spine. The graft is placed into this pocket, taking care to avoid placement directly onto the nasal spine as this may cause “clicking” with nasal manipulation in the postoperative period. The medial crura are then secured to the graft with absorbable sutures in a mattress fashion. The base of the septum may then be secured in the midline using a “Wright suture.” This suture secures the septum and both mucoperichondrial envelopes to the tough midline nasal spine periosteum. This serves as an excellent anchor for the newly reinforced columellar complex.
After the nasal base is stabilized, the lateral crura can be addressed. Lateral crural strut grafts are used in reshaping overly convex lateral crura. These grafts are typically made from septal cartilage carved to 3-4 mm in width and 15-25 mm in length. They are placed into a pocket dissected between the underside of the lateral crus and the vestibular skin. Ideally they are long enough to span from the dome region to the piriform aperture. This not only flattens the overly convex lateral crus but also reinforces the caudal ala and helps prevent alar retraction and external valve collapse. Alar rim grafts are useful adjuncts to lateral crural strut grafts. In the bulbous nasal tip, the lateral crura are typically cephalically oriented which leaves the lateral ala without rigid structure. The ala can therefore be notched, flared, and prone to collapse. Alar rim grafts are designed to combat all these tendencies. They can be placed through a marginal infracartilaginous incision or through a stab incision in the lateral vestibule. A pocket is dissected along the alar and the long, thin grafts are inserted. Rim grafts are typically 2-3 mm in width and 15 to 25 mm in length. The edges are beveled when necessary and the medial ends are gently softened to help prevent palpability. These grafts may be immobilized with 5-0 gut sutures to fixate them to the skin and soft tissue envelope.
Conclusion
The bulbous nasal tip presents a technical challenge to every rhinoplasty surgeon. Surgeons must remember to show restraint in their approach to a bulbous tip to avoid creating a tip with an “operated” appearance that is poorly supported. Successful management depends on a combination of excision, suture, and grafting techniques that remove excess tip bulk, define tip shape, and reinforce tip support.
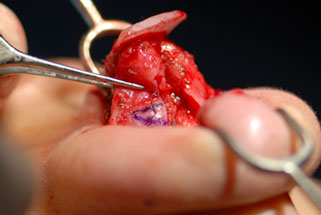
Figure 1: Frontal view of a patient with a bulbous nasal tip and very thin skin. The parenthesis deformity is evident.
Figure 2: Oblique view. Procedures performed included: septoplasty, bilateral middle vault spreader grafts, dorsal onlay graft using E-PTFE, columellar strut, tip graft, and resection of a portion of the horizontal dimension of the lateral crura.
Figure 3: (A, B)This patient had bulbous lower lateral cartilages in addition to very thick skin. (C, D,E) The lateral crura were transected in the horizontal dimension, with excision of superiorly-based wedges of cartilage to reduce the volume and width of the nasal tip. The transected cartilage was repaired with PDS suture. A tip graft was used to help improve tip definition.
Figure 4: Interdomal suture technique
Figure 5: Transdomal suture technique
1Daniel RK. The Nasal Tip: Anatomy and Aesthetics. Plast Reconstr Surg 1992 Feb; 89(2):216-224.
2Touriumi DM, Checcone MA. New Concepts in Nasal Tip Contouring. Facial Plast Surg Clin N Am 17(2009): 55-90.
3Gruber RP, Friedman GD. Suture Algorithm for the Broad or Bulbous Nasal Tip. Plast Reconstr Surg 2002 Dec; 110(7):1752-1764.
4Kridel RW, Ashoori F, Liu ES, Hart CG. Long-term use and follow-up of irradiated homologous costal cartilage grafts in the nose. Arch Facial Plast Surg. 2009 Nov-Dec;11(6):378-94.
5Gunter JP, Friedman RM. Lateral Crural Strut Graft: Technique and Clinical Applications in Rhinoplasty. Plast Reconstr Surg 1997 April; 99(4):943-952.
6Kofi DOB, Hilger P. Alar Rim Grafting in Rhinoplasty. Arch Facial Plast Surg. 2009 Sept-Oct; 11(5):285-289.
