Introduction
Rhinoplasty is an operation of many intricate complexities that also remains as much of an art as a science wherein “just enough, but not too much” manipulation of various structures is required for optimal outcomes. Surgical challenges that are critical to outcomes that may be addressed during rhinoplasty include, among others, management of the bony nasal pyramid, management of middle nasal vault aesthetics and function, relationship of dorsal nasal height and nasal tip projection, nasal tip aesthetics, position and length of caudal septum and columella, relationship of medial crura to caudal septum and management of the nasal spine, premaxilla and nasolabial angle. Revision rhinoplasty brings additional complexity to management of these many challenges when significant scarring or asymmetry is present and when one or more structures may have been over-resected previously. Many elegant techniques have been described for these various facets of rhinoplasty and it is incumbent on the rhinoplasty surgeon to have sufficiency of knowledge and technical prowess to be able to choose and, within the context of patient desires and realistic possibility, then execute appropriate techniques for the variable anatomical findings encountered with each patient. But even with appropriate confidence, humility, knowledge and execution, rhinoplasty outcomes may not always fully meet surgeons’ and/or patients’ expectations.
Pre-operative computer imaging (PCI) has become a valuable tool to improve communication between patient and surgeon according to Mehta et al because it helps to reconcile differences between patient expectations and each surgeon’s aesthetic and also provides a mechanism for critical self-assessment.1 In their study experts’ comparison of PCI AP images to post-operative AP photographic images was more accurate than that for the PCI profile images versus post-operative profile images in three quarters of patients. While predictive accuracy of PCI depends on imaging skill, surgical expertise and other factors (e.g. healing variables; e.g. thickness of nasal skin) it has been said that surgical management of the lower nasal third may be the most challenging aspect of rhinoplasty.2 In appropriate patients the tongue-in-groove (TIG) technique in septorhinoplasty is a reliable method for controlling tip rotation and projection, reducing columellar show and straightening the caudal septum wherein “the intraoperative appearance closely approximates the expected long-term result”.2 Major potential pitfalls of the technique include widening of the caudal septum-medial crura complex, excessive advancement of the medial crura (including footplate) onto the caudal septum with creation of a columella defect and/or excessive tip rotation and flattening of the infratip lobule. Mastery of the TIG technique, however, may enable surgeons to improve the predictive accuracy of pre-operative PCI profile imaging in addition to enhancing overall surgical results and patient satisfaction.
Overview
The approach to rhinoplasty detailed herein, Medial Crural Sequential Vectoring Rhinoplasty, certainly does not apply to all patients and the myriad anatomical findings that may be encountered but when these techniques become second nature, they can be indispensable in helping rhinoplasty surgeons achieve favorable outcomes that ideally closely resemble PCI. The caudal septum is addressed first, followed by the nasal dorsum and middle vault, the columella and subnasale, the nasal tip and anterior septal angle and finally extra-structural aesthetic camouflage grafting, if needed.
Caudal Septum
A long caudal septum may extend beyond the anterior nasal spine tensioning the columella and upper philtral skin and shortening the distance between the tip defining point and the anteroinferiorly displaced subnasale. The nasolabial angle is typically more acute and excess columellar show is often present. The excess caudal septal cartilage pushes the columella soft tissue inferiorly such that it may encroach into the upper lip space and negatively impact upper lip aesthetics. Excess caudal septal length may be seen as “extra” tissue that may be easily resected enabling the native medial crura or a stabilized medial crura – columella strut complex to then passively adjust cephalically, often facilitated by appropriate resection of redundant vestibular skin.3 While caudal septal resection (if needed) and/or use of floating columella strut is a necessary skill that is commonly employed, where appropriate many rhinoplasty surgeons are increasingly in favor of preservation of caudal septal length as required for TIG.
