Funding/Financial disclosure:
The authors have no financial interest to declare in relation to the content of this article. No external funding was received.
Keywords: rhinoplasty, nasal tip, alar rim, lower lateral cartilage, sidewall, lateral crural strut graft, alar rim graft, nasal valve
Abstract:
The lower lateral cartilages are critical structures for maintaining tip projection, refining tip dynamics, and strengthening the nasal sidewall. Atypical orientation or lack of support from the lower lateral cartilages or nasal dome can lead to nasal tip fullness, blunting, de-projection, and static or dynamic nasal valve collapse. Classically, lateral crural strut and alar contour grafts are used to correct alar rim irregularities and sidewall deformity. Here, we present a novel surgical technique of the integrated alar-lateral crural strut graft, which combines features of the traditional lateral crural strut graft and alar rim graft. In our experience, the integrated alar-lateral crural strut graft is a versatile and viable alternative to conventional methods of optimizing tip dynamics, re-positioning lower lateral cartilages, and stabilizing sidewall support.
Introduction:
Modification of the lower lateral cartilages (LLCs) is a key component of controlling the nasal tip and sidewall in rhinoplasty. The paired alar cartilages differ in their shape, orientation, thickness, and resiliency. Together, they define the attributes of an aesthetically pleasing nasal tip while preserving patency and contour of the external nasal valve. The ideal alar rim has a smooth, curvilinear contour that extends from the tip-defining point to its lateral insertion at the nasofacial sulcus. Support for the alar rims are dependent on the integrity of the LLCs and their orientation within the nasal sidewall. Prior studies demonstrated that the lateral crura should lie in a plane at approximately 45 degrees relative to the axial plane. In addition, the caudal margin of the lateral crura should be positioned close to, or at the same level, as its cephalic margin.1
The characteristic anatomic relationship between LLCs and the alar rim has several functional and aesthetic implications. Cephalically oriented LLCs can cause inward movement of the alar rims, resulting in nasal tip fullness. The bulbous appearance of the tip and supra-tip on the frontal view also results in blunting of the boundaries between nasal tip and sidewall, forming the so-called “parenthesis-shaped deformity.”2 Additionally, a weakened lateral crus or under-supported alar rim can cause excessive pinching and static or dynamic collapse of the external nasal valve, leading to chronic nasal obstruction and difficulty breathing.3,4,5 Patients with cephalically oriented LLCs are more susceptible to unfavorable post-surgical results after rhinoplasty and have increased revision rates.6 Thus, sub-optimal orientation of LLCs and alar rim should be identified and promptly addressed during tip refinement procedures of rhinoplasty.
Conventional lateral crural strut graft:
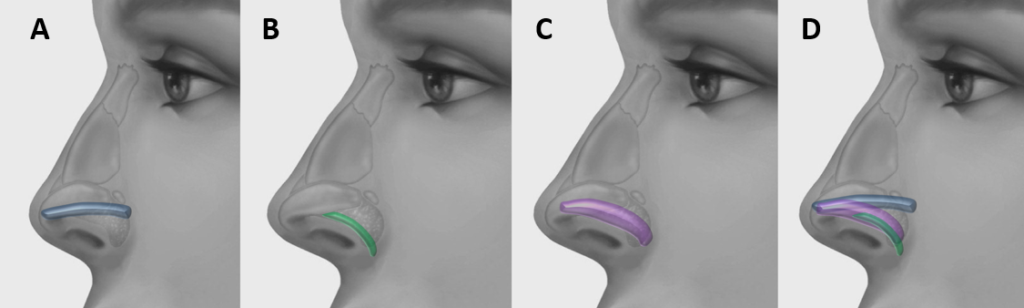
Structural and contour deformities of LLCs and alar rims may be addressed with placement of alar batten grafts, later crural strut grafts, composite grafts, and suture techniques during rhinoplasty. The lateral crural strut graft is one of the most commonly utilized techniques for correcting LLC malposition, strengthening lateral crural support, and increasing tip projection (Figure 1, panel A).7,8 To perform the lateral crural strut graft, cartilage graft is fashioned into segments of 15-25 mm in length and 3-4 mm in width.5 The graft material is placed into a soft tissue pocket on the undersurface of the lateral crus. The lateral crural strut graft is oriented in an axial plane following the trajectory of the lateral crus and extends towards the piriform aperture. The skin along the anterior two thirds of the lateral crus is left intact to prevent graft migration.
