Abstract
Often, rhinoplasty patients present not just for aesthetic correction, but for improvement of their nasal breathing due to functional abnormalities or problems. Because the aesthetic and functional problems must be addressed together, an understanding of both the internal and external anatomy is essential. In this article, the authors review the differential diagnosis of nasal obstruction and the important components of a thorough examination. In this article, medical treatment options are not discussed, but just as an exacting aesthetic analysis leads to an appropriate cosmetic rhinoplasty plan, a thorough functional analysis will dictate the appropriate medical or surgical treatment.
This chapter is reprinted with permission from the “Aesthetic Surgery Journal.”
When evaluating patients for rhinoplasty, it is important to assess for nasal airway obstruction. Indeed, a significant subset of rhinoplasty patients seek to improve both the aes- thetics of their nose and their nasal breathing. Typically, the functional and cosmetic portions of the procedure are addressed together. Therefore, it is critical that the rhino- plasty surgeon be armed with a knowledge of both the external and intranasal anatomy, the differential diagnosis of nasal obstruction, the elements of a complete nasal examination (including nasal endoscopy), and the medical and surgical treatment options. Although medical treatment options are not discussed in this article, just as an exacting aesthetic analysis will lead to an appropriate cosmetic rhinoplasty plan, the thorough functional analysis detailed here will dictate the appropriate medical or surgical treatment. 1
Anatomy
Anatomy of the Nasal Airway
Nasal obstruction is a symptom in which a patient feels he or she has inadequate nasal airflow. Although it is a subjective sensation, it has a foundation in objective anatomic and physiologic findings. Therefore, thorough knowledge of the nasal anatomy and physiology is a critical foundation for proper diagnosis and treatment of nasal obstruction. Selected anatomic points are highlighted here; further study is recommended.
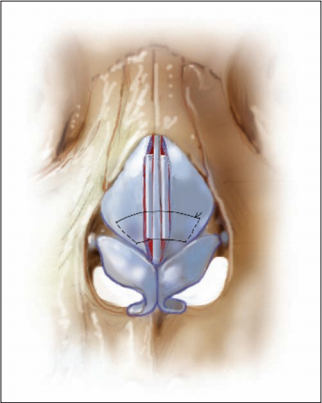
Bony Anatomy (Figure 1)
The pyriform aperture is the entrance to the nasal cavity and represents the narrowest, most anterior bony aspect of the nasal airway. Superiorly, this area is bounded by the paired nasal bones, which are attached to the frontal bone of the skull. These bones come together in the midline to form the “nasal pyramid,” which projects out from the face to form the bony nasal dorsum. 2 The nasal bones are also attached at their superolateral aspect to the lacrimal bones and inferolaterally to the ascending process of the maxilla.
The bony aspect of the nasal septum starts posteriorly at the nasal apertures or choanae, opening into the nasopharynx as the vomer (inferiorly) and the perpendicular plate of the ethmoid bone (superiorly). This bone is contiguous with the cribiform plate of the ethmoid superiorly.
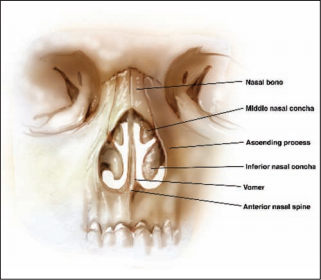
Sloping in a posterior direction from this area is the bony face of the sphenoid sinus, or rostrum. The nasal floor is made up of the nasal crest of the palatine bones and the premaxilla. This is formed embryologically when the wings of the premaxilla fuse with the vomer in the midline to form the maxillary crest (Figure 2).

The lateral nasal walls contain three pair of “scroll-like” bony shells, known as the turbinates. The superior, middle, and inferior turbinates are composed of the conchal bones, which serve as a support to the erectile tissue of the turbinates. Beneath each of these turbinates is a space called a meatus, into which the sinus cavities are able to drain.
The inferior meatus drains the nasolacrimal duct, whereas the middle meatus provides a drainage pathway to the anterior ethmoid, maxillary, and frontal sinuses. The superior meatus is the drainage area to both the posterior ethmoid sinuses and the sphenoid sinus.
Cartilaginous Anatomy (Figure 3)
The cartilaginous septum articulates with the bony portion of the septum posteriorly and the nasal crest of the maxilla inferiorly. This area, where the cartilage sits on the maxillary crest, contains densely interwoven decussating fibers of periosteum and perichondrium. The large portion of cartilage separating the two sides of the nasal cavity is termed the “quadrangular cartilage” due to its shape. Thequadrangular cartilage contains the supportive “L-strut” that is largely responsible for maintaining the strength and sup- port of the cartilaginous nasal dorsum.
The remaining cartilaginous framework of the nose consists of the paired upper lateral, lower lateral, and sesamoid cartilages. The upper lateral cartilages (ULC) are trapezoidal in shape and articulate with the nasal bones superiorly, with the nasal dorsum and dorsal septum in the midline, and loosely with the bony caudal margin of the piriform aperture. Although the inferior aspect of the ULC remains free, variable sesamoid cartilages are found in the fibrous connective tissues lateral to the ULC.
Below the ULC are the paired lower lateral cartilages (LLC). The LLC form the nasal tip and ala. The LLC can be considered in terms of a medial crura that extends superiorly and flares superolaterally as the intermediate crura and then continues superolaterally as the lateral crura. The ULC and LLC have a relationship with each other in the “scroll” region. This scroll is most commonly formed by an inward curving to the cephalic edge of the LLC, which relates to an outward-curving caudal border of the ULC.
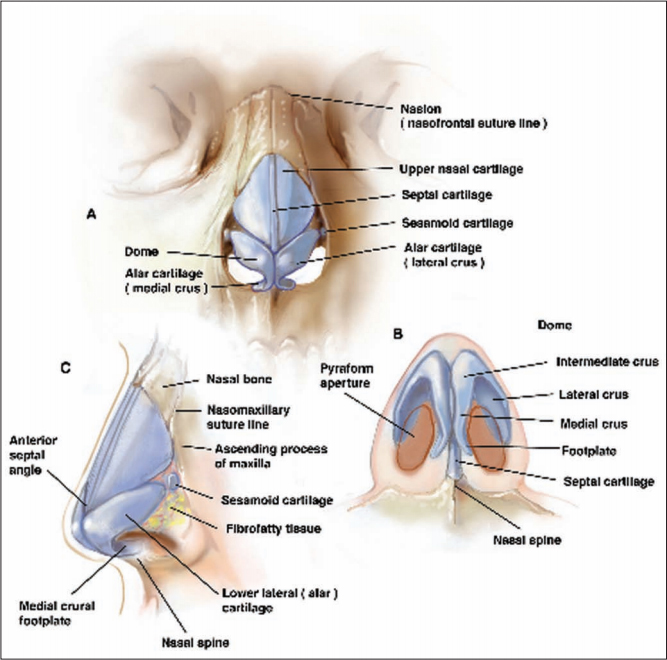
External Nasal Anatomy (Figure 4)
Aspects of external nasal analysis provide important diag- nostic evidence in the evaluation of nasal obstruction. Examples include a narrow middle vault, inverted V deformity with middle vault collapse, pinched nasal side- walls and/or pinched nostrils, narrow “slit-like” nostrils, asymmetric nostrils with evidence of a deviated caudal septum, and others. These findings will be addressed in the course of this article. The reader is directed elsewhere for detailed discussion of aesthetic anatomic analysis.

Intranasal Anatomy
An important aspect of nasal anatomy that relates to nasal airway obstruction is the area known as the external nasal valve. This has been described as the area bounded by the caudal edge of the ULC superolaterally, the nasal ala and attachment of the lateral crus laterally, the caudal septum and columella medially, and the nasal sill inferiorly. 3 This area is variable and dependent on the shape, size, and strength of the LLC.
Located just superior to the external nasal valve is the site of greatest resistance in the entire human airway, the internal nasal valve. Anatomically, the internal nasal valve is the cross-sectional area bounded superiorly by the ULC, medially by the cartilaginous nasal septum, laterally by the anterior head of the inferior turbinate, and inferiorly by the nasal floor. This valve angle is between 10 and 15 degrees in the Caucasian nose but tends to be more obtuse in ethnic African-American and Asian noses.
The cross- sectional area of the internal nasal valve is about 0.73 cm2 . 4 The physiology and function of the nasal valves will be discussed in later sections of this article.
Mucosal Anatomy
The lining of the nasal cavity is composed of a few differ- ent types of epithelium. Located at the level of the nasal vestibule is nasal skin, composed of keratinized stratified squamous epithelium, with sweat and sebaceous glands and nasal hair or vibrissae. As one moves into the nose, the lining transitions to a respiratory epithelium, com- posed of goblet cells that secrete mucin at their apical surface, basal cells, ciliated and nonciliated columnar cells, and granule cells. 5 Ciliated columnar cells are the predominant type of cell and have both cilia and microvilli to move mucus throughout the nasal cavity; these play a critical role in mucociliary clearance.
Also, different types of mucus glands (seromucous, serous, and intraepithelial) are scattered throughout the nasal airway. The sinonasal cavities produce somewhere between 1 and 2 liters of mucus each day, and the major- ity of this mucus is made by the 80,000 to 100,000 submu- cosal seromucous glands.
Finally, a specialized neuroepithelium exists in the area of the olfactory clefts and the superior portion of the nasal cav- ity. This epithelium is nonciliated and contains bipolar olfac- tory receptor neurons, their progenitor cells, sustentacular cells, and mucous glands. There are also special glands in the olfactory epithelium known as Bowman’s glands, which are believed to play an important role in olfaction.2
Blood Supply (Figure 5)
There is an abundant vascular supply to the nasal cavity. Contributions arise from the internal carotid artery (which gives off the anterior and posterior ethmoid arteries from the ophthalmic artery) and the external carotid system (which gives off branches forming the sphenopalatine, greater palatine, superior labial, and angular arteries).6
Externally, the nose is mainly supplied by the angular artery, which is a branch of the facial artery, whereas the nasal dorsum and sellar regions get their blood supply from the infraorbital artery and ophthalmic artery, respectively.
The internal nose receives its vascular supply to the lateral nasal walls posteroinferiorly from the sphenopala- tine artery, off of the internal maxillary artery, and superi- orly from the anterior and posterior ethmoid arteries. The blood supply along the nasal septum comes from the sphenopalatine artery, as well as the anterior and posterior ethmoid arteries, with contributions from the superior labial artery at the front and the greater palatine artery more posteriorly. It is important to understand the area of the septal blood supply known as Kiesselbach’s plexus or Little’s area.

This region at the anteroinferior third of the septum is a common site of anterior epistaxis and repre- sents the convergence of all three major blood supplies to the nasal cavity. (6) Veins in the nose essentially follow the arterial sup- ply, but one should take note of two very important aspects of the nasal venous drainage: these veins can communicate directly with the cavernous sinus and are valveless, possibly potentiating the intracranial spread of infection.
Innervation
The sensory nerve supply to the nasal cavity arises from the first (ophthalmic) and second (maxillary) divisions of the trigeminal nerve. The ophthalmic division (V1) gives off the nasociliary nerve, which then branches to the ante- rior ethmoid nerve, supplying the anterior lateral nasal wall. This nerve has an internal branch to innervate the anterior ethmoid and frontal sinuses and an external branch, which gives sensation to the nasal skin, from the rhinion to the tip. The posterior ethmoid nerve innervates the superior and posterior septum and lateral nasal wall. The maxillary division (V2) has an infraorbital branch, which provides sensation to the external nares, and a sphenopalatine branch, which divides into lateral and septal branches to provide sensation to the posterior and central regions of the nasal cavity.
Autonomic innervation to the nasal cavity is critical to its normal physiologic activity. The parasympathetic nerv- ous supply starts in the superior salivary nucleus in the midbrain and travels along the facial nerve to reach the greater superficial petrosal nerve, which joins fibers of the deep petrosal nerve to form the vidian nerve. These para- sympathetic fibers synapse in the sphenopalatine ganglion and send postganglionic fibers to the sinonasal mucosa. The sympathetic innervation arises in the thoracolumbar spinal cord and synapses in the superior cervical sympa- thetic ganglion before postganglionic fibers run with the vasculature to the nasal cavity.
Physiology of the Nasal Airway
The form and function of the nasal airway are intimately tied to each other. The rhinoplasty surgeon must under- stand how nasal physiology and airflow dynamics relate to the internal and external nose and how they can be affected by rhinoplasty. 2
The nose humidifies, warms, and conditions the inspired air while removing airborne particles before they reach the lower airway. This function begins with the nasal hair or vibrissae, which protect the nasal airway by filtering out large particles that enter the nasal orifice. The sinonasal mucus is critical to the process of particulate filtration. The apical surface of the respiratory epithelium is covered with cilia, and the coordinated ciliary beating from anterior to posterior in the nasal cavity sweeps par- ticles along the “mucus escalator” to the nasopharynx, where it is swallowed. This transport of trapped particles by this mucociliary clearance transport occurs about every 10 to 15 minutes in a healthy nose (about 6 mm per minute), and then it is replaced by fresh mucus. 7,8 This mucus blanket is a critical cleaning and filtering system for the upper airways and also maintains nasal moisture. 9
Humidification and warming of the inspired air occurs in part through the airflow pattern that is created by the presence of the conchal nasal bones (turbinates) and by the increased surface area of the nasal cavity. 10 By the time inspired air reaches the pharynx, the nasal cavity has the ability to raise the temperature to about 37°C and to humidify it until it is about 85% saturated. The presence of a physiologic nasal airflow pattern allows this to occur and facilitates alveolar gas exchange more efficiently in the lower airways. 4,11
Physiologic airflow in the nasal airway is also related to resistance. The resistance in the nasal airway can be divided between the nasal vestibule, internal nasal valve, and the turbinated cavity of the nasal passage. The nasal vestibule contributes only about one-third of the nasal resistance. The nasal valves comprise the major areas of resistance in the nasal cavity. 4 The internal nasal valve is the flow-limiting segment of the nasal airway and com- prises about 50% of the total airway resistance from the nasal vestibule to the alveoli. 12 Nasal resistance functions according to Poisseuille’s law, in that it is inversely propor- tional to the fourth power of the radius of the nasal pas- sages (resistance = [viscosity * length]/radius4 ). 3,13 This means that small changes in the size of the nasal valve can have exponential effects on the airflow resistance. Bernoulli’s principle also plays a key role in the physiology of the nasal valve. As the air flows across a narrowed nasal valve, velocity increases and pressure decreases. This results in negative pressure in the valve area and an increased transmural pressure difference, which can cause further “dynamic” nasal valve collapse. 14 Both the internal nasal valve and the external nasal valve function are gov- erned by these principles and they can collapse from the increased negative pressures developed from inspiration.
