Introduction
The subalar graft, was developed to resolve the central facial skin surface anatomic asymmetries associated with a unilateral hypoplastic maxilla in the rhinoplasty patient. In addition to the common rhinoplasty patient complaints of nasal dorsal hump, wide nasal dorsum, boxy nasal tip, ptotic tip, projecting tip, etc. these patients exhibit a distinctive group of findings that are not ordinarily addressed at rhinoplasty. These findings include: 1) an ipsilateral hidden ala when viewed for the front (because the nasal tip is rotated to the affective side), 2) an ipsilateral elevated alar sill, 3) an ipsilateral deep nasolabial sulcus, and 4) an ipsilateral elevated oral commissure (Fig.1).
Ordinarily, the rhinoplasty patient with these findings does not indicate that they want these findings changed or even recognize that an abnormality exists. In these patients, the asymmetries have been present from birth. While the asymmetries give an appearance of facial distortion to the observer, they are in a sense a “normal look” to the patient. The one feature of this quartet of findings that may be noted by an observant rhinoplasty surgeon is the elevated alar sill. This feature, however is usually acknowledged as an anatomic variation which is not ordinarily correctable.
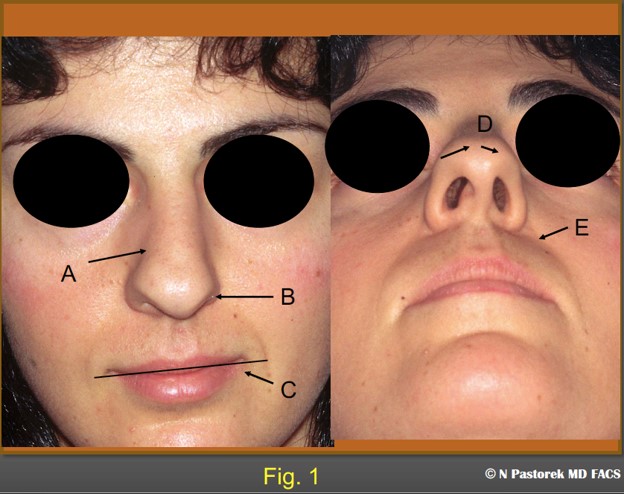
This is the index rhinoplasty case who presented with the additional facial surface findings of a hypoplastic maxilla. A) nose deviated to the left, B) ipsilateral elevated alar attachment, C) elevated oral commissure, D) deviated nasal tip, E) ipsilateral deep oral commissure.
The sub alar base graft was used in the initial index case in the early 1980’s by the author in a spontaneous fashion when at the completion of a rhinoplasty the four findings (especially the elevated alar sill) enumerated above diminished an otherwise good result. The initial thought of surgically elevating the lower alar sill (on the unaffected side) with an alar base resection seemed unreasonable and an external incision in this area has not been consented. It appeared as if the
unilateral deep nasolabial sulcus may be drawing the alar sill (on the affected side) upward as well as rotating the entire ala toward the deepened sulcus.
The subalar graft as described below and used in the index case had the immediate effect of rotating the ala toward the center face and lowering the alar sill to a position equal to the opposite side. (Fig. 2 and 3).

The preoperative and postoperative views of the patient at one year following rhinoplasty. Note the effects of the subalar graft. The nasal tip is rotated to the central position. The left alar attachment is now at the same level as the opposite side. The oral commissure on the left is now lower. The deep nasal labial sulcus is similar to the opposite side.