The TIG technique avoids reliance on inherent nasal tip support mechanisms that may be routinely compromised during rhinoplasty (e.g. dome division; e.g. disruption of inter-crural ligaments; e.g. reducing anterior septal angle height) or that may otherwise be inadequate to maintain needed projection and/or support of the nasal tip. The TIG technique also avoids the potential for the posterior edge of a stabilizing columellar strut to engage with the caudal (anterior) edge of the septum and the potential for a clicking sensation with any manipulation of the nasal tip post-operatively.4
Midline caudal septal position must be achieved or maintained to help ensure midline positioning of the nasal tip upon completion of rhinoplasty and during the long term. Abnormal pre-operative findings may include but are not limited to minor caudal septal deflection to one side, more significant deviation to one side or a severe deformity with deviation of the anterior septum into one vestibule and curvature of the caudal septal edge into the contralateral vestibule. Repositioning the deviated caudal septum to the midline often requires complete release of perichondrium from both sides as well as release from nasal floor and anterior nasal spine soft tissues. After the septal cartilage is fully released a sequential approach to achieving midline position often requires resection of redundant inferior caudal septal cartilage (shortening the vertical segment of the L strut) to enable this segment to reposition to the midline. In cases where the septal cartilage displacement extends posteriorly along the nasal floor additional inferior septal cartilage may need to be resected to enable the entire structure to swing back to the midline (Metzenbaum swinging door)5. If the anterior/caudal septal cartilage is curved it may require scoring on the concave surface to facilitate straightening.6
Occasionally a stabilizing septal cartilage or bone graft (with or without caudal extension) may be needed for additional support and in cases of severe deformity the septum may require removal, ex vivo re-contouring and replacement.6 While various methods of stabilization of the repositioned caudal septum have been described an effective method involves use of a 4-0 Vicryl modified (non-locking) double loop mattress suture anchored on the side opposite the original deviation. The suture should engage the ipsilateral nasal floor periosteum, traverse the caudal septal cartilage, engage the contralateral nasal floor periosteum twice, re-traverse the caudal septal cartilage and then the ipsilateral nasal floor periosteum where it is then secured. Care should be taken to avoid fixation of the medial crura during this maneuver so as to not limit ability to advance them during TIG maneuvers. See VIDEO 1 for live demonstration of caudal septal repositioning and fixation.
Columella and Subnasale
The relative effects of position of medial crural mid-point fixation onto the caudal septum via TIG have been characterized: increasing horizontal (cephalic) advancement reduces columellar show and increases rotation with little effect on tip projection and stiffness; moving the location of vertical fixation toward the anterior septal angle enhances tip projection and rotation with little effect on columellar show or tip stiffness (Figures 1 – 4).4 The authors suggest that overclosure of the angle of divergence (angle between the posterior border of the medial crura and caudal edge of septum) may result in over-rotation of the nose.4
Figure Legends
For Figures 1 through 12 the solid gray rectangle represents the cartilaginous septum. The colored rectangles below the solid gray rectangle represent the medial crura. The blue dots in the middle of the colored rectangles represent the mid-point of the medial crura. The orange dots toward the left side of the colored rectangles represent the proximal medial crural fixation point. The colored stippled curvilinear outlines toward the right of each diagram represent the nasal soft tissue profile outline.
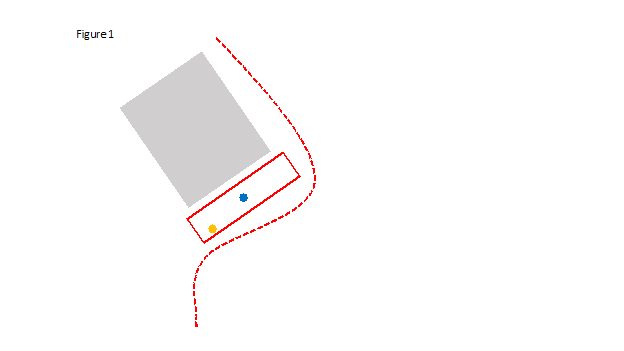
Figure 1 – Medial Crural Mid-Point Fixation TIG
Pre-operative position of medial crura (red rectangle) relative to nasal septum.
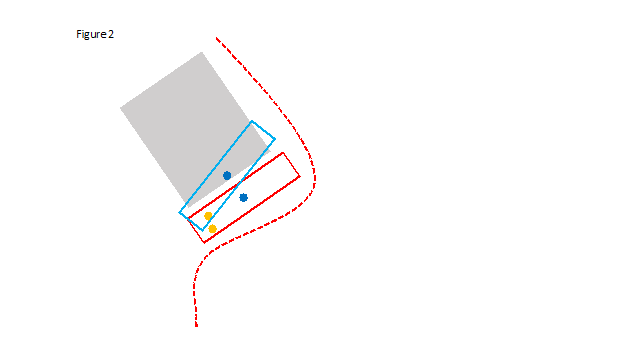
Figure 2 – Medial Crural Mid-Point Fixation TIG
Pre-operative position of medial crura (red rectangle) relative to nasal septum; cephalad rotation of medial crura (light blue rectangle) with fixation on septum at mid-point of medial crura.