Additionally, the size of the nasal airway is also governed by an alternating pattern of congestion and decon- gestion, known as the nasal cycle. This phenomenon, present in about 80% of the population, occurs though the reciprocal pattern of vascular engorgement of the capillar- ies and microscopic vessels in the nasal lining and over the inferior turbinate. 9 This pattern repeats itself in the range of every two to seven hours and, as expected, the nasal resistance between the two sides of the nasal cavity also alternates throughout the day; however, both the total combined nasal resistance and nasal airflow remains rela- tively constant. 9 Additionally, many different factors can increase nasal resistance by causing the nasal mucosa to swell or become engorged. These are things such as the autonomic regulation of the nasal vasculature and nitric oxide (NO) production in the nasal cavity. 4
Nasal Obstruction
It is important that nasal obstruction in rhinoplasty patients be properly evaluated and diagnosed. Proper diagnosis is the critical first step in the correct treatment of nasal obstruction. The differential diagnosis of nasal obstruction is broad. The etiology of nasal airway obstruc- tion can be multifactorial and often contains pathology from both the anatomic and physiologic aspects of the nasal airway. 15 The more common causes are discussed here.
Anatomic Causes
Deviated Nasal Septum
Multiple studies have reported that the prevalence of a nasal septal deviation (Figure 6) is extremely common. In fact, a nondeviated septum appears to be more of the exception than the rule, as it is only present in anywhere from 7.5% to 23% of patients. 16,17 As it comprises the medial border of the nasal airway and nasal valve on each side, even small deflections in the septum can play a large role in nasal airway obstruction. Anterior septal devia- tions, often in the region of the nasal valve, may be more likely to cause the patient significant symptoms of nasal obstruction, whereas posterior deflections typically need to be larger in order to cause the patient problems. 4
Deviations of the anterior part of the quadrangular carti- lage into the mid-to-low nasal cavity are more common, but bony spurs in the region of the vomer, the perpendicu- lar plate of the ethmoid bone, or deflections of the carti- lage off of the maxillary crest also occur. 18 Additionally, it appears that anatomic problems with the septum can cause physiologic problems.
Studies have shown that a deviated nasal septum causes increased mucociliary clear- ance times compared to noses with a straight septum and that a septoplasty to repair a deviated nasal septum will return mucociliary clearance to normal. 19,20
Nasal Valve Narrowing
The internal nasal valve is the narrowest part of the nasal airway and is the site of the highest nasal resistance. Once the nasal valve has been determined to be the source of obstruction, it is important to assess whether this is a static or dynamic problem. Although static obstructions require a physical alteration in the anatomy, a dynamic problem usually focuses on adding support to a deficiency of the cartilages or soft tissues. 10
Regarding the internal nasal valve, a static obstruction can be seen from abnormalities in the anatomic bounda- ries of the valve, such as inferior turbinate hypertrophy or a deviated nasal septum. Also, there can be displacement of the lateral wall of the nasal valve from trauma, as well as scars in the intercartilaginous region, pyriform aperture stenosis, or ULC that are disarticulated and fall into the nose, obstructing the airway. Schlosser and Park21 asserted that when the nasal bones are deviated or displaced, no nasal valve grafting repair will be sufficient without addressing the nasal pyramid due to the relationship between the nasal bones and the ULC.
On the other hand, a dynamic problem that involves the internal nasal valve usually involves a collapse of the lateral nasal sidewall due to a destabilization of the LLC or nasal septum. 3 If these structures are disrupted and not refixated, they no longer have the stability to support the ULC, leading to collapse. Sheen22 observed that a patient with an overprojected nose, a narrow middle vault, and short nasal bones represents a “narrow nose syndrome.” This situation presents a higher risk for internal nasal valve narrowing after resection of the middle vault roof. This can result in an inferomedial collapse of the ULC into the airway. 10 Spreader grafts are required in this setting.
Regarding the external nasal valve, some of the more common causes of a static narrowing include alar base malpositioning, postoperative scarring in the valve area or nasal vestibule, caudal septal deflections, or nasal tip pto- sis. 3 Furthermore, a dynamic collapse or obstruction in this area can be due to a weak or deficient LLC and nasal ala or even dysfunction of the nasal and facial muscles that help to dilate this area and keep it from collapsing. The former is often a result of deficiency of the LLC from an overresection of the lateral crura or due to anatomically vertically positioned LLC, known as the “parenthesis deformity.”23 In these situations, the cartilages are not able to adequately support the alar margin. Also, tip ptosis can occur from a bulky excess of nasal tip soft tissue, leading to obstruction of the nasal vestibule. 3 As mentioned above, patients with facial paralysis also frequently have external nasal valve collapse because of the denervation of the nasalis and dilator nasi muscles. The muscular tone is no longer present in this case to support the sidewall of the nose.
Middle Turbinate Concha Bullosa
Because a majority of airflow through the nose enters the middle meatus, obstruction at this level must be addressed. A pneumatized middle turbinate, or concha bullosa (Figure 7), is a very common anatomic variation of the middle meatus and nasal airway, occurring in about 25% of the population. Although most concha bullosa are asymp- tomatic, large concha can be attributed to nasal obstruction.
Furthermore, there is a correlation between a unilateral concha bullosa and a septal deviation to the contralateral side. This is caused from the pneumatizedmiddle turbinate pushing the septum across to the other side as it develops. Almost 80% of patients with a large unilateral concha bullosa have an associated septal deviation. 15
Inferior Turbinate Hypertrophy
The inferior turbinate has a number of important functions, including airflow warming, humidification, filtra- tion, and mucociliary clearance. However, pathologically enlarged turbinates can also play a significant role in nasal airway obstruction. With the head of the inferior turbinate comprising the lateral boundary of the nasal valve, enlarge- ment can cause narrowing of the internal nasal valve. Different variations in inferior turbinate hypertrophy have been described, ranging from bony to soft tissue to mixed. 18
Although bony abnormalities of the inferior turbinates are often treated with surgical procedures such as outfracture and partial turbinectomy, soft tissue or mucosal hypertrophy can be addressed first with topical and sys0temic medications to control the engorged inflammation of the overlying nasal mucosa and then, when indicated, with submucous resection or radiofrequency. These therapies will be discussed later in the article.
Choanal Atresia
Choanal atresia refers to obstruction of the posterior nasal apertures. This abnormality is most commonly congenital and can be unilateral or bilateral, with an incidence in the range of 1 in 5000 to 7000 live births. 24 The choanal obstruction can be bony, membranous, or mixed; the bony entity is by far the most common, occurring in about 90% of cases.
25 The presence of choanal atresia can be an iso- lated occurrence, but it is usually associated with other congenital anomalies (in over 50% of cases). Most com- monly, this cause of nasal airway obstruction is associated with CHARGE syndrome (coloboma, heart defects, cho- anal atresia, growth or developmental retardation, geni- tourinary hypoplasia, and ear anomalies). 18,26 Although generally identified in the pediatric population, unilateral choanal atresia or stenosis is occasionally encountered in the adult population.
Pyriform Aperture Stenosis
The bony pyriform aperture is the narrowest and most ante- rior portion of the bony nasal airway. Stenosis of this por- tion of the airway usually results from a bony overgrowth of the nasal process of the maxilla. As a cause of nasal obstruction, this process was first described by Brown et al 27 in 1989. This study determined that the pyriform aperture is stenotic when the maximum transverse diame- ter is less than or equal to 3 mm. It is important to remem- ber that patients with a narrow or relatively hypoplastic midface may be at risk for pyriform aperture stenosis. 28
Trauma and Previous Sinonasal Surgery
Many complications from both accidental and iatrogenic trauma can lead to patient problems with nasal airway obstruction. These anatomic problems—such as nasal septal fractures, adhesions in the nasal cavity, septal per- forations, and scarring of the nasal valve—can block the airflow through the nose and cause the patient significant symptomatology. 15 Additionally, previous trauma and rhi- noplasty surgery are the most common causes of a weak- ened nasal valve and increased nasal airway resistance. 15 Paradoxically, overresection of the nasal turbinates can leave the patient with a feeling of nasal obstruction. This phenomenon, known as “empty nose syndrome,” disrupts the physiologic ability of the nasal airway to warm and humidify the inspired air through the lack of the previ- ously resected turbinate mucosa (Figure 8). 29
Physiologic Causes
Sinonasal Inflammatory Diseases
Diseases of the sinonasal mucosa are extremely common and one of the most prevalent symptoms that results is nasal obstruction. Inflammation of the nasal mucosa is clearly a multifactorial process and it is believed that an increased local blood flow in the area, in response to the inflammation, is a cause for the edema and congestion of the nasal tissue.
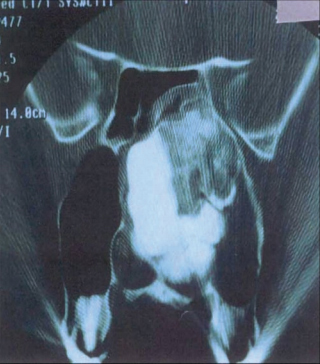
Nasal polyposis, often felt to be triggered by a combination of factors (including rhinosinusitis, asthma, and allergy), may be large enough to obstructthe nasal airway and the sinus ostium, resulting in sinus infections and the inability for the nasal mucus to drain (Figure 9). Although a discussion of sinusitis and other rhinologic diseases is beyond the scope of this article, it should be noted that nasal obstruction plays a key role in the symptomatology of these patients and their quality of life. 30
In addition, atypical inflammatory diseases must be kept in the surgeon’s mind, as nasal obstruction can be caused by lesions such as Wegener’s granulomatosis, sarcoidosis, rhinoscleroma, rhinosporidosis, and tuberculosis, to name a few. These processes can all contribute to the formation of lesions, crusting, ulcerations, and irritations in the nasal cavity, causing patients to have symptoms of obstruction. 15

Neoplasm
All sinonasal neoplasms can present as nasal obstruction and this symptom continues to be the most common com- plaint that triggers evaluation. It is often accompanied by epistaxis; other vague problems such as facial pain, pres- sure, and anosmia may trigger a rhinoplasty surgeon to perform a nasal endoscopy or to refer the patient for evaluation by an otorhinolaryngologist for a thorough nasal endoscopy and possible computed tomography (CT) scan, if indicated.
Although squamous cell carcinoma remains the most common malignancy of the sinonasal cavity, other benign tumors or lesions such as inverted papillomas, antral-coanal polyps, and osteomas may also be seen (Figure 10). 31
Medical/Hormonal Changes
Many medications, both prescription and over-the-counter, can lead to significant problems with nasal airway obstruction. It is critical to ask patients about their use of nasal decongest- ant medications. Patients often reach for an over-the-counter solution without seeking medical help for their nasal obstruction, but overuse of medications in both the imidazoline class (ie, oxymetazoline) and sympathomimetic amines (ie, ephe- drine and phenylephrine) can cause significant problems with nasal obstruction. Prolonged ingestion of these medica- tions can lead to a process called rhinitis medicamentosa and a phenomenon known as “rebound nasal congestion.” After more than three days of intranasal application, these patients will complain that they have even more rhinorrhea and nasal congestion than before they started the medication. Studies have shown that this condition results in a disruption of the mucociliary clearance from the ciliated epithelial cells being destroyed, as well as a subsequent increase in the vascular permeability and edema of the nasal mucosa. 32 In addition to these topical nasal medications, some systemic medications such as antihypertensives (ie, hydralazine), methyldopa, beta-blockers (ie, propranolol), antidepressants, and even antipsychotic medications can cause nasal obstruction.
Also, it is important to note that medical problems such as hypothyroidism and the hormonal changes that accom- pany pregnancy have been shown to cause rhinitis and nasal obstruction. Neither mechanism for these processes has been well elucidated, but it has been considered a vascular dilation of the nasal mucosa in the case of hypothyroidism and a combination of a direct effect of the woman’s hormones along with a generalized increase in the interstitial fluid volume from pregnancy that cause the mucosal edema and nasal obstruction. 15
Evaluation Of Nasal Airway Obstruction
A patient reporting significant nasal obstruction should have a thorough evaluation. This starts with the history and physical examination (including nasal endoscopy), and then can progress to more extensive assessment, such as radiologic exams and even objective tests or measures of the nasal airway and its obstruction.
History and Physical
In the patient with nasal obstruction, a thorough history should address the presence of nasal obstruction, sinusitis, rhinitis, inflammatory sinonasal disease, postnasal drip, chronic cough, facial pain or pressure, ear pain or pressure, loss of sense of smell or taste, hearing loss, or other pertinent findings. 33 A history of environmental or seasonal allergies must be obtained and any prior nasal surgery must be noted, including sinus surgery, rhinoplasty, septoplasty, turbinate reduction, or other procedures. A history of prior nasal trauma should also be identified.
The rhinoplasty surgeon must also investigate the specific aesthetic concerns the patient may have with his or her nose. Some procedures, such as narrowing the external appearance of the nose, may have an internal effect on the nasal airway. Additional history—specifically, the patient’s medication history, including the use of aspi- rin, aspirin-containing products, anticoagulant medica- tions, nonsteroidal anti-inflammatory drugs (NSAID), and herbal supplements that may increase the bleeding risk during the case—should be noted. The patient must be questioned about continued use of intranasal topical decongestants to rule out rhinitis medicamentosa. A good social history should be obtained to determine the patient’s smoking habits, for reasons of wound healing. A history of intranasal cocaine should be identified, as this may lead to significant preoperative and postoperative issues. 33
A thorough physical examination of the head and neck is the next step in the evaluation of the patient. An exhaustive discussion cannot be undertaken here. However, with regard to the nasal airway, complete external and internal nasal examination must be undertaken. Externally, the rhinoplasty surgeon must take note of a patient with a narrow middle vault and short nasal bones, the so-called narrow nose syndrome patient, as he or she is at increased risk of middle vault collapse and internal valve narrowing if this is not recognized preoperatively and appropriately addressed intraoperatively. 10,22,33 Also, the external nasal exam may show the patient experienc- ing alar collapse or supra-alar pinching on inspiration, designating either external or internal nasal valve collapse. Facial nerve function also should be assessed to determine whether there is any asymmetry of the facial function or collapse of the external nasal valve from nasalis or dilator nasi muscle dysfunction.

Internally, anterior rhinoscopy should be performed to visualize the inferior turbinates, caudal nasal airway, and external nasal valve. A nasal speculum and a headlight can assist in identifying any anterior nasal pathology; however, this view is generally limited to the anterior nasal airway. The Cottle maneuver is helpful in assessing the nasal valve. 15 This maneuver is classically described as retracting the cheek skin and lateral nostril while pulling the ULC away from the septum to open a larger nasal valve area. 3,15,33 The physician may create false-positive results with this test unless the lateralization of the nasal sidewall is performed realistically. 33 Many authors, includ- ing Constantinides et al, 34 have described a modification of the Cottle maneuver. They describe placing a small ear curette under the LLC and the ULC, both before and after decongestion and topical anesthesia. The airway patency is assessed with the curette, gently elevating the nasal cartilages one at a time in order for the patient to experi- ence what it would be like to have these areas reinforced with surgical grafting techniques. Nasal airflow improve- ment with ULC support would suggest internal nasal valve pathology, whereas improvement with LLC support would signify that an external nasal valve problem may be involved. 3,34 Another anterior rhinoscopic exam should also be repeated once both topical anesthetic and a decon- gestant are applied to the nose. This may facilitate precise localization of the site of nasal obstruction.