The pre- and postoperative submental views of index patient at one year post op. The boxy tip which was rotated to the right affected side is now more triangular in shape and positioned more centrally.
Alternative techniques
Maxillofacial orthognathic surgery with bone grafting can be performed to reposition the hypoplastic maxilla. But this is an extensive and invasive procedure with a prolonged associated recovery. The subalar graft is performed at the time of rhinoplasty with no additional instruments other than those used for the rhinoplasty and septal cartilage harvesting.
Patient Information
The facial asymmetries associated with a hypoplastic maxilla are not commonly recognized as entities in need of change by a patient seeking rhinoplasty. The subalar graft procedure is introduced to the patient as a way of lowering the elevated alar sill, elevating the deep nasolabial sulcus, rotating the nasal tip toward the midline, and the lowering the elevated oral commissure in a simple fashion that would add little additional operative time, morbidity, or length of recovery time to the overall rhinoplasty procedure. At the consultation, the patient is informed that the changes will be in degrees of improvement and may not result in complete symmetry. The graft to be used may be palpable but will not be observable.
In these cases, the surgeon is in reality offering a solution to a problem the patient, most likely, did not recognize. In the authors experience, however, not a single patient has turned down the opportunity to have a more symmetric face.
It is always in the best interest of the surgeon to have postoperative patients look as good as possible. When the subalar graft is indicated, the author has included the graft as part of the rhinoplasty procedure and not treated it as a separate procedure.
Surgical Technique
Rhinoplasty is planned to give the patient the best possible result despite the effect of the maxillary facial asymmetry. Most of these patients have a nasal septum deviation to the affected side. So, septoplasty is necessary most cases. Septoplasty is also necessary to obtain the largest possible septal cartilage for the subalar graft. An isosceles triangle shaped graft measuring 3cm x 1.5cm would be desirable in most cases.
A graft that is slightly smaller is still effective.
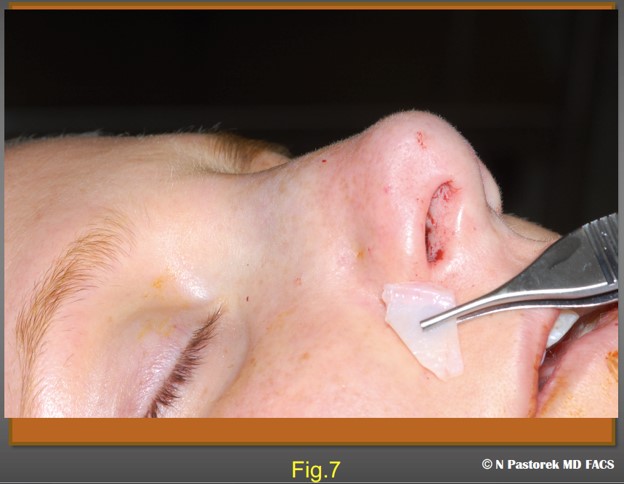