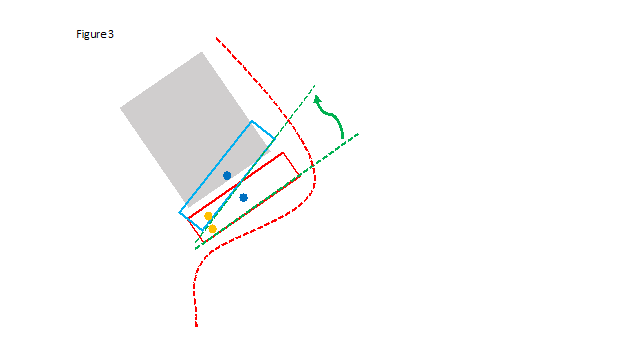
Figure 3 – Medial Crural Mid-Point Fixation TIG
Pre-operative position of medial crura (red rectangle) relative to nasal septum; cephalad rotation of medial crura (light blue rectangle) with fixation on septum at mid-point of medial crura. Stippled green lines at anterior edge of medial crura showing significant rotation and arc of rotation with fulcrum at proximal (base) of medial crura.
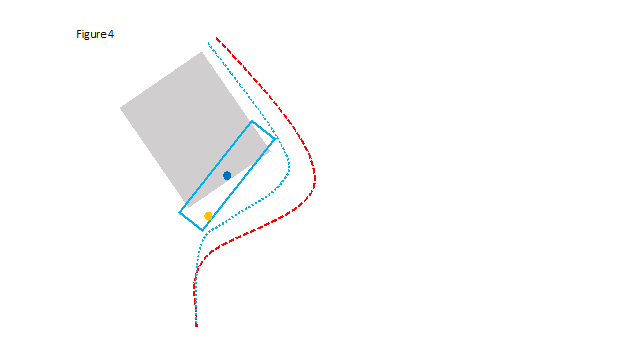
Figure 4 – Medial Crural Mid-Point Fixation TIG
Pre-operative position of nasal soft tissue profile (stippled red line); cephalically rotated medial crura (light blue rectangle) with fixation on septum at mid-point of medial crura; post-operative position of nasal soft tissue profile (stippled blue line).
An alternative concept for TIG, Medial Crural Sequential Vectoring Rhinoplasty (MCSVR), takes advantage of mobilizing the proximal medial crura as initial fixation points (orange dot Figures 1 through 12) versus mid-point of medial crura (blue dots Figures 1 through 12) with potential bidirectional initial movement of the columella at the subnasale (Figure 5): caudal-cranial advancement (solid orange arrow) and, if needed, anterior-posterior advancement, i.e. retro-positioning, stippled orange arrow). Increasing vertical fixation enhances upper lip aesthetics (opens up upper lip into more full view with reduction of downward projection of the proximal columella) and also presents the opportunity for simultaneous retro-positioning of the subnasale to increase columella length and relative projection of the nasal tip while minimizing tip rotation, if desired, with relatively little movement of the midpoint of the medial crura (blue dots, Figures 6, 7). Cephalad movement of the medial crura midpoint (Figures 2 – 4) involves a rotation arc with fulcrum at the proximal medial crura (Figure 3) that offers substantial tip rotation without the added benefit of significant movement of the proximal columella, if needed.
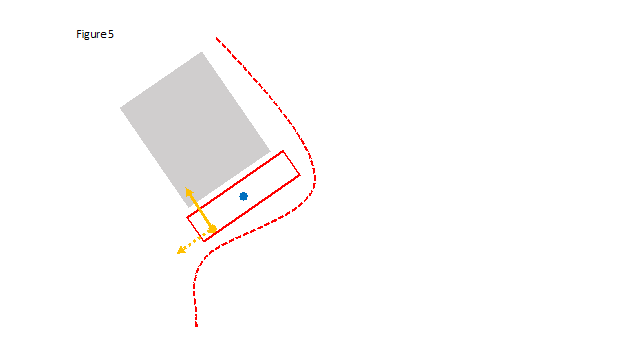
Figure 5 – Medial Crural Sequential Vectoring Rhinoplasty (MCSVR)
Potential bidirectional movement of the columella at the subnasale via mobilizing the proximal medial crura as initial fixation points (orange dot) versus mid-point of medial crura (blue dot): caudal-cranial advancement (solid orange arrow) and, if needed, anterior-posterior advancement, i.e. retro-positioning, stippled orange arrow).