Since the original publication by Gunter and Friedman in 1997, the conventional lateral crural strut graft has undergone several modifications.7 Contemporary design of the lateral crural strut graft includes a shorter graft length and more caudal placement within the nasal sidewall.9 LLC re-positioning using this technique been shown to reduce nasal tip volume10 and improve tip definition.8,11 The classic lateral crural strut graft placement is depicted in panel A below.
Conventional alar rim graft:
The alar rim graft, or alar contour graft, is another useful technique for buttressing the nasal sidewall and is sometimes combined with the lateral crural strut graft. The alar rim graft is particularly effective in reducing alar notching and retraction.12 Alar rim grafts can be placed through either an external rhinoplasty approach, a marginal incision, or simply an isolated incision at the alar margin. Unlike the lateral crural strut graft, the alar rim grafts are thinner (6-8 mm in length by 1-3 mm in width) and placed along the caudal edge of the vestibular skin, rather than being oriented towards the piriform aperture. The alar rim graft is oriented following the posterolateral curvature of the alar rim. Furthermore, this type of graft is placed in a “floating fashion” within the soft tissue envelope and is typically not sutured to the caudal surface of the LLCs. An illustration of the alar rim graft placement is shown in Figure 1, panel B.
An integrated alar-lateral crural strut graft:
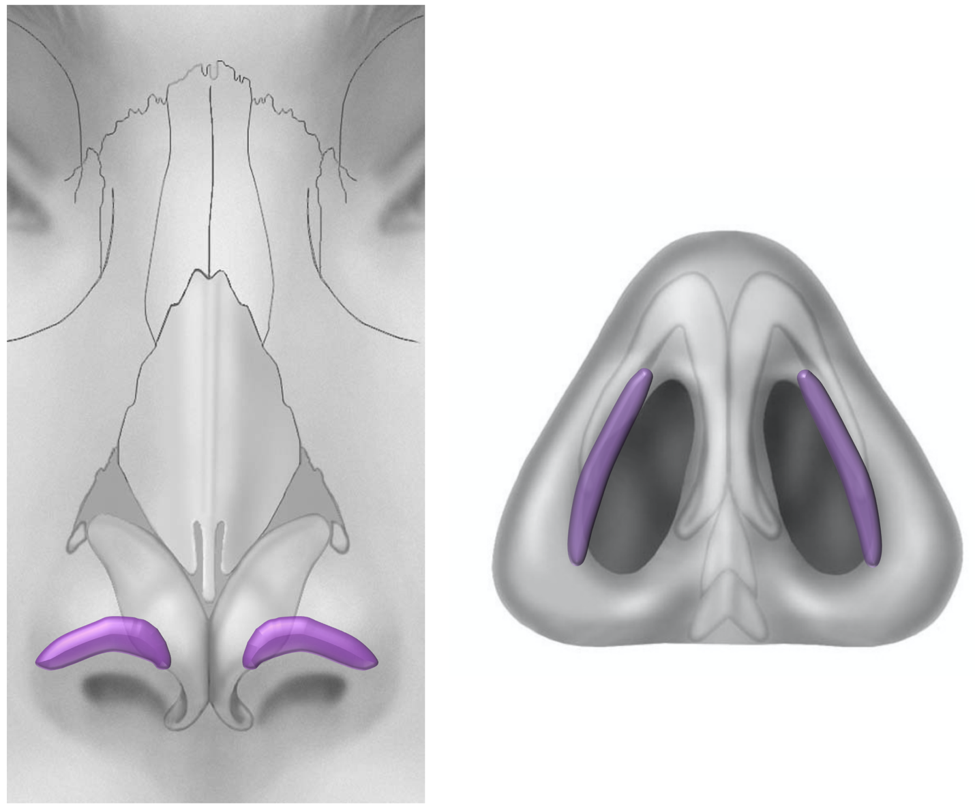
Here we demonstrate the novel concept of an integrated alar-lateral crural strut graft, which combines advantages of traditional lateral crural strut graft (designed for LLCs re-positioning and tip support) and alar rim graft (most often utilized for correction of sidewall collapse and alar notching). This method represents an evolution of contemporary grafting techniques to optimize tip dynamics and functional sidewall support. Figure 1, panel C and Figure 2 demonstrate the position and orientation of the integrated graft.