Diagnostic nasal endoscopy allows a more thorough examination of the nasal airway (Figure 11). This endos- copy, whether flexible or rigid, should include evaluation of the septum, turbinates, nasal mucosa, nasal valve, and other nasal structures. Again, assessment before and after decongestion is advised, as improvement or relief of air- way obstruction after the administration of decongestion alone may point to some other type of nasal pathology, such as a sinonasal mucosal inflammatory disorder. 35
It is advisable to perform a diagnostic nasal endoscopy following initial anterior rhinoscopy, as recommended by Lanfranchi et al. 36 According to their study, additional surgi- cal therapy to relieve nasal obstruction was undertaken in 28 of the 95 patients (29%) because of significant pathologic findings on nasal endoscopy. The authors advise perform- ance of nasal endoscopy on all patients who present for a septorhinoplasty when they report nasal airway obstruction.
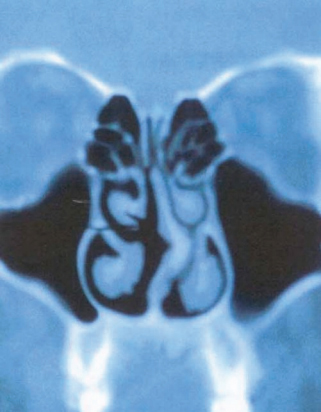
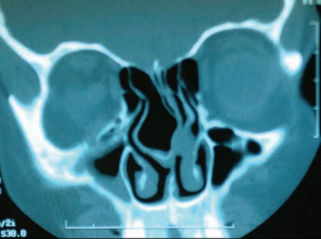
Radiologic Exams
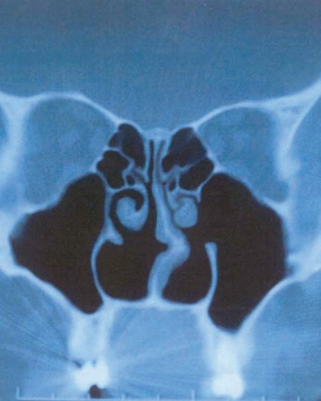
Some radiologic studies may assist with the diagnosis when the site(s) or source(s) of nasal obstruction cannot be identified with a history and physical exam (Figure 12). In these cases, a coronal sinus CT scan can assist in iden- tifying sources of nasal obstruction, such as a concha bullosa or posterior septal deviation, which may not have been appreciated on physical exam. Additionally, a coronal sinus CT may provide additional information for a patient who has had a history of chronic nasal obstruc- tion or sinonasal inflammatory disease. This added infor- mation may alert the surgeon to additional pathology and may ultimately lead to an alteration of the surgical plan. 15,33

Objective Nasal Airway Studies
Rhinomanometry
The rhinomanometer is a device that functionally meas- ures nasal airflow at a fixed pressure differential during the nasal respiratory cycle. This provides a method with which the rhinoplasty surgeon can quantitatively measure nasal resistance. With this technique, a pressure-flow curve is generated that will show a higher nasal resistance and less nasal airflow in a more obstructed nose. The most common method is called anterior rhinomanometry and was introduced by Coutade in 1902. 37 The transnasal pres- sures are generated from a nostril transducer and each nostril is measured separately, making total nasal airway resistance only calculable from formulations. Another limitation is that this technology does not accurately work on patients who have septal perforations.
A rhinomanometry study was performed by Constantian and Clardy, 38 who examined postrhinoplasty nasal obstruc- tion. In their study, external and internal valve reconstruc- tive surgery improved nasal airflow by 2.6 and 2.0 times, respectively, and improved airflow 3.8 times when they were combined. Also, the addition of a septoplasty to internal and external nasal valve surgery improved airflow by 4.9 times. Even in patients who had undergone previ- ous septoplasty, 91% had their nasal obstruction corrected with nasal valve surgery, highlighting the importance of internal and external nasal valves in nasal airway surgery. Although rhinomanometry does give an objective measure of nasal resistance (or how difficult it is for the patient to breathe), some authors have not found it to be useful because, in their experience, the quantitative findings fre- quently do not correlate with the patients’ subjective assessments of nasal patency. 39-41
Acoustic Rhinometry
Acoustic rhinometry has also been employed as a way to objectively measure nasal airway obstruction and nasal airflow. Acoustic rhinometry was first introduced to calcu- late the cross-sectional area of the nasal airway in 1989 by Hilberg et al. 42 They described how the volumes of the nasal passages could be calculated through contiguous cross-sectional areas. Acoustic rhinometry works by prop- agating a sound wave through the nasal cavity. The sound wave is reflected back to create a rhinogram, showing a two-dimensional representation of the nasal airway. 43 Acoustic rhinometry is a complementary study to rhi- nomanometry, in that it assists in measuring the location of the nasal obstruction, not in determining total nasal resistance. Interestingly, acoustic rhinometry has been deemed the most accurate measurement of nasal area, especially anterior in the nose and the region of the nasal valve. 44 Perhaps for this reason, acoustic rhinometry is the most utilized method of measuring nasal airway patency in both clinical and research settings. 15 Acoustic rhinom- etry has been useful in quantifying and comparing postop- erative changes in the cross-sectional area of the nasal airway after rhinoplasty. 45 In a study by Friedman et al, 46 the authors demonstrated how acoustic rhinometry can be a tool for assessing the effects of specific surgical tech- niques on the nasal valve area.
Surgical Procedures to Open the Nasal Airway
Nasal Septal Surgery
The various approaches to septal surgery have specific historical origins, and subsequently numerous modifica- tions and variations exist and have been described. A partial overview is provided here.
Submucous Resection
The history of submucous resection (SMR) dates back to techniques described by Killian and Freer, who discussed elevating mucopericondrial flaps on either side of the nasal septum and resecting the intervening quadrangular septal cartilage, leaving the overlying mucosa intact. 47 Bony septal spurs or deviations are also removed with the majority of the cartilage. A critical portion of this opera- tion involves leaving an adequate 10- to 15-mm strut of cartilage both dorsally (to prevent collapse or a saddle nose deformity) and caudally (to provide support against columellar collapse and a subsequent nasal tip ptosis). 47 Once the offending deviation to the septum has been removed, the flaps are then reapproximated, and the inci- sion is closed anteriorly. The large empty space that is left between the mucosal flaps in this classically described technique requires attention. The placement of quilting sutures, silastic septal splints, and nasal packing are among the techniques described to prevent fluid accumu- lation between the flaps.
Traditional Septoplasty
What we commonly think of as the traditional septoplasty is similar to the SMR, but is a more conservative proce- dure that removes less cartilage and aims to specifically target the area of the septal deviation. There are multiple small differences between a traditional septoplasty opera- tion and the SMR. A notable difference is that with the tradi- tional septoplasty, the cartilage that is removed may be morselized or otherwise straightened and then replaced back between the septal flaps. Also, cartilage modifica- tions to score and weaken the septal cartilage can be per- formed to straighten the deflection while maintaining septal strength. 47 Some authors, however, have suggested that these cartilage modifications and replacements can lead to recurrent deviations from cartilage memory
Endoscopic Septoplasty
The endoscopically guided septoplasty is a technique that can be particularly useful for cases involving revision sur- gery, as well as for addressing focal septal deflections or spurs (Figure 12). Some surgeons have advocated the use of the endoscopic septoplasty for patients with densely adherent septal mucosal flaps, such as those found in revi- sion septoplasty. Especially in cases of prior septoplasty, septal hematoma, or abscess—where there is a significant loss of the septal cartilage with subsequent scarring of the septal flaps to one another—endoscopic assistance helps the surgeon to elevate these flaps with partially obliterated dissection planes or bypass densely adherent flaps and directly address the persisting deviation. 1 Additionally, the endoscopic septoplasty has been a useful approach when attempting to address isolated posterior septal spurs or deflections, where it is often unnecessary to raise large septal flaps or to make incisions in the mucosa at the anterior aspect of the nose.
Open Septoplasty
At times, the nasal septal deformity is such that endonasal approaches may not be adequate to fully address the deformity. In these situations, addressing the septum through an open rhinoplasty approach may be preferred. This procedure first involves “opening” the nose through an external rhinoplasty approach. Once the nose has been degloved and the underlying anatomy exposed, the sep- tum can then be addressed from both a dorsal and caudal direction.
The open rhinoplasty approach for severe cases requir- ing an extracorporeal septoplasty warrants mention. This procedure may be indicated for patients in whom both the septum and the external nose are severely deviated. In order to straighten the nose in addition to both the caudal and dorsal aspects of the septum, the cartilaginous septum is removed, repaired, and then reimplanted. The septum can be removed by separating the dorsal septum from the bilateral ULC, after which it is fractured off the pre- maxilla inferiorly and the bony septum posteriorly. Once the septum is removed from the nose, it can be reworked, straightened, and grafted before it is replaced and secured. Gubisch, 48 in his report of 2119 patients undergoing extra- corporeal septoplasty, described how he secured the replaced septum to the nasal spine and ULC with sutures for maximum support.
A report by Most 49 details a useful modification to the extracorporeal septoplasty that he has termed the “ante- rior septal reconstruction.” In this case, a dorsal cartilagi- nous strut is maintained to anchor the reimplanted septum and retain the normal dorsal nasal contour. Most explains that by not securing the reimplanted septum to the “key- stone area” where the septum and nasal bones meet, any dorsal saddling or irregularities from accidental disruption of this point are avoided. 49
Caudal Septal Deflections
Caudal septal deflections (as seen with the patient in Figure 13) can be specific challenges to septal surgery because they can often cause persistent nasal obstruction and may require complex septal reconstructions. 50,51 Simply resecting the caudal septal cartilage would clearly violate the inverted L-strut that is providing tip and colu- mellar support. 47 The simplest technique (and often the first attempt to correct this problem) involves vertically scoring or incising the caudal septal cartilage on the con- cave side in an attempt to remove the “spring” memory from that portion of the septum. 1,50
Another method to correct a deviated caudal septum is the “swinging door” technique, originally described by Metzenbaum. 52 In this technique, the septum is treated as in a standard septoplasty and then raised out of its maxillary crest groove with an elevator, like a Cottle. The wedge of cartilage along the maxillary crest is then excised. At this point, the caudal edge of the cartilage is freed from the anterior nasal spine and caudal attachments and is now only attached superiorly.
This single attachment then allows the cartilage to swing into a more midline or straight position, where it can be secured with a suture to the nasal spine. 47,52 Pastorek and Becker 50 later modified this method and termed it the “doorstop technique.” In this modification, the cartilage that is dissected out of the maxillary crest is not resected but is instead flipped to the side of the nasal spine, opposite the obstruction, and secured with a suture. In this method, the nasal spine acts as a “doorstop” to prevent the caudal septum from return- ing to the other side.
An additional way to straighten the caudal septum is through the placement of an ethmoid bone splinting graft. As described by Metzinger et al, 51 a straight piece of the perpendicular plate may be harvested and small holes are then drilled in the bone with a hand drill. A Keith needle then secures the bony splint to the caudal septal cartilage, which may be straightened first by scoring. It should be noted, however, that the ethmoid bone, when secured in place at this location, can cause the caudal septum to thicken. The surgeon should be sure that the additional piece of bone does not itself cause nasal obstruction when it is secured. 1
At times, excision and replacement of the caudal septum may be necessary. An external rhinoplasty approach facilitates this technique.
Turbinate Surgery
The management choices in turbinate surgery have been extremely controversial. Although some advocate turbi- nectomy as the treatment of choice for nasal obstruction, others explain the physiologic importance of the turbinates and strongly suggest a more conservative approach to save the turbinate mucosa.
Radiofrequency Turbinate Reduction
With radiofrequency volumetric tissue reduction (RFVTR), a needle on the handpiece of the RF device is inserted into the hypertrophied turbinate mucosal tissue and radiofre- quency energy is emitted to ablate the tissue. 53 Unlike in electrocautery or laser reduction, which can cause crust- ing or damage to the overlying mucosa, the mucosal injury is significantly reduced because the needle is inserted into the submucosa; the temperatures remain much lower than with either laser or submucous dithermy treatment because of minimal heat dissipation. 54,55 Cavaliere et al 56 looked at long-term follow-up after RFVTR of the inferior turbinates and reported that RFVTR improved nasal volumes and nasal airway resistance by acoustic rhinometry and also by a subjective decrease in nasal obstruction. The results of this procedure may not be permanent and may need to be repeated. Radiofrequency reduction can be performed under local anesthesia.
Electrocautery
Electrocautery of the inferior turbinates has ranged from monopolar and bipolar surface electrocautery to submucous dithermy. Although this treatment has definitely been shown to decrease the size of the inferior turbinates, there have been some associated problems. The results of this procedure may not be permanent and may need to be repeated. Meredith57 reported that 31% of patients who underwent outfracture and electrocautery of the inferior turbinates had recurrent nasal obstruction when followed for longer than 33 months. Also, there appears to be an increased amount of postoperative crusting, edema, and scarring associated with this procedure that may persist as long as six weeks after treatment. 57
Laser Cautery
Various lasers, ranging from the KTP to the carbon dioxide (CO2), have been employed to reduce the mucosa overly- ing the inferior turbinates. They originally gained popular- ity because of the surgeon’s ability to perform this procedure in the office under local anesthesia, with mini- mal postoperative pain or bleeding. 54 Although the laser is an effective technique for reducing the hypertrophied tur- binate mucosa, patients with bony turbinate hypertrophy will not receive benefit from this procedure. In a study looking at the use of the laser versus submucous dithermy, nasal patency appeared to be about the same at six weeks, but only the laser group showed continued reduction in subjective nasal obstruction at the one-year point. 58
Cryotherapy
Cryotherapy reduces the turbinate mucosa and can be performed under local anesthesia. This method utilizes a cryroprobe that is placed into the turbinate mucosa. Freezing is induced in order to shrink the hypertrophied turbinate. Cryotherapy has low morbidity as a procedure, but the reported results are temporary and inconsistent. 59
Submucous Resection
A critical aspect of inferior turbinate reduction is leaving the adequate mucosa intact. A submucous resection removes the erectile submucosa and the underlying conchal bone that can be attributed to enlargement. This technique is practical specifically in cases where significant nasal obstruc- tion is caused by the bony portion of the inferior turbinate.
The application of microdebrider technology was a sig- nificant advance in the treatment of inferior turbinate hypertrophy and related nasal airway obstruction. Through a small stab incision at the head of the inferior turbinate, the microdebrider turbinate blade (Xomed Medtronic, Jacksonville, Florida) bluntly dissects on a submucosal plane to excise the erectile soft tissues and conchal bone of the inferior turbinate. The turbinate is then outfrac- tured, if indicated. In a study performed by Chen et al, 60 the microdebrider-assisted submucous resection was suc- cessful in reducing subjective complaints, including snor- ing, rhinorrhea, and nasal obstruction at one, two, and three years postoperatively, as well as significantly improv- ing rhinomanometric values from preoperative evaluation.
Total Inferior Turbinectomy/Partial Inferior Turbinectomy
Total or partial inferior turbinectomy is not a uniformly accepted approach for the treatment of a patient with nasal obstruction and enlarged inferior turbinates. This technique involves fracturing the inferior turbinates toward the mid- line and truncating the turbinate at its lateral attachment. A portion of these patients may suffer with postoperative crusting, nasal dryness, bleeding, and even atrophic rhini- tis. 54 Passali et al 61 undertook a study in 2003, looking at 382 patients with symptomatic inferior turbinate hypertro- phy who were randomized into six different therapeutic groups. The results of the study showed that those patients who received total or near-total turbinectomy had long- term relief of nasal airway obstruction but had a signifi- cantly higher percentage of crusting and bleeding compared to other types of inferior turbinate reduction. It is important for the rhinoplasty surgeon to realize that even though infe- rior turbinectomy may decrease nasal resistance and widen the nasal airway, it may do so at the cost of a disturbance in the nasal airflow and physiology.