In appropriate patients MCSVR enables more significant change to the nasolabial angle and improvement of upper lip aesthetics while also minimizing the potential for over-rotation of the nasal tip. The first arc of rotation involves mobilizes the base of the columella cephalically using a rotation arc with fulcrum at the distal medial crura (Figure 7). This maneuver closes the angle of divergence proximally (Figures 6 through 8) with relatively little effect on tip rotation. Avoiding a columella deficit requires conservatism in vertical fixation of the proximal medial crura; however, the importance of this initial stabilization of the columellar base component of the tripod cannot be overstated. If needed a cartilaginous premaxilla-columella onlay graft may be used preemptively or as a simple in office corrective measure post-operatively. A second arc of rotation with fulcrum at the now fixated proximal crura then enables customization of nasal tip rotation (Figures 9 through 12). The new angle of divergence may also be closed completely without over-rotation of the nasal tip if caudal septal length is adequate. Depending on caudal septal length, a caudal septal extension graft is occasionally needed to enable desired tip positioning (projection and rotation) with TIG medial crural fixation maneuvers.
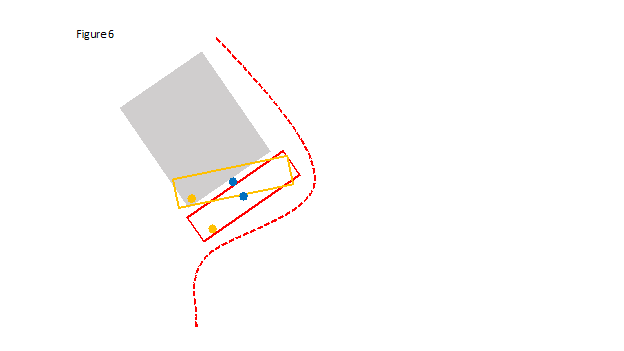
Figure 6 – MCSVR, First Rotation Arc
Pre-operative position of medial crura (red rectangle) relative to nasal septum; cephalad rotation with slight posterior retro-positioning of proximal medial crura (orange rectangle) with fixation on septum at anterior or leading edge of proximal medial crura.
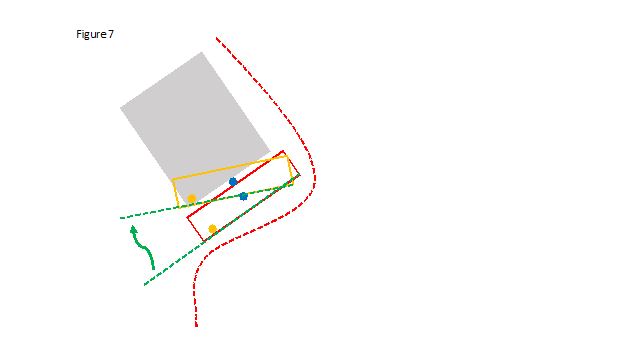
Figure 7 – MCSVR, First Rotation Arc
Pre-operative position of medial crura (red rectangle) relative to nasal septum; cephalad rotation with slight posterior retro-positioning of proximal medial crura (orange rectangle) with fixation on septum at anterior or leading edge of proximal medial crura. Stippled green lines at anterior edge of medial crura showing significant cephalad rotation of base of columella and arc of rotation with fulcrum at distal aspect of medial crura.
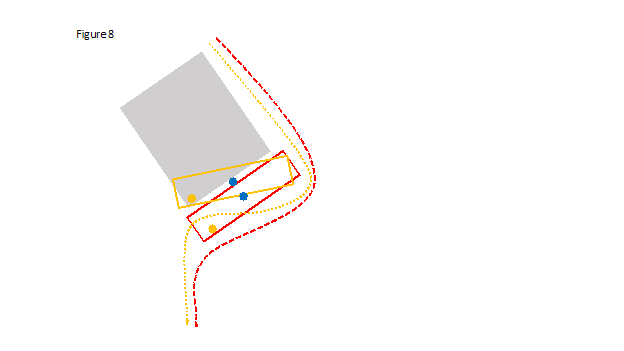
Figure 8 – MCSVR, First Rotation Arc
Pre-operative position of nasal soft tissue profile (stippled red line); cephalically rotated proximal medial crura (orange rectangle) with fixation on septum at anterior or leading edge of proximal medial crura; intra-operative temporary position of nasal soft tissue profile (stippled orange line).