In the original index case, the subalar graft was placed at the conclusion of the rhinoplasty and this order of timing still seems the best. On the affected side, the osteotomy incision is used as the portal for the graft. The tissue over the canine fossa is infiltrated with local anesthesia. A pocket is made deeply down to the periosteum of the canine fossa in the direction of the nasolabial sulcus. The pocket is made with a curved Stevens scissors. The scissors are gently opened repeatedly to provide tissue separation of the soft tissue from the periosteum. It is important to not close the scissors completely while in the pocket because the facial artery is in this anatomic neighborhood and would be put at risk. If the pocket is made too large the graft will not be effective. The pocket should be just large enough to accept the graft so that the base of the graft observed at the edges of the osteotomy incision. This position places the base of the graft directly under the affected ala (Fig. 5,6,7,8,9,10). Usually in rhinoplasty, the mucosal incision for the osteotomy is not closed, but when the incision is used to accept a subalar graft a single 4-0 chromic suture is used at the site to prevent the graft from extruding.
The effect of the graft is immediate. On the operating table, the alar sill can be seen to be lowered, the ala and nasal tip is rotated more to the midline, the nasolabial sulcus is fuller, and the oral commissure is seen at level more even to the opposite side. The author’s opinion that the
contraction of the Zygomaticus major and minor is altered allowing the alar sill and the oral commissure to reposition downward.
It is possible that in the absence of septal cartilage that auricular cartilage or rib cartilage can be used for the subalar graft. All the patients to date in my practice have been primary cases where septum is available to harvest for grafting.
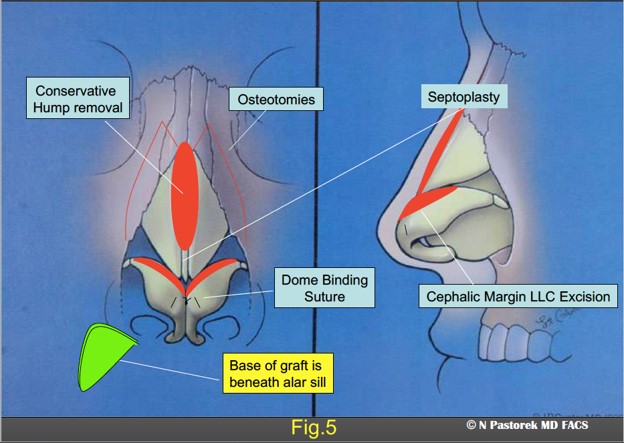
The graphic illustration shows the procedures of the rhinoplasty in this patient. The Sub Alar Graft is positioned at the conclusion of the procedure so the base of the triangular graft is beneath the elevated ala.
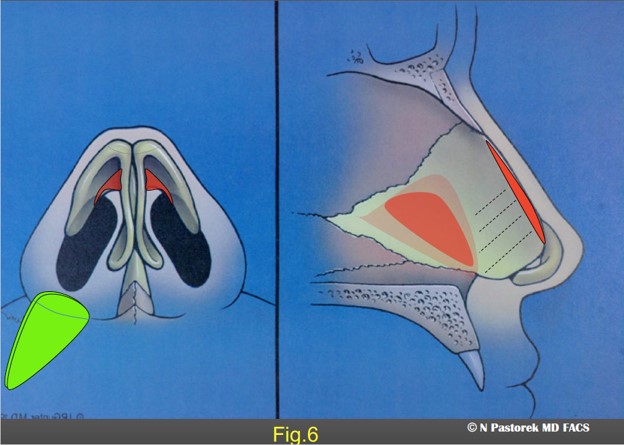
Base view illustration showing the positioning of the Sub Alar Graft beneath the elevated ala.
This figure shows the size and position of a Sub Alar Graft which will placed in dissected pocket over the periosteum of the canine fossa
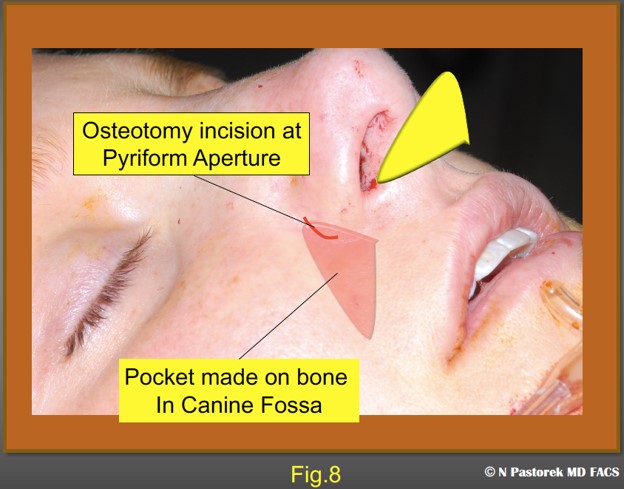