Middle Turbinate Surgery
Due to its critical location in the internal nasal valve area, the inferior turbinate appears to receive most of the attention when a surgeon talks about the turbinates and nasal airway obstruction. The middle turbinate is smaller than the inferior turbinate, accounts for an extremely small portion of the nasal airway resistance, and contains less erectile tissue capable of engorgement. 54 Even with all this information, it is extremely important not to forget about the middle turbinate, as this can be a source of nasal obstruction that is often missed.
Middle turbinate resection/partial resection. Although some surgeons routinely resect the entire middle turbinate for access in sinonasal surgery, many advocate for its preserva- tion and its important role in the physiologic functioning of the nasal cavity. This has been a hotly debated topic in the sinus surgery community, and a consensus as to what is the correct treatment of the middle turbinate remains undecided. As a general rule, sacrifice of the entire middle turbinate is rarely performed for treatment of routine nasal obstruction. Partial resection of the middle turbinate, however, can signifi- cantly improve a patient’s nasal airflow if the turbinate hypertrophies and blocks the nasal passage posterior to the internal nasal valve. 62
Concha bullosa. In addition to a hypertrophy of the middle turbinate or a septum that is pushing the middle turbinate into the nasal airway, the middle turbinate can be pneuma- tized, known as a concha bullosa, and cause significant nasal obstruction. Kennedy and Sinreich63 elucidated an effective method for treating a concha bullosa that leaves most of the middle turbinate intact and able to perform its normal functions. In this technique, the middle turbinate head is split down the middle, and only the lateral portion is resected, in order to open the airway and relieve this obstruction.
Nasal Valve Surgery
Although some of the procedures described above, such as septoplasty and inferior turbinate reduction, will widen the nasal valve area, we will now focus on rhinoplasty techniques that open the nasal valve.
Internal Nasal Valve Surgery
Spreader grafts. In 1984, Sheen22 introduced spreader grafts to widen the nasal valve area and prevent nasal valve collapse (Figure 14). He described a thin (1- to 2-mm wide) rectangu- lar bar of autologous cartilage that is placed in a submucosal pocket, situated between the septal cartilage and ULC and secured with horizontal mattress sutures. This cartilage should run the length of the ULC, from their insertion just beneath the nasal bones superiorly to the caudal end of the nasal septum. This effectively widens the nasal valve area and improves the nasal airflow by lateralizing the ULC. Cosmeti- cally, the placement of spreader grafts after hump reduction is employed to maintain the appropriate width of the middle vault and avoid an inverted-V deformity. Functionally, spreader grafts appear to be most effective with a narrowed middle nasal vault that needs to be widened. In an interesting cadaveric study by Schlosser and Park, 21 the authors found that spreader grafts, probably the most common treatment for internal nasal valve collapse, represented the smallest quanti- tative improvement in the cross-sectional area of the internal nasal valve with acoustic rhinometry. Another study by Zijlker and Quaedvlieg64 looking at airflow showed that just placing bilateral spreader grafts improved nasal patency in their patients by 81%.
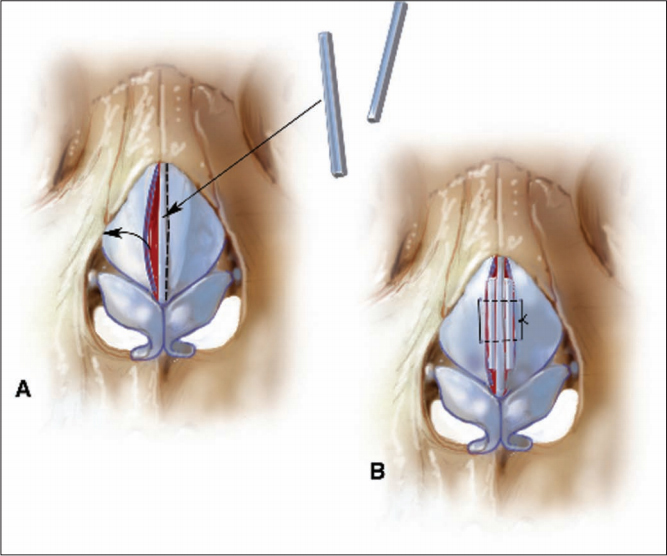
Flaring sutures. Another technique that can be utilized to widen the internal nasal valve area is the placement of verti- cal mattress flaring sutures, or “Park sutures”10 (Figure 15). These sutures are placed at the lower border of one ULC, extended over the top of the nasal dorsum, and then secured to the lower border of the ULC on the opposite side. As this suture is gently tightened, the dorsal septum acts as a pivot point, and the lateral ends of the ULC begin to flare and widen the internal nasal valve. 10 This method is especially beneficial in those patients with more vertically oriented ULC. In the cadaveric study performed by Schlosser and Park, 21 flaring sutures alone improved the cross-sectional nasal valve area by 9.1% and the placement of flaring sutures in combination with spreader grafts increased the valve area significantly, by 18.7%. Both flaring sutures and spreader grafts together also significantly improved mean nasal patency scores in the patient arm of the study.
Suspension sutures. An alternative technique that attempts to suspend the nasal valve with a suture anchored to the orbital rim was first introduced by Paniello65 in 1996. This suture is placed through a lower eyelid transconjunctival approach and sutured to the ULC, or passed through the nasal mucosa in the nasal valve area just cephalad and then back caudally, essentially cradling the region of the nasal valve col- lapse. This suture is then secured back to the periosteum of the orbital rim. This procedure has since been modified by surgeons utilizing a bone-anchored system46,66,67 and by another surgeon who passes the suture medial and lateral to the ULC and then secures the suture to the periosteum over the nasal bones. 68
Splay grafts. In 1998, Guyuron et al 69 first discussed the placement of a ULC splay graft to open the nasal valve. In their technique, a piece of conchal cartilage is placed concave side down over the dorsal septum and in a pocket underneath each ULC, in an attempt to reconstruct the middle vault of the nose. The dorsal nasal septum then becomes a fulcum for the conchal cartilage and the lateral aspects support and “splay” the ULC apart, widening the nasal valve. Similarly, modifica- tions of this technique have been attempted and described as butterfly grafts.
Butterfly grafts. Another graft technique that can be utilized to widen the internal nasal valve area is the butterfly graft. This is most commonly a piece of conchal cartilage that is harvested and placed to span the nasal dorsum, with the nat- ural concave surface pointing down toward the nasal cartilages. 70 The placement of these grafts can be via an open or endonasal approach, and they are secured into position between the LLC and ULC. To widen the nasal valve, the caudal edge of the butterfly graft is placed underneath the cephalic edge of the LLC to support it. A modification of this graft has been developed that employs septal cartilage, which is longitudinally striated, allowing it to bend; it is sutured over the top of the nasal dorsum. 3 The graft then acts as a modified flaring suture when it is secured to the underlying ULC on each side of the nose. Additionally, Stucker and Hoasjoe71 and Stucker et al 72 described the placement of a conchal cartilage onlay graft over the ULC with excellent outcomes. More recently, authors have also employed alloplastic materials to mimic a butterfly graft. One example of this is the Monarch implant, made of an expanded polytetrafluoroethylene (PTFE) package around an adjustable titanium center. This malleable implant is now approved by the Food and Drug Administra- tion (FDA) for the treatment of nasal valve dysfunction. A study by Hurbis73 in 2008 showed no adverse effects from the implant and an improved nasal valve area at one and six months postoperatively, according to acoustic rhinometry. The surgeon should be aware that there is always a greater risk of infection or extrusion of alloplastic versus autogenous grafts and that long-term data on this implant have not been evaluated.
Z-plasty. Scarring of the internal nasal valve area—usually of iatrogenic origin from previous rhinoplasty, nasal surgery, or otherwise—can cause a significant narrowing of the nasal valve area. Recently, surgeons have been employing small intranasal Z-plasties to widen the scarred area. This method relies on small, triangularly based flaps, which are elevated and sewn open in a transposed orientation. This rearrange- ment of the nasal valve mucosa allows that area to lengthen, open, and heal back without a contractile scar. In a study by Dutton and Neidich74 in 2008, all of the 12 patients who had intranasal z-plasty to correct nasal valve scarring appeared to have a larger nasal valve area postoperatively on nasal endos- copy and also subjectively reported improvement of nasal airway obstruction.
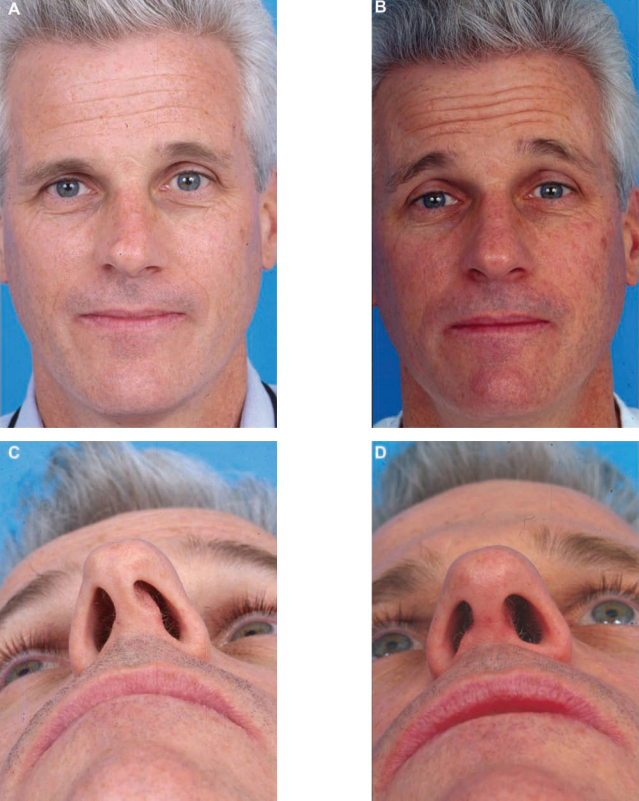
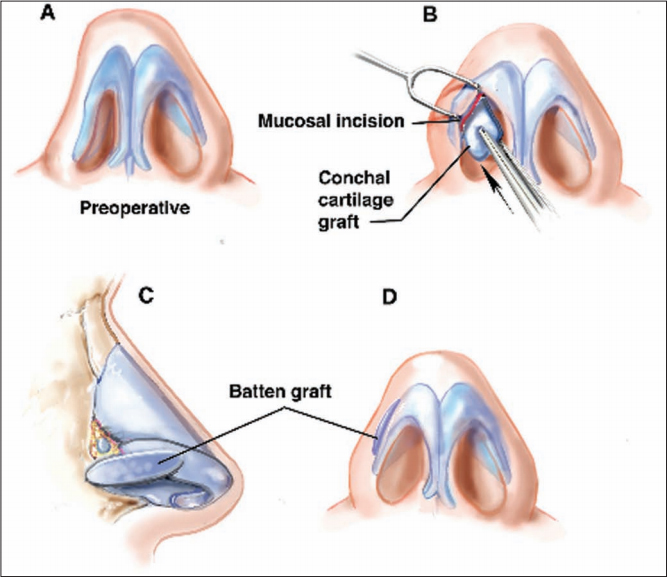
External Nasal Valve Surgery
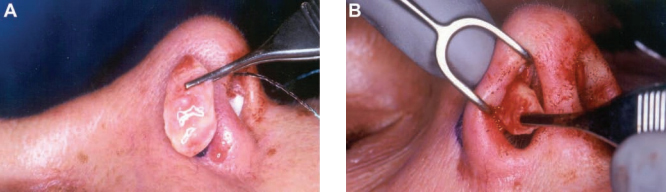
Alar batten grafts. The most common treatment for repair of external nasal valve collapse is the placement of alar batten grafts (Figure 16). These grafts help to augment and strengthen the weakened or absent lateral crus of the LLC. 10 Dysfunction of the external nasal valve is most often seen after overresec- tion of the lateral crus of the LLC from a previous rhinoplasty, in an attempt at tip modification. (Clinical examples can be seen in the patient in Figure 17.) The alar batten graft is usu- ally fashioned from auricular conchal or septal cartilage.
It is critical that the graft be the correct size to bridge the dysfunc- tional cartilage in a precise soft tissue pocket. The grafts are placed just caudal to the LLC, to support the external nasal valve, and they extend laterally to the bony lip of the pyriform aperture, at the point of maximal lateral wall collapse. 75
The alar batten grafts must be situated in a position to effectively support the region of the external nasal valve that collapses on inspiration (Figures 18A and 18B). The alar batten grafts may be secured with an absorbable suture through the nasal mucosa, in order to pull up the mucosa against the cartilage. 10 Studies by both Becker and Becker76 and Toriumi et al 77 have shown excellent long-term results in treating external nasal valve collapse with this technique. Although these grafts are usually placed to address external nasal valve collapse, they can also be placed to help bolster the internal nasal valve when they are secured at the junction of the ULC and LLC or scroll region.

Alar strut grafts. Contrary to alar batten grafts, which over- lay the lateral crus to provide support, alar strut grafts act like a support beam from below to strengthen the LLC. Originally reported on by Gunter and Friedman, 78 these grafts are placed in a pocket underneath the lateral crus by dissecting the
vestibular skin away from the cephalic portion of the LLC. This graft acts to support the lateral crus immediately lateral to the dome and stretches to the area of its fibrous attachment at the pyriform aperture.
Placement of these grafts deep to the lateral crura also eliminates the slight alar fullness that is sometimes seen when they are placed as the alar batten grafts described above. 79
Lateral crus pull-up. Another method described by Menger, 80 for cases where the external nasal valve is floppy, is termed the lateral crus pull-up. This technique utilizes a spanning suture to rotate the lateral crus of the LLC superolaterally; it is fixed in place with a permanent suture through the pyriform aperture. This suture is anchored through a hole that is drilled in the pyriform aperture.
Z-plasty/skin grafts/composite grafts. Z-plasty is a well- established maneuver for correcting cicatricial scarring and stenosis of the external nasal valve. This technique, designed to lengthen the area of contraction and decrease the stenotic segment of the external nasal valve, has largely been describedin the surgical treatment of the cleft nasal deformity. This maneuver utilizes the rearrangement of intranasal skin flaps and is very similar to the one described above for treatment of the internal nasal valve. Skin grafts and composite grafts have also been described to reconstruct a scarred area of the exter- nal nasal valve. Additionally, small areas of scarring can be primarily divided to release the scar band and then kept open with different forms of stenting. 3
Complications
For the purpose of this article, we discuss selected compli- cations that relate to the subject of the surgical treatment of nasal obstruction. Nasal obstruction can occur secondarily to rhinoplasty surgery. For instance, overresection of the lateral crura can lead to external and internal nasal valve collapse. Also, failure to resecure the ULC with spreader grafts after hump reduction may contribute to middle vault collapse and internal valve collapse. Although pertinent to the discussion, these topics would be complications of rhi- noplasty and cannot be fully addressed here.