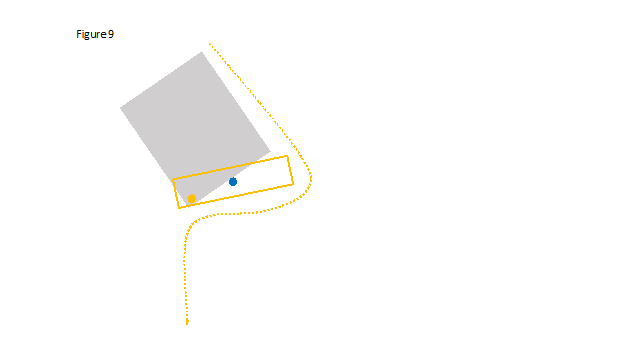
Figure 9 – MCSVR, First Rotation Arc Completed
Intra-operative position of nasal soft tissue profile (stippled orange line); cephalically rotated proximal medial crura (orange rectangle) with fixation on septum at anterior or leading edge of proximal medial crura.
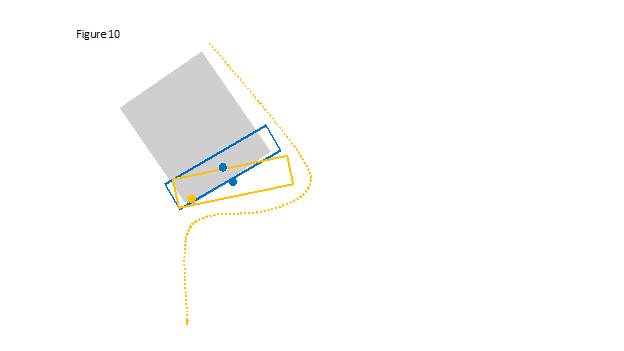
Figure 10 – MCSVR, Second Rotation Arc
Intra-operative position of nasal soft tissue profile (stippled orange line); cephalically rotated proximal medial crura (orange rectangle) with fixation on septum at anterior or leading edge of proximal medial crura; cephalically rotated mid- and distal medial crura (blue rectangle).
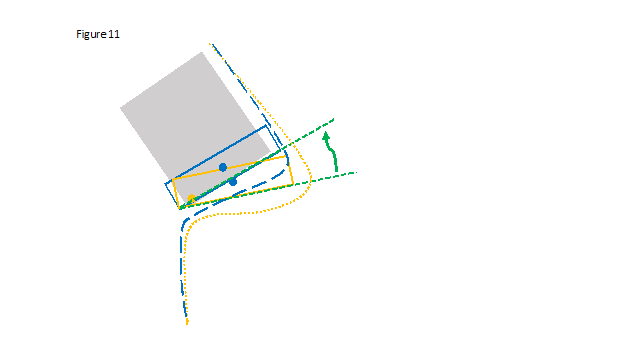
Figure 11 – MCSVR, Second Rotation Arc
Intra-operative position of nasal soft tissue profile (stippled orange line); cephalically rotated proximal medial crura (orange rectangle) with fixation on septum at anterior or leading edge of proximal medial crura; cephalically rotated mid- and distal medial crura (blue rectangle). Stippled green lines at anterior edge of medial crura showing significant rotation and arc of rotation with fulcrum at proximal aspect (base) of medial crura.
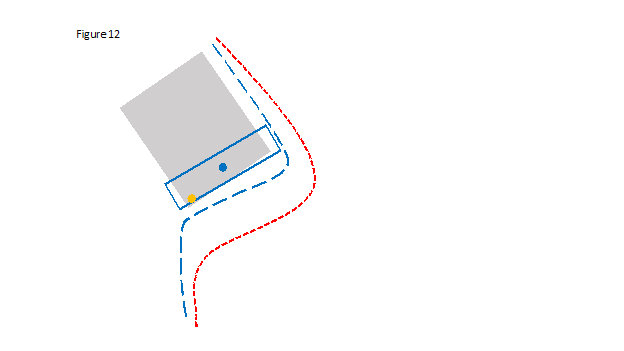
Figure 12 – MCSVR, First and Second Arcs of Rotation Completed
Pre-operative position of nasal soft tissue profile (stippled red line); sequentially rotated proximal and distal medial crura (blue rectangle); post-operative position of nasal soft tissue profile (stippled blue line).