Operative technique:
The graft is most readily placed via an external rhinoplasty technique, although placement via an endonasal approach can also be performed. The operation involves first elevating the vestibular skin at the caudal edge of the LLCs. Next, a small soft tissue pocket is carefully elevated with Converse scissors underneath the vestibular skin (Figure 3, left).
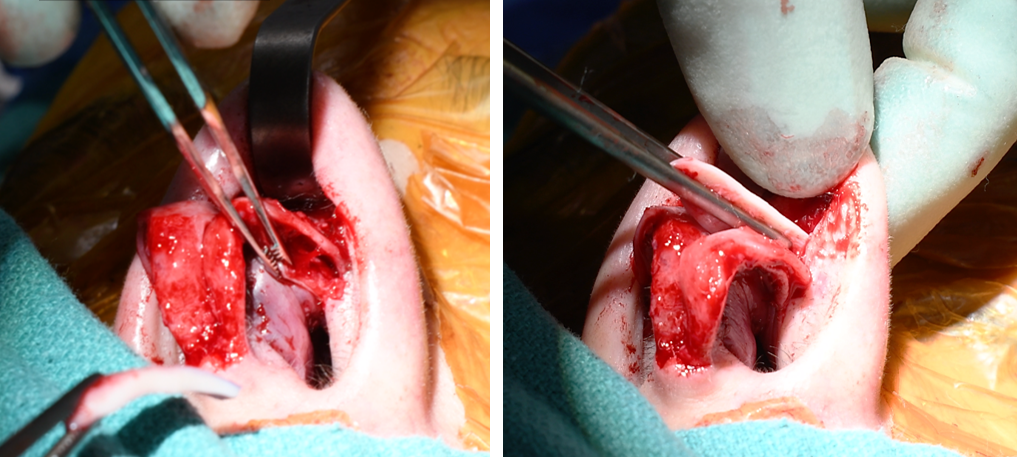
The soft tissue pocket is elevated laterally within the same region that is typically dissected for placement of an alar rim graft. Care should be taken to avoid perforation of the vestibular skin in this area. One of the key features of our dissection is that only partial elevation of the vestibular skin is performed to decrease fluid stasis and ischemia. This dissection should be more limited than with the traditional placement of a lateral crural strut graft.
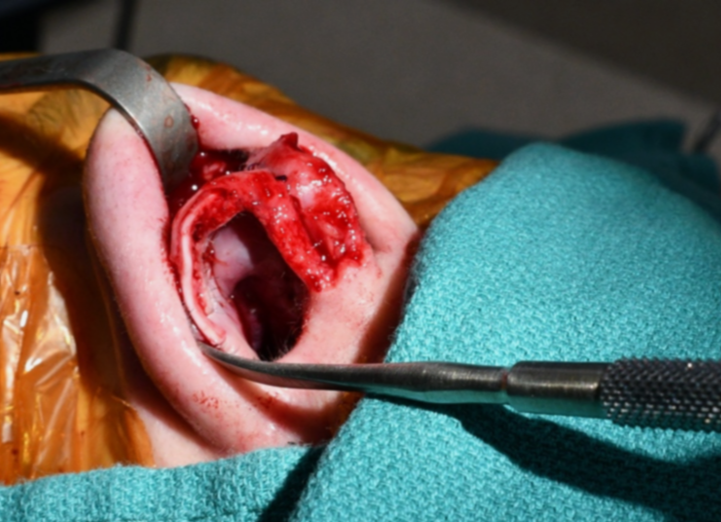
Next, a cartilage graft is fashioned and introduced into the soft tissue pocket. Either septal cartilage or auricular cartilage provides adequate thickness, bulk, and support while maintaining resiliency of the alar rim. Septal cartilage affords greater rigidity for the tip while auricular cartilage affords more curvature. Once the graft is fashioned, it is advanced into the vestibular soft tissue pocket. The graft is placed inferiorly and laterally first (Figure 3, right), followed by gentle insertion into the cephalic pocket. The final graft should be in direct contact with the LLCs just above the vestibular skin (Figure 4). Suturing the graft onto the LLC is often not necessary, due to limited dissection of vestibular skin. Finally, the incision is closed with 5-0 or 6-0 Chromic sutures. A dissolvable suture may be used to obliterate dead space between vestibular skin and the integrated graft. A video demonstration of this technique is available (see Movie 1).