Early Complications of Septoplasty
Early complications of septoplasty primarily relate to hemorrhage, which should be distinguished from the typical 24 to 48 hours of postoperative spotting expected. Significant perioperative hemorrhage in septoplasty ranges from 6% to 13.4% of cases. 81,82 Acute bleeding during nasal surgery may occur as a result of inadequate local anesthetic, inadequate wait for the vasoconstrictive effects of the epinephrine to occur, or mucoperichon- drial flap tears during elevation. It is prudent to inject as soon as possible at the beginning of the surgery and then to wait approximately five minutes or more after injection of 1% lidocaine with 1:100,000 epinephrine before proceeding. This time is appropriate for decon- gestion of the nose with oxymetazoline-soaked cotton- oids and for making other surgical preparations. Mucosal decongestion, particularly when accompanied by nasal endoscopic exam, gives the surgeon immediate feedback as to the relative contributions of the bony structures of the lateral nasal wall and any existing allergic or inflam- matory sinonasal disease. With adequate local anes- thetic, intraoperative bleeding should be minimal.
Significant arterial bleeding is rare. Cerebrospinal fluid (CSF) leak is a potential early com- plication of septoplasty that is exceedingly rare but war- rants discussion given its severity. CSF leak occurs when submucous resection is carried too high in the nasal cav- ity. A crack in the very thin bone of the anterior skull base (generally at the cribiform plate in the midline or the fovea ethmoidalis more laterally) and a concomitant tear of the dura mater on the floor of the anterior cranial fossa results in communication of the subarachnoid space and the nasal cavity. 83,84 In one extreme case, a patient developed a meningoencephalocele requiring more invasive repair. 83 Although this problem is extremely unusual after septo- plasty, it can be life threatening if not rapidly diagnosed and appropriately managed because of the attendant risk of meningitis. Sinonasal surgery is the second most com- mon cause of CSF leak, second only to traumatic skull base fractures. CSF leaks typically occur early in the post- operative period but in some cases may present later. This delay is exacerbated by the presence of nasal packing, which obscures both the nature and source of the patient’s rhinorrhea. In addition, patients undergoing day-surgery septorhinoplasty may not be familiar with the classic symptoms, which include clear rhinorrhea, headache, and a salty or metallic taste in the postnasal drip. This could delay presentation for days in some cases, significantly increasing the risk of ascending infection.
When performing a septoplasty in which a high bony septal deviation must be removed to improve nasal airflow or correct an external deformity, a controlled break of the perpendicular plate of the ethmoid bone provides safe sepa- ration from the skull base, provided that visualization is adequate. In the case of severe deformity (generally follow- ing blunt external trauma), removal of the bony and carti- laginous septum in controlled pieces is prudent, given that an uncontrolled break of the perpendicular plate can place significant force on the anterior skull base. This delicate area may have sustained some trauma during the injury to the nose, thus rendering the patient more prone to CSF leak.
Minimizing the rate of CSF leak after septoplasty is best accomplished through prevention; early diagnosis of this rare complication will ensure that further morbidity owing to ascending infection is avoided. In a review of mortality following rhinological procedures, Tawadros and Prahlow85 showed that the risk of CSF leak after nasal surgery is increased in patients with a low-lying cribriform plate of the ethmoid roof (Keros type III), specifically found at a level inferior to two-thirds of the orbit height on the preop- erative coronal CT scan. Thorough review of available preoperative imaging, particularly in patients with a known history of trauma or previous nasal surgery, is imperative. In cases where there is no imaging available, exam under anesthesia (either with a headlight and speculum or prefer- ably with a telescope) will alert the surgeon to significant nasal anatomic variations. Prevention of skull base injury in difficult cases may then require a less aggressive septo- plasty method, especially when manipulating the perpen- dicular plate attachment to the ethmoid roof.
Antibiotic prophylaxis for meningitis should be given immediately at the time of the suspected diagnosis of the CSF leak, as waiting for diagnostic imaging or fluid beta- 2-transferrin will delay potentially life-saving therapy. Conservative management of CSF leak is preferred, with placement of a lumbar drain by either the anesthesiologist or neurosurgical consult service. Surgical repair is reserved for patients with a persistent leak despite at least 72 hours of lumbar drainage, bed rest, and sinus precautions (avoidance of nose blowing, sneezing, and nasal medica- tions). The standard of care is endoscopic repair, except in cases of very large defects, and a multilayer repair is per- formed at the defect site. 86 When the defect cannot be readily identified on endoscopic exam, intrathecal fluores- cein may be employed to aid localization. 86 In the event that a CSF leak is observed during surgery, this may be repaired immediately with endoscopic techniques, once informed consent for the additional procedure is obtained.
Postoperative Infection
Occurring in the first postoperative week, local infection is an important complication to recognize and ideally to prevent. Postseptoplasty infection is very uncommon, with the literature showing a rate of 0.48% to 2.5%. 87,88 In these cases, infections are almost exclusively localized to the septum and nasal cavity, although hematogenous spread can rarely occur, particularly in patients with an immunodeficiency of any origin. Ascending infection may present as meningitis, cerebritis, subdural empyema, brain abscess, and even cavernous sinus thrombosis. 87 The pathogenesis of infections occurring after nasal surgery is related to the normal mucous membrane colonization of the upper respiratory tract. The mucous membrane barrier is violated during the approach to the nasal septum and thus provides a point of entry for bacteria, which may then enter the vascular system through the arcade of capillaries and venules beneath the epithelium. 89 There is evidence that a transient bacteremia occurs during open septorhinoplasty. This is usually harmless in healthy sub- jects and resolves quickly and spontaneously. Certain higher risk populations, however, require greater atten- tion, such as patients with mitral valve replacements. 89
The risk of bacteremia increases in septoplasty if nasal packing is left in place for 48 hours after surgery and cases of toxic shock syndrome have been reported. 90-93 Staphylococcus aureus, an important pathogen in nosoco- mial infections, is a frequent cause of bacteremia in post- operative patients. 89 Toxic shock syndrome results from the concentration of the bacterial endotoxin in the absorbent nasal packing material, analogous to the original reported cases secondary to tampon use. 91,92 Release of this toxin into the systemic circulation begins a rapid cascade of sep- sis. This manifests as high fever and diffuse erythema and is followed by peripheral desquamation, hypotension, tachycardia, vomiting, and diarrhea. Treatment must be initiated promptly, starting with removal and culture of the nasal packing, hospitalization for the administration of fluids, empiric antibiotics against S. aureus, and vasopres- sors if needed. 91,92 Given this potential risk, patient discom- fort, and possible deleterious effects on mucosal healing, it is beneficial to avoid nasal packing unless absolutely required for uncontrolled oozing.
The administration of perioperative antibiotics in septo- plasty is controversial. Caniello et al 90 found no significant difference in pain, fever, nausea and vomiting, bleeding, and purulent secretions postoperatively with or without antibiotics. However, when septoplasty is carried out with other procedures, such as endoscopic sinus surgery or rhinoplasty, infection risk theoretically increases. Further, the cost of a single dose of preincision antibiotic is small in comparison to the cost of postoperative infectious com- plications, and national guidelines support antibiotics in all procedures requiring skin or mucous membrane viola- tion. Thus, preoperative antibiotics are recommended. Postoperative antibiotics, however, are given only to those patients who have structural grafting or who require intra- nasal splint or packing placement. In this situation, antibi- otic therapy must be maintained for the duration of the intranasal packing and for three to five days afterward in the case of nonabsorbent splint materials (such as silas- tic). Finally, patients with significant comorbidities such as diabetes or immunocompromise must receive prophy- lactic antibiotics. In all cases of acute or chronic infection of the operative site, placement of cartilage grafts, implan- tation of allogenic materials, presence of a hematoma, mechanical blockage attributable to nasal packing, or postoperative nasal obstruction producing rhinosinusitis, antibiotics should be administered. 87,88
Intermediate Complications of Septoplasty
A septal hematoma occurs when significant venous oozing continues after the septal mucosa incision is closed, result- ing in blood being trapped between the mucoperichondrial flaps or against the remaining cartilage. 94 If this goes unrec- ognized and is not treated early, septal hematoma can be a major complication of septoplasty. An untreated septal hematoma begins a cascade of events that can lead to sev- eral other complications, including ischemia and necrosis of the septal cartilage, decreased septal support, and collapse of the middle vault. The result of this structural insufficiency is the saddle nose deformity.
Prevention of septal hematoma is effectively accom- plished by employing a mattress suture technique and by ensuring adequate drainage. Nasal packing or splinting may also be effective but can cause patient discomfort or pain. According to Lee and Vukovic, 95 the mattress suture technique reduces the possibility of a septal hematoma by directly abutting the ipsilateral and contralateral muco- perichondrial flaps, closing any inadvertent tears in the mucosa, and supporting cartilage pieces retained after the septoplasty in optimal position. In addition, suture tech- niques reduce patient discomfort by eliminating the need for nasal packing.
If a septal hematoma does occur, it may contribute to the formation of a septal abscess. Blood products make an ideal broth for bacterial growth and the nasal mucosa is frequently colonized with pathogens. Organisms found in septal abscesses include Staphylococcus, Haemophilus influenzae, and rarely Pseudomonas aeruginosa. Should a septal abscess develop, it should be drained immediately. This is most often done first with large-bore needle aspira- tion. Subsequently, the septal incision is reopened, allow- ing the abscess to drain. Purulent material should be rinsed out of the nose gently with saline irrigation. Bilateral nasal packing should then be placed to eliminate the septal dead space and prevent reaccumulation of fluid. Antibiotics should be administered after drainage to pre- vent abscess reformation or further infection by hematog- enous spread. Also, the patient should remain on antibiotics as long as the nasal packing is present.
Late and Lasting Complications of Septoplasty
Mucosal Adhesions/Synechiae
Mucosal adhesions, also known as synechiae, are abnormal bridges of inflamed and adherent mucosa that may cause nasal obstruction after septorhinoplasty. Synechiae occur when opposing mucosal surfaces are abraded or injured and are most commonly formed between the septum and infe- rior or middle turbinates. Synechiae formation complicates approximately 7% of septoplasties, generally forming in the late wound-healing phases of recovery. 96 Although less com- mon, adhesions at intranasal intercartilaginous incision sites may cause internal nasal valve synechiae and result in nasal obstruction (see above). Patients generally remain asympto- matic if the adhesions occur posteriorly. Postoperative air- way obstruction attributable to adhesions more anteriorly is experienced as a change in the direction of nasal airflow or greater resistance on inspiration. 81
As with most complications of septoplasty, careful sur- gical technique may be expected to reduce the incidence. Prevention of postoperative synechiae can be improved via placement of endonasal splints, although this is some- what controversial. 81,87 Splints are made of silastic sheet- ing and are placed against the septum for one to two weeks after surgery. 97-99 Malki et al 97 reported that there was no significant difference in synechiae incidence between splinted and nonsplinted patients. They con- cluded that if the goal was to prevent adhesions, nasal splints were not justified. Most rhinoplastic surgeons now employ intranasal splints in only select cases where sig- nificant instability is anticipated. Packing provides an alternative but itself is associated with potential complica- tions. For the majority of patients, the authors’ approach is a septal suture technique.
Septal Perforation
Septoplasty or nasal surgery is the second leading cause of septal perforation after nasal trauma and is reported at rates less than 1% to 6.7%. 81,87,96,100-102 Perforation occurs when there are bilateral opposing tears in the mucoperi- chondrial flaps. It has been reported that 62% of patients with septal perforations are asymptomatic. 81,100,103 Symptoms of septal perforation may include dryness and crusting, intermittent epistaxis, pain, rhinorrhea, whis- tling during nasal inspiration, abnormal airflow, and a paradoxical sensation of nasal obstruction. Most perfora- tions are small and anterior, causing turbulent flow and decreasing the humidification of inspired air. A small number of perforations may enlarge over time, and some may eventually destabilize the nose and lead to a saddle nose deformity. 103
Septal perforation may occur despite meticulous tech- nique. Still, meticulous surgical technique may reduce the incidence. Great care should be taken to avoid inadvertent dissection in a submucosal supraperichondrial plane, lead- ing to perichondrial or periosteal resection with the speci- men. 103 The perichondrial layer imparts most of the biomechanical strength to the septal lining. 103 This tissue is also essential, in the case of a small tear, in separating the free mucosal edges of the raised flaps after removal of the septal cartilage or bone. Without this intervening layer, the mucosa edges may heal together, making a perforation. Intraoperative perforations should be recognized and repaired with simple interrupted 5-0 chromic sutures, with the help of an endoscope if needed. Tears occur mostly over convexities, spurs, or crests, and the resulting surplus of mucosa may facilitate endonasal sutures without tension. 81
When septal perforations occur, they should first be managed conservatively with observation and improved nasal hygiene and humidification. Some patients exacer- bate the problem and enlarge the size of the perforation from repeated trauma, picking at the crusting that occurs. In cases of severe symptoms, repair may alleviate breath- ing problems, bleeding, crusting, frontal headaches, and nasal whistling. Unilateral or bilateral bipedicled mucosal flap closure with autogenous grafts is the preferred method for closure of small- to medium-sized (<20 mm) nasoseptal perforations, although there are many alternatives in the literature. 100 This method has resulted in a 90% closure rate and significant improvement in symptoms. 104 An open rhinoplasty approach may facilitate repair. 104 This method is extremely helpful for exposure, especially with larger (>20 mm) defects.
Aesthetic Complications
In addition to functional complications of septoplasty, the risk for aesthetic complications exists. 81 There is a reported risk of 1% to 4.5% of major aesthetic change. 101,105,106 Postseptoplasty nasal deformities result from loss of sup- port mechanisms, cartilage mobilization or weakening, and partial overresection. Three major types of deformity occur: tip projection loss, supratip depression or dorsal saddling, and columellar retraction.
There is no relation between general surgical risk factors for septoplasty and the possibility of aesthetic deformity after the procedure and no reported increase in risk for aesthetic complica- tions in patients who have had previous septal surgery. 101
The extreme end of the spectrum of dorsal destabiliza- tion is the saddle nose deformity (Figure 19). The K-area, or keystone, is the critical area in which the quadrangular cartilage, nasal bones, perpendicular plate, and ULC come together. When the K-area is disrupted, it may act as a pivot point; downward and inward rotation of the anterior septal cartilage then becomes possible. Subsequently, this rotation may widen the nasal base. 81 Avoidance of K-area instability and overresection of the dorsum is essential in children because septal trauma or surgery can inhibit the growth of the prepubescent nasal cartilage and thus pre- dispose the child to a saddle deformity after puberty. 87
In all cases, if septal cartilage is removed in the treat- ment of a septal spur or deformity (or for grafting pur- poses), it is crucial to maintain a 10- to 15-mm “L-strut” of cartilage along the nasal dorsum and caudal septum. After treatment of the septum is complete, the surgeon should verify adequate fixation of the caudal septum; if it is mobile, it must be stabilized to the maxilla with a Wright suture into the periosteum of the nasal spine. Dislocated septal cartilage may be repositioned with a guide suture (figure-of-eight) through the columella. 81 At the conclusion of the case, gentle palpation of the dorsum and tip support should be standard. If weakness is present, additional structural techniques should be per- formed before waking the patient.