Initial cephalic advancement of the columella base may result in outward flaring of the medial crura and medial crural footplates that may not be fully corrected with closure of the transfixion incisions. Redundant anterior septal mucoperichondrial flap tissue may need to be resected along with a cuff of vestibular columellar skin and cartilage from the posterior edge of the medial crura – resection of anterior vestibular columellar skin should be limited, however, to avoid a post-operative wet nasal tip.2 The transfixion incision may also need to be extended inferiorly to fully avoid any secondary soft tissue fullness that may negatively impact the airway. Medial crural flaring may be reduced or avoided if the fixation point on the proximal medial crura is moved cephalad to the mid-position across the width of the medial crura. See VIDEO 2 for live demonstration of medial crural sequential vectoring.
Nasal Dorsum and Middle Vault
Adjusting dorsal height and contour including upper and middle third widths may ideally be done before additional distal fixation points (beyond initial positioning of the base) for TIG medial crural advancement are completed. Access to the dorsum for dorsal osteotomy, lowering dorsal septal cartilage height and resecting redundant upper lateral crura (if present after lateral osteotomies and medialization of the nasal bones) is more facile if the lower lateral crura have not been contoured and medialized at this point.
Nasal Tip and Anterior Septal Angle
After the base of the columella is anchored to the caudal septum with caudal-cranial advancement with or without retro-positioning, the mid columella is then anchored to the caudal septum with one or more fixation points. At this point the domes may extend beyond the dorsal plane of the septum and anterior septal angle and tip projection may be increased as the full potential length of the medial crura is realized as they are fully extended (any inherent lateral tensioning of the medial crura near the domes is negated as they are sequentially anchored to the caudal septum from their base toward the domes).
Ensuring that the domes project beyond the dorsal plane of the septum and anterior septal angle (as opposed to anchoring the domes to the septum at this same plane) is essential to maintaining some pliability and softness of the nasal tip as well as maximizing the opportunity for an aesthetically pleasing supra-tip break on profile view. If medial crural length does not position the domes above the dorsal plane of the septum and anterior septal angle then distal dorsal septal cartilage height may be lowered. Tip projection may be further modified as needed by appropriate maneuvers including intact domes (with or without dome narrowing) and inter-domal sutures (intact dome unit)3, dome division (with or without tip de-projection via limited cartilage resection) with inter-domal sutures (divided dome unit)3, lateral crural steal versus lateral crural overlay maneuver7, etcetera.
“Extra-Structural” Aesthetic Camouflage Grafting
As with any rhinoplasty one of the challenges that surgeons face during the procedure and especially at the end of the procedure is the ability to visualize in their mind’s eye the likely final result through the edema and structural “memory” of the skin flap as well as the potential space that is present between the skin flap and the underlying structures. Once the skin flap is initially replaced to its original position “extra-structural” cartilage camouflage grafting may be desired or needed to further enhance certain features or to minimize the likelihood of undesirable contours. Subtle dorsal width differences may be improved with crushed or morselized septal cartilage. The nasal tip defining point can also be elevated slightly and infra-tip lobule volume can be increased in a similar manner. Remnant septal or other cartilage may alternatively be contoured and shaped into various onlay grafts that are typically secured with suture material to enhance the nasal tip (e.g. increased nasal tip projection with cap graft9; e.g. increased projection and lengthening of the nose with shield graft10; e.g. softening of soft triangle facets with stabilized grafts11) and columella and/or pre-maxilla (a longer graft that adds volume to both the pre-maxilla and columella may be used12) if needed for any final adjustments to the nasolabial angle.
Conclusions and Summary
Figure sets 13 to 15, 16 to 18 and 19 to 21 demonstrate Medial Crural Sequential Vectoring Rhinoplasty in three patients with substantial correlation between pre-operative PCI profile images versus post-operative profile images. In appropriate patients this sequential proximal columella then nasal tip vectoring modification of TIG rhinoplasty may help improve reliability of primary and revision rhinoplasty outcomes as well as patient satisfaction. Major benefits of the technique include improved control of nasal tip rotation and projection along with enhancement of upper lip aesthetics. A proximal columella soft tissue deficit should be pre-empted but is also relatively simple to correct secondarily.