This figure illustrates the size and position of the dissection over the canine fossa periosteum via the incision made for a lateral osteotomy. The mucosal incision can be enlarged slightly but not much. There is an advantage in just slightly stretching the incision so that when the graft is placed the incision contracts over the graft.
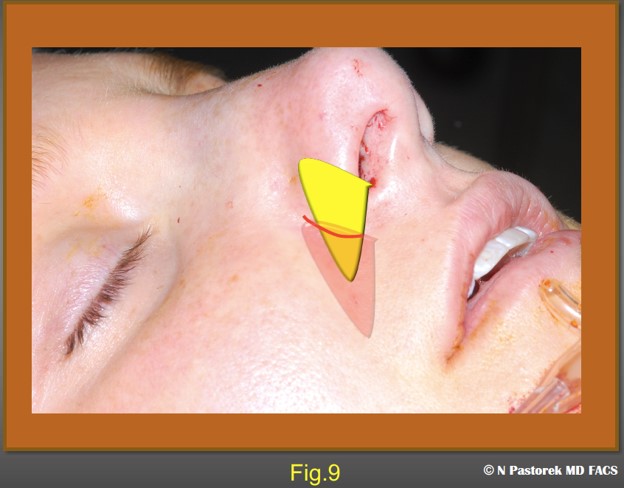
This illustration shows the osteotomy incision being stretched to accommodate the Sub Alar Graft which is larger than the incision.
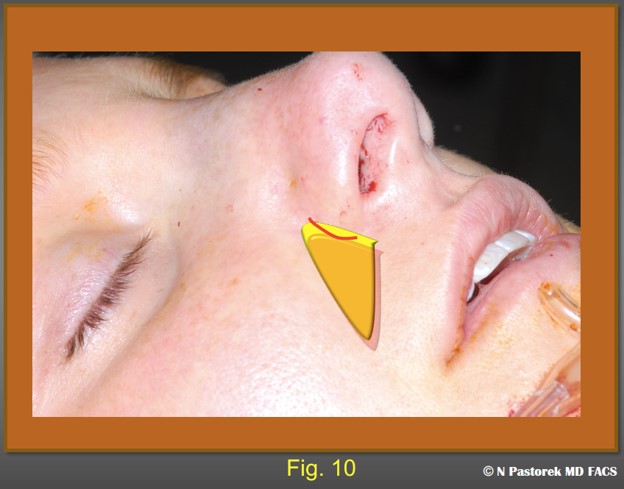
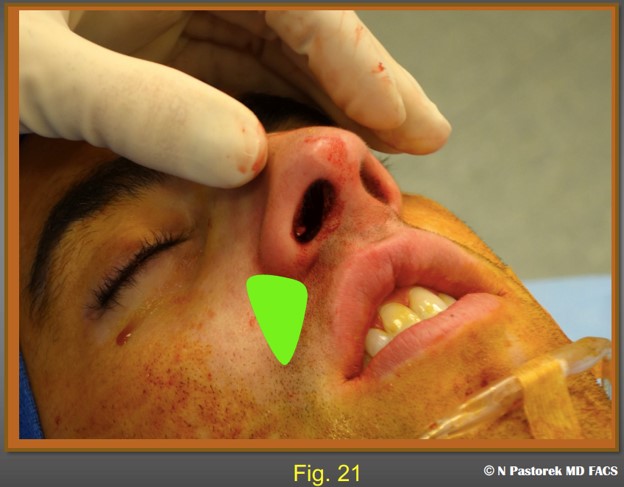
This illustration shows final ideal position of the graft with the base showing at the osteotomy incision. Usually, a single 4-0 chromic suture is used to close this incision to prevent the graft from migrating.
Surgical Tips
The corners of the graft should be slightly rounded to prevent any palpable edges. Use the biggest graft possible. Tell the patient that they may be able to palpate the graft under the midface skin. Note that the changes are in degrees and that perfect symmetry may not be achieved, but that without the graft the preoperative asymmetry would be unchanged. Do not make the graft pocket too large. The edge of the base of the triangular graft must be visible at the osteotomy mucosal incision. This observation places the bulk of the graft just beneath the alar base on the affected side where is most effective. To date no patient has objected to the improved central facial symmetry the subalar graft has produced.
Potential Complication
There have been no complications with the use of the subalar base graft since its inception over two decades ago. The chief potential complication of concern has always been bleeding from transection of the angular artery. The Stevens scissors has been used as a dissection instrument more than a cutting instrument, never actually closing blades of the scissors while in the pocket. Infection is possible though it has not occurred. The nasal inlet is swabbed with Betadine preoperatively, with Chlorhexidine if there is any history of MRSA, and with Mupirocin for 5 days preoperatively. The graft could, theoretically, come out of the canine fossa pocket to present in the nose. The osteotomy incision should be closed with one or two absorbable sutures.
Clinical Cases
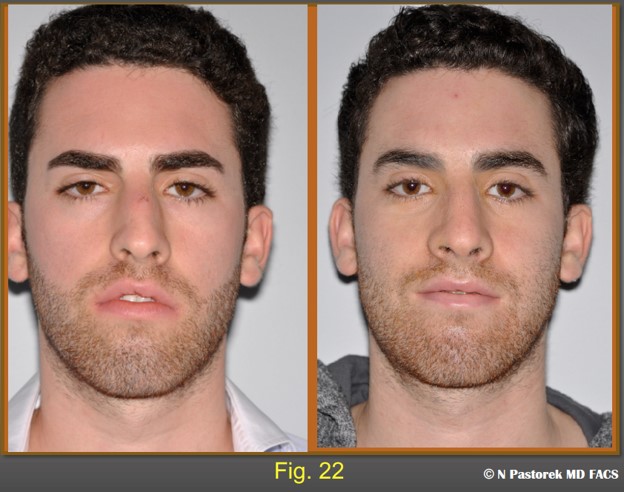
These patents presented for rhinoplasty without an awareness of the facial asymmetry. The possibilities of facial changes beyond those expected with rhinoplasty were discussed. An operative plan was designed to implement the Sub Alar Graft, Fig. 4, 11-24).