Advantages of the integrated graft:
The integrated alar-lateral crural strut graft represents a marriage of two contemporary grafting techniques in rhinoplasty, and is a versatile approach for providing tip support and lateral crura support while preventing sidewall collapse. Whereas alar contour grafts provide alar rim and sidewall support and can resist notching, lateral crural strut grafts tend to be more rigid and contribute to LLC re-positioning, flattening lateral crura concavity, or improving nasal tip projection. The integrated graft described here combines these functions and is modifiable depending on size and orientation, such that alar rim graft or lateral crural strut graft characteristics may exert primary effects. Its advantages over previously described grafting methods include the ability to combine versatility of the alar rim graft with the strength and tip-defining ability of the classic lateral crural strut graft. It also decreases the amount of vestibular skin dissection and minimizes the amount of cartilage required to achieve optimal aesthetic and functional goals of surgery.
Clinical example:
We provide an example of a patient who underwent placement of the integrated alar-lateral crural strut grafts. This patient presented with a history of nasal trauma and longstanding nasal obstruction, which was more severe on the right. Her symptoms were refractory to medical therapy and she elected to proceed with surgery. Her pre-operative examination was notable for severe caudal septal deflection to the right, alar contour distortion, and external valve collapse. The patient underwent open rhinoplasty, septoplasty, placement of bilateral spreader grafts, caudal septal extension graft, and bilateral integrated alar-lateral crural strut grafts. Figure 5 shows her pre- and post- operative frontal and base view photographs, which demonstrate improvement in alar rim contour, tip support, and definition after surgery. Her pre- and post-operative oblique and profile photographs (Figure 6) demonstrate improvement in profile and enhanced sidewall support.




Conclusion:
The integrated alar-lateral crural strut graft described here combines the advantages of the traditional lateral crural strut graft and alar rim graft. In our experience, this graft is a versatile and effective alternative to traditional methods of LLC re-positioning and nasal sidewall support. This discussion highlights the role of comprehensive pre-operative planning and analysis, and emphasizes the importance of addressing LLC malposition and alar rim deformity during rhinoplasty.
References:
- Toriumi DM. New concepts in nasal tip contouring. Arch Facial Plast Surg. 2006;8(3):156-185.
- Sheen J. Aesthetic Rhinoplasty. 2nd ed. St. Louis, MO: CV Mosby; 1987.
- Constantian MB. The incompetent external nasal valve: pathophysiology and treatment in primary and secondary rhinoplasty. Plast Reconstr Surg. 1994;93(5):919-931.
- Yeh CC, Williams EF. Cosmetic and Functional Effects of Cephalic Malposition of the Lower Lateral Cartilages: A Facial Plastic Surgical Case Study. Otolaryngol Clin North Am. 2009;42(3):539-546.
- Cingi C, Muluk NB, Winkler A, et al. Nasal tip grafts. J Craniofac Surg. 2018;29(7):1914-1921.
- Constantian MB. Four common anatomic variants that predispose to unfavorable rhinoplasty results: A study based on 150 consecutive secondary rhinoplasties. Plast Reconstr Surg. 2000;105(1):316-331.
- Gunter JP, Friedman RM. Lateral crural strut graft: Technique and clinical applications in rhinoplasty. Plast Reconstr Surg. 1997;99(4):943-955.
- Toriumi DM, Asher SA. Lateral crural repositioning for treatment of cephalic malposition. Facial Plast Surg Clin North Am. 2015;23(1):55-71.
- Cochran CS, Sieber DA. Extended alar contour grafts: An evolution of the lateral crural strut graft technique in rhinoplasty. Plast Reconstr Surg. 2017;140(4):559E-567E.
- Bared A, Rashan A, Caughlin BP, Toriumi DM. Lower lateral cartilage repositioning objective analysis using 3-dimensional imaging. JAMA Facial Plast Surg. 2014;16(4):261-267.
- Emre Ilhan A, Saribas B, Caypinar B. Aesthetic and functional results of lateral crural repositioning. JAMA Facial Plast Surg. 2015;17(4):286-292.
- Unger JG, Roostaeian J, Small KH, et al. Alar Contour Grafts in Rhinoplasty: A Safe and Reproducible Way to Refine Alar Contour Aesthetics. Plast Reconstr Surg. 2016;137(1):52-61.