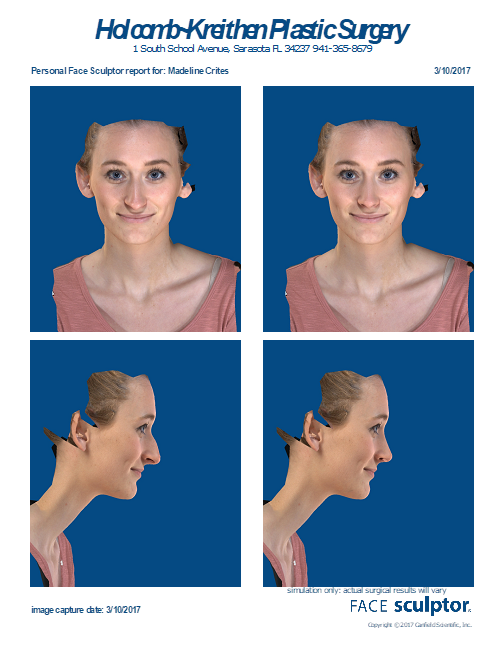
Figure 13 – Patient 1, Primary Rhinoplasty with MCSVR
Front and lateral Pre-Operative Computer Imaging (PCI). Pre-operative views show dorsal soft tissue excess, narrow middle nasal vault, mild tip asymmetry, infra-tip fullness, over-projected nasal tip, prominent anterior nasal spine, excess columella show with encroachment into upper lip space decreased vertical height upper lip, acute nasolabial angle.
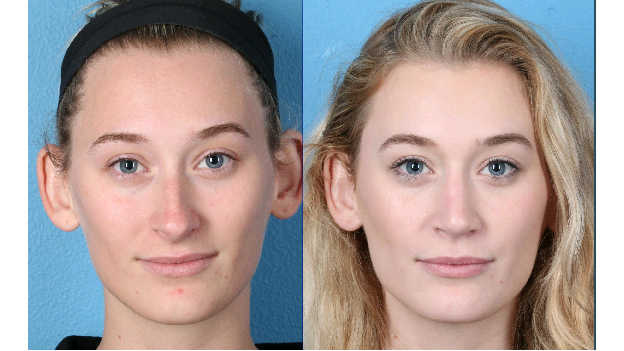
Figure 14 – Patient 1, Primary Rhinoplasty with MCSVR
Front before and 6 months after digital photographic images showing improvement in middle nasal vault width, tip symmetry and position and improved upper lip aesthetics.

Figure 15 – Patient 1, Primary Rhinoplasty with MCSVR
Front right lateral and 6 months after digital photographic images showing reduction of dorsal soft tissue excess, nasal tip deprojection and cephalic rotation, decreased columellar show, improved nasolabial angle and upper lip aesthetics. Note substantial similarity of front and lateral PCI and post-operative front and lateral digital photographic images.
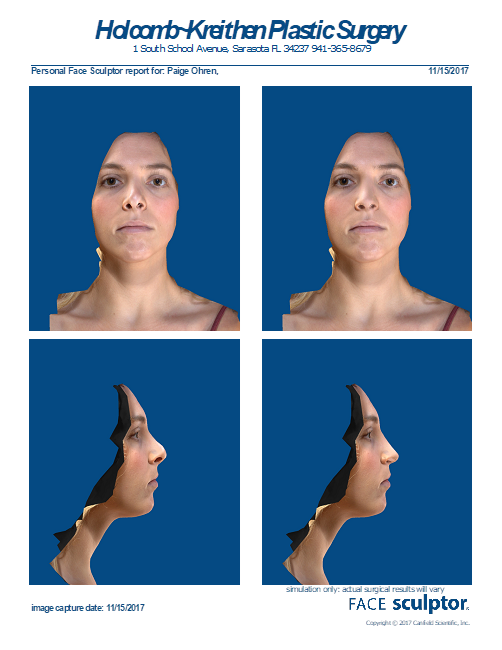
Figure 16 – Patient 2, Revision Rhinoplasty with MCSVR
Front and lateral Pre-Operative Computer Imaging (PCI). Pre-operative views show dorsal soft tissue excess, narrow and asymmetrical middle nasal vault with inverted V deformity, tip asymmetry and increased width, columella deviation to right, mild asymmetry alae, over-rotated nasal tip, slightly prominent anterior nasal spine and excess columella show with encroachment into upper lip space.