Sensory Disturbance
Sensory disturbance of the anterior palate and central inci- sors has been reported in 2.8% of patients after septo- plasty. 107 This is most likely related to direct injury of the branches of the nasopalatine nerve at the floor of the nose and in the maxillary crest, secondary to drilling or chis- eling in this area. Conservative resection along the maxil- lary crest is therefore recommended.
Blindness
Blindness is a rare but frightening complication of septo- plasty. The pathogenesis of vision loss after septoplasty is unclear, and many different mechanisms are possible. One possibility relates to the application of high-pressure intra-arterial injections of lidocaine with epinephrine. When this mixture is injected into the membranous part of the caudal septum or into the turbinates, retrograde flow could enter branches of the ophthalmic artery. Embolism or vasospasm then occurs, with subsequent occlusion of the feeding vessels of the ophthalmic artery, causing uni- lateral blindness. Some authors have suggested that slower injection at a single site could prevent this complication, although the extreme rarity of this event makes preventative measures difficult to assess. 87,108 In addition, direct trauma to the optic nerve during septoplasty is another mechanism that has been reported to have caused blindness. Instruments for fracturing the bony septum may be placed too high and too laterally in the posterior nasal cavity, entering the optic canal with an aggressive mallet strike.
Complications Of Turbinate Surgery
Early Complications of Inferior Turbinate Reduction
Inferior turbinate reduction can be a useful adjunct to septorhinoplasty in patients with preoperative nasal air-way obstruction and inferior turbinate hypertrophy. There are many different methods, and each has its own particu- lar potential complications. Although some controversy persists in the literature with regard to the quantity and methods of turbinate resection, the focus here will be complications in general. It is worth noting, however, that total turbinate resection is never indicated for the treat- ment of nasal obstruction and that the physiologic func- tion of the inferior turbinates is important to maintain.
The most common complication of inferior turbinate reduction is hemorrhage. Hemorrhage after septorhino- plasty with treatment of the inferior turbinates most com- monly originates from the turbinate remnant. 82,109 Prior to initiation of turbinate reduction, it is very helpful to inject the head of the turbinate with lidocaine with 1:100,000 units epinephrine (usually 1 mL). This mixture should be allowed to work for five minutes prior to incision and, as with septoplasty, the mucosa can be decongested with oxymetazoline-soaked cottonoids during this time. Submucous resection, with or without the assistance of a microdebrider, may then proceed. If visualization is ade- quate, particularly without powered instruments, working from posterior to anterior will help to maintain a clear field. The microdebrider may increase the efficiency of turbinateremoval and help to clear the nasal cavity of debris and blood. In addition, the microdebrider reduces mucosal trauma when used precisely; if the surgeon is not meticu- lous, however, accidental contact with the septum, middle turbinate, or nasal vestibule can lead to a poor result. Severe postoperative hemorrhage is rare, but mild oozing is to be expected. This may be treated with short-term use of topical decongestant sprays and humidification.
Newer treatment options for inferior turbinate reduction have some different risks. Radiofrequency ablation and elec- trocautery procedures may be performed in the surgeon’s office with only local anesthesia. With radiofrequency reduc- tion, careful observation of the placement and temperature of the radiofrequency device tip must be maintained throughout to avoid pain and possible thermal injury. 1,54 Results with traditional electrocautery have not been favorable when com- pared to other modalities and have included significant patient discomfort (when performed awake) and postopera- tive edema and crusting, which may last up to six weeks. 57 Carbon dioxide laser techniques have been successful in the treatment of inferior turbinate mucosal hypertrophy, with scant blood loss and minimal patient discomfort. Hemorrhage may occur, however, when the resulting eschar sloughs in the days following surgery, and postoperative crusting is still a problem for some patients. The laser also requires technical expertise, expensive equipment, and safety precautions that make it impractical in many settings. 54 Last, it is important to note that removal of the bony portion of the turbinate (infe- rior concha) is not possible with these techniques, signifi- cantly limiting their long-term utility in some patients.
Late Complications of Inferior Turbinate Reduction
Apart from the risk of recurrent nasal obstruction after inadequate inferior turbinate reduction, there are compli- cations involving mucosal or bony injury, the postopera- tive healing process, and overresection. As discussed previously, inadvertent mucosal injury during nasal sur- gery can have significant long-term results that are diffi- cult to appreciate at the time of surgery. Synechiae may form between the inferior turbinate and the septum. Patients are often asymptomatic, but in some cases, per- sistent nasal obstruction may be perceived, or the syn- echiae may even contribute to a poor result of the septorhinoplasty as a whole. Although placement of nasal packing or silastic stents may reduce the risk of synechiae, this is not without complications (as discussed above). The key to prevention of poor results from adhesion for- mation is synechiae prevention with protection of the mucosal surfaces of both the turbinate and the septum and prompt repair of accidental tears whenever feasible.109
In addition to mucosal injury and related complica- tions, the bony portion of the inferior tubinate (concha) may be injured during turbinoplasty. Especially with elec- trocautery for inferior turbinate reduction (but also with the carbon dioxide laser), there is a risk of bony necrosis. 54 Direct thermal injury to the thin bone of the concha may destroy its delicate blood supply and this damage may be irreversible. This leads to necrosis, sequestration, inflam- mation, pain, and increased risk of infection. 110 In some patients, this requires a second procedure to remove the dead bone, and the resultant turbinectomy may predispose the patient to severe crusting or other complications.
Overresection causes the most difficult-to-manage of the late complications, resulting in persistent crusting and, in severe cases, atrophic rhinitis. As Lindemann et al 111 showed with fluid dynamics modeling, inferior turbinate resection leads to severe disturbance in nasal airflow and dramatically impairs air conditioning function. The nor- mal physiologic function of the inferior turbinate is humidification and filtration of inspired air. In its absence, dry air with particulate matter enters the nose, and the mucociliary clearance formerly provided by the ciliated epithelium of the inferior turbinate is no longer possi- ble. 54,112 Thick mucous crusts may form and the patient may develop significant rhinorrhea, foul smell or taste, and a paradoxical sensation of nasal airway obstruc- tion. 1,113 Alterations in the airflow and mucous clearance in patients with atrophic rhinitis may eventually lead to changes in bacterial colonization and may predispose the patient to bacterial rhinitis with distinct flora such as Klebsiella ozaenae. 112,113 Some improvement may be achieved by routine humidification, a variety of nasal irri- gations, improved nasal hygiene, and topical antibiotics, but no curative treatment exists for this complication.
Outcome Assessment In Surgery For Nasal Airway Obstruction
Although the outcome evaluation of the surgical treatment for nasal obstruction is often straightforward and obvious, at times it can be difficult and subjective.
Straightforward clinical assessment of postoperative nasal airflow can be performed in the clinic with the same techniques employed in the initial diagnostic visit (see above). Clinical assessment, paired with a basic, subjective response from the patient, has been the most frequently reported outcome assessment in the litera- ture. 75 More rigorous symptom-based assessment and objective data, however, have been historically more difficult to generate. The generic nature of outcome reports, coupled with the retrospective nature of the overwhelming majority of studies of nasal airway sur- gery, has led to an accumulation of level IV evi- dence. 75,114 Although much of this has been positive in the sense that surgeons have data to support the effi- cacy of their patient selection and treatments, lasting effects of nasal airway surgery have been difficult to document and preoperative prediction of patient benefit (according to diagnostic maneuvers, anatomy, or the surgeon’s overall impression) has not been reliably achieved. 75,115,116 Finally, correlation between physical or anatomic findings by the surgeon and patients’ relative improvement after procedures has been very poor across studies. 114,117
In this section, objective postsurgical nasal airway evaluation is reviewed. This includes general considera- tions and a review of the current literature.
Objective Outcomes Studies
Objective studies of improvement in nasal function after surgery for nasal obstruction have included assessment of nasal air conditioning, nasal volumes, cross-sectional areas, and airflow pattern. 111,115,118,119 Unfortunately, results of these studies have often conflicted and have failed to provide a clear picture with regard to preoperative and postoperative objective assessments. Adding to the confu- sion, a broad range of success rates has been reported in the literature, between 43% and 90%. 120
Acoustic rhinometry and rhinomanometry, both described above, have been employed in objective postop- erative assessments of nasal airway surgery, in addition to preoperative diagnosis and selection of surgical candi- dates. The data regarding these measures are mixed across multiple studies, with multiple groups publishing conflict- ing results from similar research designs. Kemker et al 118 showed increased postoperative volumes on postdecon- gestion acoustic rhinometry, whereas Reber et al 119 found no increases in postoperative volumes and, furthermore, found no correlation between measured cross-sectional areas and subjective nasal patency either before or after surgery.
Dinis and Haider 115 employed rhinomanometry to assess septoplasty patients pre- and postoperatively and then compared objective measures to patients’ reported satisfaction. They found that rhinomanometry does not correlate well in many cases and only shows increased resistance in anterior deviation. 115 Further, even in cases where rhinomanometry was useful in diagnosis, it failed to predict long-term outcome (ie, patient satisfaction) in the years after surgery. 115 This result is supported by Kim et al, 103 who showed that acoustic rhinometry and rhi- nomanometry measures are not significantly correlated with patients’ subjective assessments of airway obstruc- tion. Because this is the ultimate driver of success in nasal airway surgery, the authors emphasize that objective assessments should not be overvalued relative to the patients’ subjective impressions. The difficulty with these data, however, is the significant recall bias inherent in purely subjective outcomes studies, particularly those that do not employ standardized, validated clinical outcomes instruments.
Sipila and Suonpaa121 used acoustic rhinomanometry to select surgical candidates with apparent success in a large study supported by the Finnish health system. The authors showed that patients with high intranasal resistance preop- eratively were satisfied with the surgical outcome 85% of the time. 121 The authors presented this result as supportive of rhinomanometry as a screening tool in identifying the best surgical candidates. Additional support for objective measures comes from Skouras et al, 122 who showed increased cross-sectional area and nasal volumes postsepto- plasty. These authors also reported that symptom improve- ment paralleled objective data, although no statistical correlation was given. 122 Last (and in contrast with other studies), Grymer et al 123 have shown a positive correlation between minimal cross-sectional area and the subjective feeling of nasal patency both pre- and postseptoplasty.
In a review of the literature, we found that most nasal obstruction studies only objectively examine the smaller nasal cavity (ie, the side of maximal deflection or spur), but correction of septal deviation may result in changes in airflow on the contralateral (larger) side. Increased obstruction may manifest at the contralateral internal valve in some cases, and this has a significant effect on outcome. Pirila and Tikanto124 showed that patient satis- faction is negatively correlated with a decrease in the cross-sectional area of the contralateral internal valve. When there is significant improvement in cross-sectional area at the ipsilateral or bilateral internal valves, however, satisfaction increases, and the correlation between area and subjective airflow is strong.
The data supporting improvement in nasal air condition- ing with surgery for nasal obstruction leave less doubt about positive results. Multiple studies by Lindemann et al 111,125 showed that nasal physiologic functions, such as heating and humidifying inspired air, were improved by septoplasty and septoplasty with appropriate inferior tur- binate reduction. This effect is derived from increased vol- umes and direction of physiologic airflow to key places in the nasal passage, thus increasing mucosal contact with the nasal air stream. In addition, filtration of particulate matter may be more effective with improved flow dynamics.
Quality of Life Assessments and Patient Satisfaction
In addition to objective measures, multiple authors have sought a standardized assessment of results from the patients’ perspective (ie, subjective). These efforts have taken the form of symptom-based questionnaires and inventories and have met with variable success. 126-128 The importance of outcomes research and assessment of health-related quality of life (QoL) continues to grow, par- ticularly as economic factors play an increasing role in treatment decisions. As such, there has been a significant rise in the efforts of surgeons to quantify the benefit that patients receive from particular interventions. This has taken the form of symptom or disease-specific outcome measures, the best of which are standardized, validated, and then employed across multiple studies of different treatments. 114,117,129
Schwentner et al 127 designed a mailed questionnaire (a composite of multiple outcomes instruments and a visual analog scale) to assess patients’ subjective QoL after septo- plasty. The response rate was approximately 50%, which is standard for such methods, and most patients were more than two years postoperative. Analysis of the symptombased subsets showed significant improvement in each category, including “overall medical state.”127 This result was consistent over different lengths of follow-up and accompanied improvements in nasal-specific QoL. In a similar study, Siegel et al 116 employed the Nasal Health Survey (NHS), as well as the Short Form 12 (SF-12), to assess septoplasty-related changes in QoL. Patients achieved significant improvement in both symptom and medication use subscores of the NHS at a mean follow-up of nine months, although no significant change was observed in the SF-12. 116 These studies highlighted the utility of disease- specific measures, but they also underline the need for standardization. Interpretation of results between studies is greatly facilitated when authors employ the same instru- ments rather than novel scales or ad hoc surveys.
The most rigorously developed disease-specific meas- ure for nasal obstruction was created by the Nasal Obstruction Symptom Evaluation (NOSE) study investiga- tors. 128 These authors began with multiple questions derived from different assessments and then employed multiple rounds of item elimination and statistical valida- tion to arrive at a five-item instrument that tracks nasal obstruction-related QoL. The NOSE scale generates an integer score out of 100 and thus facilitates quantitative comparisons within subjects at different time points or between groups of subjects undergoing different treat- ments. 128 Thus far, the NOSE has been employed in a handful of important outcome studies. 117,126,128,129
Stewart et al 128 followed up the development of the NOSE scale with an analysis of septoplasty with or with- out turbinate reduction. This study showed a significant disease-specific benefit in both groups at three and six months postoperatively, as well as decreased medication use. 128 As in many other studies, the authors could not show correlation between patient physical exam assess- ments and outcomes. Rhee et al 126 also employed the NOSE scale in their examination of nasal valve surgery. These authors showed improvement over baseline at three and six months, with improvement also present between the three- and six-month assessments (attributable to healing and resolution of edema over time). 126 Interestingly, this study also showed that physician rating of nasal obstruction on a visual analog scale predicted patient QoL, leading the authors to question the utility of objective measures. 126 Finally, Most 129 reported NOSE results after 41 functional rhinoplasties, with significant improvement noted across multiple surgical techniques used to address nasal obstruction.
A smaller number of studies have examined global health-related QoL in patients undergoing nasal sur- gery. 116,130-132 These studies have not shown improvement in global estimates of health-related QoL related to nasal surgery, although some hint at an effect on overall health. This is not entirely unexpected because the burden of nasal obstruction is likely below the measurable threshold for generic QoL instruments. 117,128 These findings under- line the importance of routine employment of high-quality disease-specific instruments, such as the NOSE scale. 128 Uppal et al 132 showed a significant correlation between subjective nasal symptom improvement and Glasgow Benefit Inventory (GBI) scores postseptoplasty. It is impor- tant to note, however, that the GBI is an outcome measure designed to specifically assess the benefit received from a particular procedural intervention; it is not a true assess- ment of global health-related QoL. The authors have shown that the GBI, however, may be an alternative means of quantifying subjective benefit. This is useful because the GBI may also be used in other procedural assessments and thus facilitates comparison of the relative benefit of heterogeneous management strategies or even treatments for different diseases entirely. 132
Unfortunately, the studies reviewed here represent a small percentage of the literature, which continues to focus primarily on technical description and level IV evi- dence. A recent systematic review of nasal valve surgery highlights the overall weakness of the evidence in the field of functional rhinoplasty and surgery for nasal airway obstruction. 75 Higher level evidence and greater emphasis on standardized, quantitative approaches are the keys to advancing the field—particularly in light of the size of the market for nasal obstruction treatment, which has been estimated at $5 billion each year. 127
Last, some discussion of patient satisfaction is war- ranted. Satisfaction is related to QoL but represents a dis- tinct entity; it is both difficult to define and difficult to isolate, in terms of the effects of a particular surgical inter- vention in the global picture. Also, as most surgeons have experienced, satisfaction is fluid—it changes over time as patients adapt to new health states and recall of previously significant symptomatic states diminishes. It is thus impor- tant to delineate satisfaction from attempts at quantitative assessment of patient symptoms because the former is general and has a significant emotional component, whereas the latter relies on patient-reported data to deter- mine a composite picture specific to their health or a par- ticular disease state.