Preoperative and postoperative frontal views of the patient at one year. The significance of the Sub Alar Graft is most obvious in this view. The nose is straighter. The elevated alar margin is now lower and symmetric with the unaffected side. The oral commissure is lowered making the plane of the lips more horizontal.

Preoperative and postoperative submental views of the patient at one year, The Sub Alar Graft has helped to rotate the nasal toward a more central position. The nasolabial sulcus is more symmetric with the opposite side.

A 21year old patient presenting for rhinoplasty. The common elements seen of the physical examination suggesting that a subalar graft could improve the overall results of the rhinoplasty are. A) deviated nose to the left, B) an elevated left nasal ala, C) an elevated oral commissure, (D a relatively normal nasal tip rotated to the left, E) a deep nasal labial sulcus.

At one year postop this patient shows the degrees of improvement of a subalar graft in a rhinoplasty patient with a hypoplastic maxilla. Some improvement is always obtained. The patient is advised that the subalar graft is not usual in rhinoplasty cases. It is being use to lessen the surface effects of a hypoplastic maxilla. In this case the nasal tip is more centralized postoperatively, the alar sill attachment has been lowered, the oral commissure is lower and the nasal labial sulcus has been elevated.

The nasal tip has been rotated to the center face. Straightening the caudal septum is imperative, but the subalar graft aids is rotating the nasal tip. The nasolabial sulci are more symmetric.
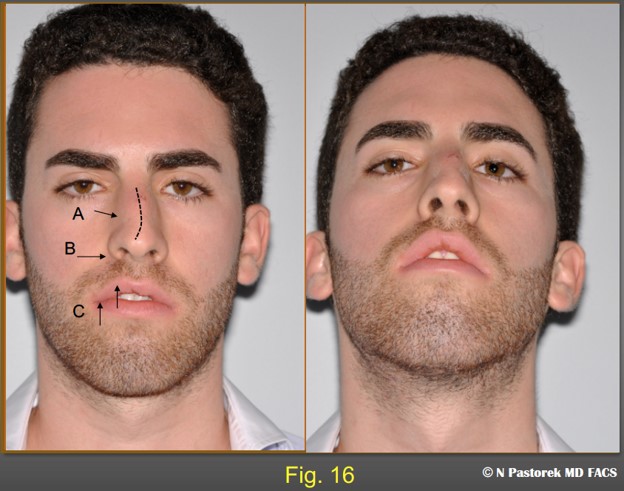
A traumatic nasal deformity in a 23 year old patient. The frontal view shows, A) nasal bone fracture and a possible upper lateral cartilage avulsion. He has additional pre -existing findings, B) elevated alar sill attachment on the right and a deep nasal labial sulcus. and C) an elevated right upper lip with poor lip closure. Though this is not a classic patient for the subalar graft he was considered a candidate for the procedure in addition to an open reduction of a nasal bone fracture and right upper lateral cartilage grafting.
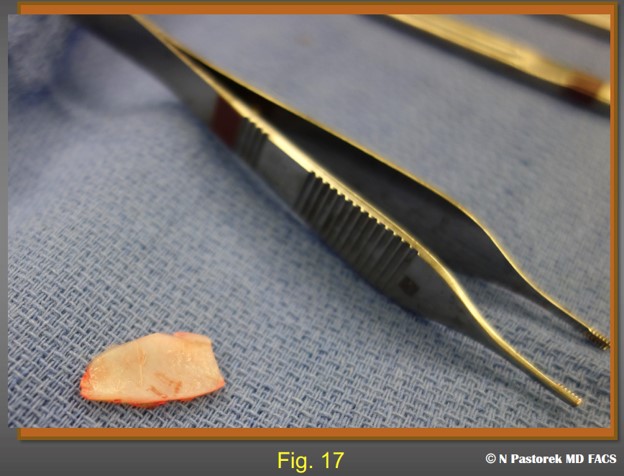
A septal cartilage segment for subalar grafting measuring approximately 3cm x 1.5 cm.
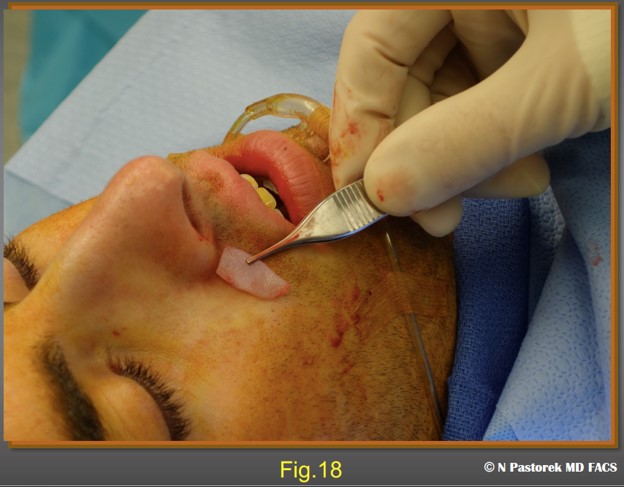
The position and relative size of the subalar graft is shown.