Figure 17 – Patient 2, Revision Rhinoplasty with MCSVR
Front before and 16 months after digital photographic images showing improvement in middle nasal vault width with elimination of inverted V deformity as well as restoration of tip symmetry.

Figure 18 – Patient 2, Revision Rhinoplasty with MCSVR
Front right lateral and 16 months after digital photographic images showing reduction of dorsal soft tissue excess, caudad rotation nasal tip, decreased columellar show, improved nasolabial angle and upper lip aesthetics. Note substantial similarity of front and lateral PCI and post-operative front and lateral digital photographic images.
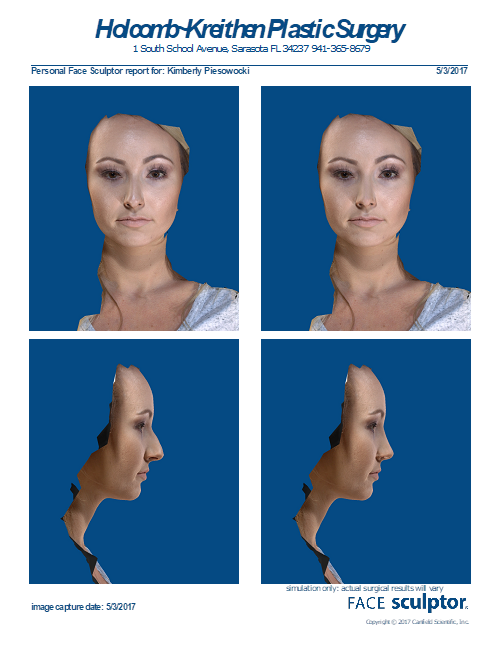
Figure 19 – Patient 3, Primary Rhinoplasty with MCSVR
Front and lateral Pre-Operative Computer Imaging (PCI). Pre-operative views show dorsal soft tissue excess, mildly increased tip width, nasal tip over-projection and under-rotation with decreased vertical height upper lip, slightly prominent anterior nasal spine and acute nasolabial angle.

Figure 20 – Patient 3, Primary Rhinoplasty with MCSVR
Front before and 6 months after digital photographic images showing improvement in nasal tip width and softening of soft triangle facets.

Figure 20 – Patient 3, Primary Rhinoplasty with MCSVR
Front before and 6 months after digital photographic images showing improvement in nasal tip width and softening of soft triangle facets.

Figure 21 – Patient 3, Primary Rhinoplasty with MCSVR
Front right lateral and 6 months after digital photographic images showing reduction of dorsal soft tissue excess, nasal tip deprojection and cephalic rotation, decreased columellar show, improved nasolabial angle and upper lip aesthetics. Note substantial similarity of front and lateral PCI and post-operative front and lateral digital photographic images.
References
- Mehta U, Mazhar K, Franel AS. Acurracy of preoperative computer imaging in rhinoplasty. Arch Facial Plastic Surg 2010;12(6):394-8
- Kridel RWH, Scott BA, Foda, HMT. The tongue-in-groove technique in septorhinoplasty: a 10-year experience. Arch Facial Plastic Surg 1999;1:246-56.
- McCollough, EG and Mangat, DS. Sytematic approach to correction of the nasal tip in rhinoplasty. Arch Otolargyngol 1981;107(1):12-6.
- Spataro EA and Most SP. Tongue-in-groove technique for rhinoplasty: technical refinements and considerations. Facial Plast Surg 2018;34(5):529-38.
- Pastorek NJ and Becker DG. Treating the caudal septal deflection. Arch Facial Plast Surg 2000;2(3):217-20.
- Lee JW and Baker SR. Correction of caudal septal deviation and deformity using nasal septal bone grafts. JAMA Facial Plast Surg 2013;15(2):96-100.
- Foda HM and Kridel RW. Lateral crural steal and lateral crural overlay: an objective evaluation. Arch Otolaryngol Head Neck Surg 1999;125(12):1365-70.
- Rohrich RJ and Deuber MA. Nasal tip refinement in primary rhinoplasty: the cephalic trim cap graft. Aesthet Surg J 2002;22(1):39-45.
- Kamer FM and Churukian MM. Shield graft for the nasal tip. Arch Otolarygol 1984;110(9):608-10.
- Goodrich JL and Wong BJF. Optimizing the soft tissue triangle, alar margin furrow and alar ridge aesthetics: analysis and use of the articulate alar rim graft. Facial Plast Surg 2016;32(6):646-55.