Patient satisfaction with an external or aesthetic result can be significantly reduced if nasal obstruction is untreated or, worse, caused during septorhinoplasty. 1,133 Thus, it is critical to approach nasal obstruction concur- rently and thoroughly. Overall, surgical correction of patients’ subjective sensation of nasal obstruction has widely variable results in terms of satisfaction, with most data in the range of 60% to 90%. 115,121,124,128 This may reflect heterogeneity in the extent of surgery or the man- ner and timing of assessments. For example, Dinis and Haider 115 found patient dissatisfaction with the level of improvement after correction of posterior deviation. It would be ideal to use an objective test to delineate surgical candidates (and likely success) from nonsurgical disease, but the authors observed that the correlation was not sig- nificant. Further, patients with anterior deviation were very satisfied only 42% of the time in this study. 115 In contrast, Sipila and Suonpaa121 showed 85% satisfaction in patients at six months with acoustic rhinometry for screening. It is worth noting, however, that this was a unique situation, where treatment decisions were based on external pressures and patients had relatively little influence. 121
Konstantinidis et al 131 were able to show disease-specific improvement but not global; more importantly, they reported that patient satisfaction with improved nasal air- way function attenuates significantly over time. This dem- onstrates a significant but not immediately obvious issue: appropriate timing for outcome assessments. It is impor- tant to assess results after healing has occurred and tissues have settled but before patients forget the burden of their preoperative symptoms. Furthermore, multiple assess- ments are necessary to track changes over time. Thus, it is recommended that at least two short-term assessments be completed—ideally one in the three- to six-month range and a second at one year. Further long-term assessments are useful but not practical in many contexts and should occur at three to five years for the purpose of clinical trials.
Safety Issues In Nasal Surgery
Nasal surgery is generally safe, but careful attention to issues surrounding the surgical procedures is essential in maximizing patient benefit. Certain surgical instruments and equipment require familiarity and careful setup to ensure safe application. This is true of the microdebrider, particularly as it relates to inadvertent mucosal tears, for- mation of adhesions, and overresection (see above). It is also crucial when using the CO2 laser, as careless setup, improper calibration of the power, or inaccuracy of the aiming beam could result in injury to intranasal structures, as well as the patient’s external nose or face.
It is important to discuss the risk of operating room (OR) fire and airway burns. There is a risk of ignition with any application of electrocautery and lasers, but this risk is dramatically increased in the setting of nasal cannula or face tent supplemental oxygen. 134 Elevated local oxygen saturation results from escape of supplemental oxygen into the surgeon’s field. When loose drapes are employed to cover the patient, oxygen may also become trapped beneath flammable materials and rise to very high concentrations. Facial burns, intraoral and airway burns, and even patient demise have been reported. 134 Although burn injuries in the OR are rare, they represent 20% of all malpractice claims for cases performed under monitored anesthesia care (MAC)—and 95% of these cases involve surgery in the head and neck region. 134 It is crucial to have a fire safety protocol in any operative setting, and training of office and operating room staff must be complete and up-to-date to ensure patient safety and facility accreditation.
The application of topical and injectable anesthetics and vasoconstrictive agents has also been debated, including topical 4% cocaine solution. Although these medications have many positives, including rapid onset, prolonged effect, local vasoconstriction, and decongest- ant effects, they are not without complications. Potential complications range from very mild to severe and life threatening, including abnormal taste sensations, tinni- tus, mild anxiety, myocardial infarction, cerebral vascu- lar accident, and death. Unfortunately, there are no preoperative criteria, other than previous history of adverse reaction, to identify patients at increased risk. 135 It is imperative to remember the maximum dosing for each drug and that doses are additive. In addition, vigi- lant perioperative cardiopulmonary monitoring is essen- tial, including blood pressure, pulse oximetry, and electrocardiography. Treatment of systemic toxicity includes oxygen, intravenous fluids, and removal of any residual agent (eg, cocaine-soaked pledgets). If cardio- vascular alterations are noted, appropriate anesthesia care and a cardiology consult are necessary.
The surgical setting and anesthesia choice also have a great potential influence on patient outcomes. There are advantages and disadvantages of local anesthesia with sedation and of general anesthesia. Nasal surgery can be performed safely under either sedation or general anesthe- sia. The method of anesthesia employed during septorhi- noplasty varies between surgeons and in different countries, with a great majority of cases in the United Kingdom, for example, being performed in a hospital set- ting with general endotracheal anesthesia (GETA), whereas this is less common in the United States. 136
Concerns about the safety of operations performed out- side of a large in-patient hospital have been addressed by large studies in the plastic surgery literature. 106,137,138 Byrd et al 106 demonstrated safe outpatient plastic surgery in a group of over 5000 cases. That study pooled multiple anesthetic strategies, so exact interpretation is difficult. Another large study, by Bitar et al, 137 examined office- based surgery in almost 5000 consecutive plastic surgery procedures. These authors found that intraoperative seda- tion and airway management performed by a registered nurse anesthetist (CRNA) and the surgeon were very safe, provided that patient selection was appropriate and clear safety protocols were in place. No deaths occurred and no surgical airways were required. 137 In their entire cohort, only one patient was emergently intubated. 137 No deep venous thromboses or pulmonary emboli occurred. 137 A small number of patients experienced postoperative nau- sea and vomiting, although this was prolonged in only a handful (<1%). Only two patients in the entire series required unplanned admission. 137 The authors advocated for the presence of CRNA for in-office procedures and also highlighted the absolute necessity of emergency training and accreditation of the staff, as well as clear patient admission and transfer protocols.
It is worth noting that without an endotracheal tube (ETT) in place, during procedures performed with local anesthesia only or with MAC techniques, there is potential for nasal bleeding to pass through the choanae, nasophar- ynx, and into the larynx. 109 In addition to alarming the patient, blood products in the glottis may cause a significant cough response, making precise surgical techniques impossible. Further, even small amounts of blood products on the vocal folds may cause laryngospasm, leading to complete airway obstruction and a need for immediate relaxation or intubation (or even a surgical airway) to avoid the possibly of pulmonary edema, cardiovascular collapse, or anoxic brain injury in severe cases. A nasopha- ryngeal pack can be a useful preventative measure, help- ing to keep the larynx clear of blood products.
Conclusions
Nasal obstruction is a relatively common problem in patients presenting for rhinoplasty; in these cases, both the functional and aesthetic aspects of their concerns must be addressed. Therefore, every rhinoplasty surgeon should cultivate a full understanding of external and intranasal anatomy, the differential diagnosis of nasal obstruction, the elements of a complete nasal examination (including nasal endoscopy), and the medical and surgical treatment options, all of which were reviewed in this article. Only after a thorough assessment of each of these factors can an appropriate operative (and postoperative) plan be dis- cussed with the patient.
Disclosures
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
References
- Becker DG. Septoplasty and turbinate surgery. Aesthetic Surg J 2003;23:393-403.
- Lane AP. Nasal anatomy and physiology. Facial Plast Surg Clin North Am 2004;12:387-395.
- Lee J, White WM, Constantinides M. Surgical and non- surgical treatments of the nasal valves. Otolaryngol Clin North Am 2009;42:495-511.
- Walsh WE, Kern RC. Sinonasal anatomy, function, and evaluation. In: Bailey BJ, Johnson JT, Newlands SD, edi- tors. Head & Neck Surgery—Otolaryngology. Philadelphia: Lippincott Williams & Wilkins; 2006. p. 307-318.
- Mygind N, Pedersen M, Neilson M. Morphology of the upper airway epithelium. In: Proctor D, editor. The Nose. Amsterdam: Elsevier Biomedical Press; 1982. p. 71-98.
- Cauna N. Blood and nerve supply of the nasal lining. In: Proctor D, editor. The Nose. Amsterdam: Elsevier Bio- medical Press; 1982. p. 45-70.
- Stammberger H. Functional Endoscopic Sinus Surgery. Philadelphia: BC Decker; 1991.
- Quinlan MF, Salman SD, Swift DL, Wagner HN Jr, Proctor DF. Measurement of mucociliary function in man. Am Rev Respir Dis 1969;99:13-23.
- Hasegawa M, Kern EB. The human nasal cycle. Mayo Clin Proc 1977;52:28-34.
- Ballert JA, Park SS. Functional considerations in revision rhinoplasty. Facial Plast Surg 2008;24:348-357.
- Marks SC. Nasal and Sinus Surgery. Philadelphia: W. B. Saunders; 2000.
- Cole P. Respiratory Role of the Upper Airways. St. Louis, MO: Mosby Year Book; 1993.
- Miman MC, Deliktas H, Ozturan O, et al. Internal nasal valve: revisited with objective facts. Otolaryngol Head Neck Surg 2006;134:41-47.
- Park SS, Becker SS. Repair of nasal obstruction in revision rhinoplasty. In: Becker DG, Park SS, editors. Revision Rhi- noplasty. New York: Thieme Medical Publishers; 2008. p. 52-68.
- Chandra RK, Patadia MO, Raviv J. Diagnosis of nasal air- way obstruction. Otolaryngol Clin North Am 2009;42:207- 225.
- Gray LP. Deviated nasal septum: incidence and etiology. Ann Otol Rhinol Laryngol 1978;87(pt 3, suppl 50):3-20.
- Mladina R, Cujic E, Subaric M, et al. Nasal septal defor- mities in ear, nose and throat patients: an international study. Am J Otol 2008;29:75-82.
- Neskey D, Eloy JA, Casiano RR. Nasal, septal, and tur- binate anatomy and embryology. Otolaryngol Clin North Am 2009;42:193-205.
- Chu CT, Lebowitz RA, Jacobs JB. An analysis of sites of disease in revision endoscopic sinus surgery. Am J Rhinol 1997;11:287-291.
- Ulusoy B, Arbag H, Sari O, et al. Evaluation of the effects of nasal septal deviation and its surgery on nasal muco- ciliary clearance in both nasal cavities. Am J Rhinol 2007;21:180-183.
- Schlosser RJ, Park SS. Surgery for the dysfunctional nasal valve: cadaveric analysis and clinical outcomes. Arch Facial Plast Surg 1999;1:105-110.
- Sheen JH. Spreader graft: a method of reconstructing the roof of the middle nasal vault following rhinoplasty. Plast Reconstr Surg 1984;73:230-237.
- Toriumi DM, Josen J, Weinberger M, Tardy ME Jr. Use of alar batten grafts for correction of nasal valve collapse. Arch Otolaryngol Head Neck Surg 1997;123:802-808.
- Deutsch E, Kaufman M, Eilon A. Transnasal endoscopic management of choanal atresia. Int J Pediatr Otorhinolar- yngol 1997;40:19-26.
- Flake CG, Ferguson CF. Congenital choanal atresia in infants and children. Ann Otol Rhinol Laryngol 1964;73:458-473.
- Samadi DS, Shah UK, Handler SD. Choanal atresia: a twenty-year review of medical comorbidities and surgical outcomes. Laryngoscope 2003;113:254-258.
- Brown OE, Myer CM III, Manning SC. Congenital nasal pyriform aperture stenosis. Laryngoscope 1989;99: 86-91.
- Burstein FD. Prevention and correction of airway com- promise in rhinoplasty. Ann Plast Surg 2008;61:595-600.
- Moore EJ, Kern EB. Atrophic rhinitis: a review of 242 cases. Am J Rhinol 2001;15:355-361.
- Rosenfeld RM, Andes D, Bhatttacharyya N. Clinical prac- tice guideline: adult sinusitis. Otolaryngol Head Neck Surg 2007;137(suppl):S1-S31.
- Hulett KJ, Stankiewicz JA. Primary sinus surgery. In: Cummings CW, Haughey BH, Regan Thomas J, et al, edi- tors. Cummings: Otolaryngology Head & Neck Surgery. 4th ed. St. Louis, MO: Mosby; 2005.
- Knipping S, Holzhausen HJ, Goetze G, et al. Rhinitis medi- camentosa: electron microscopic changes of human nasal mucosa. Otolaryngol Head Neck Surg 2007;136:57-61.
- Becker DG, Bloom JD, Gudis D. A patient seeking aes- thetic revision rhinoplasty and correction of nasal obstruction. Otolaryngol Clin North Am 2009;42:557-565.
- Constantinides M, Galli SKD, Miller PJ. A simple and reli- able method of patient evaluation in the surgical treat- ment of nasal obstruction. ENT J 2002;81:734-737.
- Corey JP. A comparison of the nasal cross-sectional areas and volumes obtained with acoustic rhinometry and magnetic resonance imaging. Otolaryngol Head Neck Surg 1997;117:349.
- Lanfranchi PV, Steiger J, Sparano A, et al. Diagnostic and surgical endoscopy in functional rhinoplasty. Facial Plast Surg 2004;20:207-215.
- Lund VJ. Objective assessment of nasal obstruction. Oto- laryngol Clin North Am 1989;22:279-290.
- Constantian MB, Clardy RB. The relative importance of septal and nasal valvular surgery in correcting airway obstruction in primary and secondary rhinoplasty. Plast Reconstr Surg 1996;98:38-54.
- Adamson P, Smith O, Cole P. The effect of cosmetic rhinoplasty on nasal patency. Laryngoscope 1990;100:357- 359.
- Naito K, Cole P, Chaban R, Oprysk D. Nasal resistance, sensation of obstruction, and rhinoscopic findings com- pared. Am J Rhinol 1988;2:65-69.
- Sipila J, Suonpaa J. A prospective study using rhino- manometry and patient clinical satisfaction to determine if objective measurements of nasal airway resistance can improve the quality of septoplasty. Eur Arch Otorhinolar- yngol 1997;254:387-390.
- Hilberg O, Jackson AC, Swift DL, et al. Acoustic rhinom- etry: evaluation of nasal cavity geometry by acoustic reflection. J Appl Phys 1989;66:295-303.
- Lal D, Corey JP. Acoustic rhinometry and its uses in rhi- nology and diagnosis of nasal obstruction. Facial Plast Surg Clin North Am 2004;12:397-405.
- Cakmak O, Coskun M, Celik H, et al. Value of acoustic rhinometry for measuring nasal valve area. Laryngoscope 2003;113:295-302.
- Grymer LF. Reduction rhinoplasty and nasal patency: change in the cross-sectional area of the nose evaluated by acoustic rhinometry. Laryngoscope 1995;105:429- 431.
- Friedman M, Ibrahim H, Lee G, Joseph NJ. A simplified technique for airway correction at the nasal valve area. Otolaryngol Head Neck Surg 2004;131:519-524.