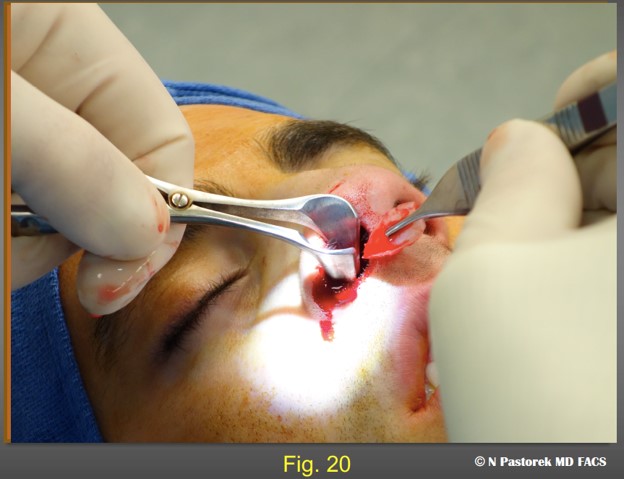
The subalar graft is being placed. The pocket should be slightly smaller than the graft so is held in place and does not float about once it is placed.
This pre- and post operative photo shows the effect of the subalar graft. The alar sill attachment has been lowered. The right lateral upper lip has been lowered so that there is a lip seal in repose.

This 23 year old female has all of the facial surface asymmetries of a hypoplastic maxilla, A) the nose is deviated to the right, B) there is a slight elevation of the right alar sill, C) the oral commissure is elevated, D) the normal nasal tip is rotated toward the affected maxilla, (E the right nasolabial sulcus is deeper than the left.

Pre- and Postoperative frontal views of the patient at one year. The effects of the subalar graft can be seen. The dorsum is midline, the alar sill attachments are symmetric, the nasal tip in centralized. And the right oral commissure has been lowered.

Pre- and postoperative submental views of the patient central positioning of the nasal tip and more symmetric nasolabial sulci.
Final Comments
Rhinoplasty patients who can benefit from the Sub Alar Graft are not seen frequently even in a busy practice. The incidence is probably less than one per hundred cases. But, once the syndrome is recognized and the solution is learned by the surgeon, these patients are among the happiest of good results.
Pertinent references
Effect of midfacial asymmetry on nasal axis deviation: indications for use of the subalar graft
Yao, F, Lawson, W, Westreich, RW
Arch Facial Plastic Surg. 2009 May-Jun; 11(3): 157-64. dol: 10.1001/archfacial.2009.1.
The subalar graft and its role in nasal tip medialization and improved nostril symmetry.
Aynechhi, BB, Mascaro ME, Rosenfeld, Westreich, RW.
Otolaryngology Head and Neck Surgery, 2013 Dec;149(6): 851-7
In an earlier a publication, Dr. Westreich gave credit to Dr. Pastorek in the form of a letter to the editor recognizing that the subalar graft procedure was learned from a presentation given by Dr. Pastorek at the Mt. Sinai Hospital in New York.
Structure Rhinoplasty: Lessons Learned in 30 Years Volume 1. Toriumi , D.,