- Fettman N, Sanford T, Sindwani R. Surgical management of the deviated septum: techniques in septoplasty. Otolar- yngol Clin North Am 2009;42:241-252.
- Gubisch W. Extracorporeal septoplasty for the markedly deviated septum. Arch Facial Plast Surg 2005;7:218- 226.
- Most S. Anterior septal reconstruction: outcomes after a modified extracorporeal septoplasty technique. Arch Facial Plast Surg 2006;8:202-207.
- Pastorek NJ, Becker DG. Treating the caudal septal deflec- tion. Arch Facial Plast Surg 2000;2:217-220.
- Metzinger SE, Boyce RG, Rigby PL, et al. Ethmoid bone sandwich grafting for caudal septal defects. Arch Otol Head Neck Surg 1994;120:1121-1125.
- Metzenbaum M. Replacement of the lower end of the dislocated septal cartilage versus submucous resection of the dislocated end of the septal cartilage. Arch Otolaryn- gol 1929;9:282-296.
- Nease CJ, Krempl GA. Radiofrequency treatment of tur- binate hypertrophy: a randomized, blinded, placebo- controlled clinical trial. Otolaryngol Head Neck Surg 2004;130:291-299.
- Nurse LA, Duncavage JA. Surgery of the inferior and middle turbinates. Otolaryngol Clin North Am 2009;42:295-309.
- Jackson LE, Koch R, James MD. Controversies in the management of inferior turbinate hypertrophy: a com- prehensive review. Plast Reconstr Surg 1999;103:300- 312.
- Cavaliere M, Mottola G, Iemma M. Monopolar and bipo- lar radiofrequency thermal ablation of inferior turbi- nates: 20-month follow-up. Otolaryngol Head Neck Surg 2007;137:256-263.
- Meredith GM. Surgical reduction of hypertrophied infe- rior turbinates: a comparison of electrofulguration and partial resection. Plast Reconstr Surg 1988;81:891-897.
- Cook JA, McCombe AW, Jone AS. Laser treatment of rhinitis: 1 year follow up. Clin Otolaryngol Allied Soc 1993;18:209-211.
- Rakovar Y, Rosen G. A comparison of partial inferior tur- binectomy and cryosurgery for hypertrophic inferior tur- binates. J Laryngol Otol 1996;110:732-735.
- Chen YL, Tan CT, Huang HM. Long-term efficacy of micro- debrider-assisted inferior turbinoplasty with lateralization for hypertrophic inferior turbinates in patients with peren- nial allergic rhinitis. Laryngoscope 2008;118:1270-1274.
- Passali D, Passali MF, Damiani V, Passali GC, Bellussi L. Treatment of inferior turbinate hypertrophy: a random- ized clinical trial. Ann Otol Rhinol Laryngol 2003;112: 683-688.
- Cook PR, Begegni A, Bryant C, Davis WE. Effect of par- tial middle turbinectomy on nasal airflow and resistance. Otolaryngol Head Neck Surg 1995;113:413-419.
- Kennedy DW, Sinreich SJ. Functional endoscopic approach to inflammatory sinus disease: current per- spectives and technique modifications. Am J Rhinol 1988;2:89-96.
- Zijlker TD, Quaedvlieg PC. Lateral augmentation of the middle third of the nose with autologous cartilage in nasal valve insufficiency. Rhinology 1994;32:34-41.
- Paniello RC. Nasal valve suspension: an effective treat- ment for nasal valve collapse. Arch Otolaryngol Head Neck Surg 1996;122:1342-1346.
- Friedman M, Ibrahim H, Syed Z. Nasal valve suspension: an improved, simplified technique for nasal valve col- lapse. Laryngoscope 2003;113:381-385.
- Nuara MJ, Mobley SR. Nasal valve suspension revisited. Laryngoscope 2007;117:2100-2106.
- Rizvi SS, Gauthier MG. Lateralizing the collapsed nasal valve. Laryngoscope 2003;113:259-269.
- Guyuron B, Michelow BJ, Englebardt C. Upper lateral splay graft. Plast Reconstr Surg 1998;102(6):2169-2177.
- Clark JM, Cook TA. The ‘butterfly’ graft in functional sec- ondary rhinoplasty. Laryngoscope 2002;112:1917-1925.
- Stucker FJ, Hoasjoe DK. Nasal reconstruction with con- chal cartilage: correcting valve and lateral nasal collapse. Arch Otolaryngol Head Neck Surg 1994;120:653-658.
- Stucker FJ, Lian T, Matthew K. Management of the keel nose and associated valve collapse. Arch Otolaryngol Head Neck Surg 2002;128:842-846.
- Hurbis CG. A follow-up study of the Monarch adjustable implant for correction of nasal valve dysfunction. Arch Facial Plast Surg 2008;10:142-143.
- Dutton JM, Neidich MJ. Intranasal Z-plasty for internal nasal valve collapse. Arch Facial Plast Surg 2008;10:164-168.
- Spielmann PM, White PS, Hussain SSM. Surgical tech- niques for the treatment of nasal valve collapse: a sys- tematic review. Laryngoscope 2009;119:1281-1290.
- Becker DG, Becker SS. Treatment of nasal obstruction from nasal valve collapse with alar batten grafts. J Long Term Eff Med Implants 2003;13:259-269.
- Toriumi DM, Josen J, Weinberger M, Tardy ME Jr. Use of alar batten grafts for correction of nasal valve collapse. Arch Otolaryngol Head Neck Surg 1997;123:802-808.
- Gunter JP, Friedman RM. Lateral crural strut graft: tech- nique and clinical applications in rhinoplasty. Plast Reconstr Surg 1997;99:943-952.
- Andre RF, D’Souza AR, Kunst HP, Vuyk HD. Sub-alar batten grafts as treatment for nasal valve incompetence: description of technique and functional evaluation. Rhi- nology 2006;44:118-122.
- Menger DJ. Lateral crus pull-up: a method for col- lapse of the external nasal valve. Arch Facial Plast Surg 2006;8:333-337.
- Rettinger G, Kirsche H. Complications in septoplasty. Arch Otolaryngol Head Neck Surg 1995;121:681-684.
- Ganessan S, Prior AJ, Rubin JS. Unexpected overnight admissions following day-case surgery: an analysis of a dedicated ENT day care unit. Ann R Coll Surg Engl 2000;82:327-330.
- Gulsen S, Yilmaz C, Aydin E, et al. Meningoencephalo- cele formation after nasal septoplasty and management of this complication. Turk Neurosurg 2008;40:185-188.
- Onerci TM, Ayhan K, Ogretmenoglu O. Two consecutive cases of cerebrospinal fluid rhinorrhea after septoplasty operation. Am J Otolaryngol 2004;25:354-356.
- Tawadros AM, Prahlow JA. Death related to nasal sur- gery: case report with review of therapy-related deaths. Am J Forensic Med Pathol 2008;29:260-264.
- Martin TJ, Loehrl TA. Endoscopic CSF leak repair. Curr Opin Otolaryngol Head Neck Surg 2007;15:35-39.
- Schwab JA, Pirsig W. Complications of septal surgery. Facial Plast Surg 1997;13:3-14.
- Makitie A, Aaltonen LM, Hytonen M, et al. Postoperative infection following nasal septoplasty. Acta Otolaryngol Suppl 2000;543:165-166.
- Okur E, Yildirim I, Aral M, et al. Bacteremia during open septorhinoplasty. Am J Rhinol 2006;20:36-39.
- Caniello M, Passerotti GH, Goto EY, et al. Antibiotics in septoplasty: is it necessary? Rev Bras Otorrinolaringol 2005;71:734-738.
- Allen ST, Liland JB, Nichols CG, et al. Toxic shock syn- drome associated with use of latex nasal packing. Arch Intern Med 1990;150:2587-2588.
- Huang IT, Podkomorska D, Murphy MN, et al. Toxic shock syndrome following septoplasty and partial turbi- nectomy. J Otolaryngol 1986;15:310-312.
- Cohen BJ, Johnson JD, Raff MJ. Septoplasty complicated by staphylococcal spinal osteomyelitis. Arch Intern Med 1985;145:556-557.
- Hari C, Marnane C, Wormald PJ. Quilting sutures for nasal septum. J Laryngol Otol 2008;122:522-523.
- Lee IN, Vukovic L. Hemostatic suture for septoplasty: how we do it. J Laryngol Otol 1988;17:54-56.
- Muhammad IA, Rahman Nabil-ur. Complications of sep- toplasty surgery. Facial Plast Surg 1997;13:3-14.
- Malki D, Quine SM, Pfleiderer AG. Nasal splints, revis- ited. J Laryngol Otol 1999;113:725-727.
- Guyuron B, Vaughan C. Evaluation of stents following septoplasty. Aesthetic Plast Surg 1995;19:75-77.
- Cook JA, Murrant NJ, Evans KL, et al. Intranasal splints and their effects on intranasal adhesions and septal sta- bility. Clin Otolaryngol Allied Sci 1992;17:24-27.
- Morre TD, Van Camp C, Clement PA. Results of the endo- nasal surgical closure of nasoseptal perforations. Acta Otolaryngol Belg 1995;49:263-267.
- Vuyk HD, Langenhuijsen KJ. Aesthetic sequelae of septo- plasty. Clin Otolaryngol Allied Sci 1997;22:226-232.
- Daudia A, Alkhaddour U, Sithole J, et al. A prospective objective study of the cosmetic sequelae of nasal septal surgery. Acta Otolaryngol 2006;126:1201-1205.
- Kim CS, Moon BK, Jung DH, Min YG. Correlation between nasal obstruction symptoms and objective parameters of acoustic rhinometry and rhinomanometry. Auris Nasus Larynx 1998;25:45-48.
- Newton JR, White PS, Lee MS. Nasal septal perforation repair using open septoplasty and unilateral bipedicled flaps. J Laryngol Otol 2003;117:52-55.
- Bateman ND, Woolford TJ. Informed consent for septal surgery: the evidence-base. J Laryngol Otol 2003;117:186- 189.
- Byrd SH, Salomon J, Flood J. Correction of the crooked nose. Plast Reconstr Surg 1998;102:2148-2157.
- Chandra RK, Rohman GT, Walsh WE. Anterior palate sensory impairment after septal surgery. Am J Rhinol 2008;22:68-88.
- Monteiro ML. Unilateral blindness as a complication of nasal septoplasty: case report. Arq Bras Oftalmol 2006;69:249-250.
- Bloom JD, Kaplan E, Bleier BS, Goldstein SA. Septoplasty complications: avoidance and management. Otolaryngol Clin North Am 2009;42:463-481.
- Jackson LE, Koch R, James MD. Controversies in the management of inferior turbinate hypertrophy: a comprehensive review. Plast Reconstr Surg 1999;103:300- 312.
- Lindemann J, Keck T, Wiesmiller KM, et al. Numerical simulation of intranasal air flow and temperature after resection of the turbinates. Rhinology 2005;43:24-28.
- Moore EJ, Kern EB. Atrophic rhinitis: a review of 242 cases. Am J Rhinol 2001;15:355-361.
- Dutt SN, Kameswaram M. The aetiology and management of atrophic rhinitis. J Laryngol Otol 2004;119:843-852.
- Stewart MG, Witsell DL, Smith TL, et al. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg 2004;130:157- 163.
- Dinis PB, Haider H. Septoplasty: long-term evaluation of results. Am J Otolaryngol 2002;23:85-90.
- Siegel NS, Gliklich RE, Taghizadeh F, Chang Y. Outcomes of septoplasty. Otolaryngol Head Neck Surg 2000;122:228-232.
- Harrill WC, Pillsbury HC, McGuirt F, Stewart MG. Radio- frequency turbinate reduction: a NOSE evaluation. Laryn- goscope 2007;117:1912-1919.
- Kemker B, Liu X, Gungor A, et al. Effect of nasal surgery on the nasal cavity as determined by acoustic rhinom- etry. Otolaryngol Head Neck Surg 1999;121:567-571.
- Reber M, Rahm F, Monnier P. The role of acoustic rhi- nometry in the pre- and postoperative evaluation of sur- gery for nasal obstruction. Rhinology 1998;36:184-187.
- Becker SS, Dobratz EJ, Stowell N, et al. Revision septo- plasty: review of sources of persistent nasal obstruction. Am J Rhinol 2008;22:440-444.
- Sipila J, Suonpaa J. A prospective study using rhino- manometry and patient clinical satisfaction to determine if objective measurements of nasal airway resistance can improve the quality of septoplasty. Eur Arch Otolaryngol 1997;254:387-390.
- Skouras A, Noussios G, Chouridis P, et al. Acoustic rhi- nometry to evaluate plastic surgery results of the nasal septum. B-ENT 2009;5:19-23.
- Grymer LF, Hilberg O, Elbrnd O, Pederson OF. Acoustic rhinometry: evaluation of the nasal cavity with septal deviations, before and after septoplasty. Laryngoscope 1989;99:1180-1187.
- Pirila T, Tikanto J. Unilateral and bilateral effects of nasal septum surgery demonstrated with acoustic rhinometry, rhinomanometry, and subjective assessment. Am J Rhi- nol 2001;15:127-133.
- Lindemann J, Keck T, Leiacker R, et al. Early influence of bilateral turbinoplasty combined with septoplasty on intranasal air conditioning. Am J Rhinol 2008;22:542- 545.
- Rhee JS, Poetker DM, Smith TL, et al. Nasal valve surgery improves disease specific quality of life. Laryngoscope 2005;115:437-440.
- Schwentner I, Dejakum K, Schmutzhard J, et al. Does nasal septal surgery improve quality of life? Acta Otolar- yngol 2006;126:752-757.
- Stewart MG, Smith TL, Weaver EM, et al. Outcomes after nasal septoplasty: results from the Nasal Obstruc- tion Septoplasty Effectiveness (NOSE) study. Otolaryngol Head Neck Surg 2004;130:283-290.
- Most SP. Analysis of outcomes after functional rhino- plasty using a disease-specific quality-of-life instrument. Arch Facial Plast Surg 2006;8:306-309.
- Arunchalam PS, Kitcher E, Gray J, Wilson JA. Nasal sep- tal surgery: evaluation of symptomatic and general health outcomes. Clin Otolaryngol Allied Sci 2001;26:36-70.
- Konstantinidis I, Triaridis S, Triaridis A, et al. Long term results following nasal septal surgery: focus on patient satisfaction. Auris Nasus Larynx 2005;32:369-374.
- Uppal S, Mistry H, Nadig S, et al. Evaluation of patient benefit from nasal septal surgery for nasal obstruction. Auris Nasus Larynx 2005;32:129-137.
- Joe SA. The assessment and treatment of nasal obstruc- tion after rhinoplasty. Facial Plast Surg Clin North Am 2004;12:451-458.
- Rinder CS. Fire safety in the operating room. Curr Opin Anaesthesiol 2008;21:790-795.
- Ashchi M, Widemann HP, James KB. Cardiac com- plication from use of cocaine and phenylephrine in nasal septoplasty. Arch Otolaryngol Head Neck Surg 1995;121:681-684.
- Georgalas C, Paun S, Zainal A, et al. Assessing day-case septorhinoplasty: prospective audit study using patient- based indices. J Laryngol Otol 2002;116:707-710.
- Bitar G, Mullis W, Jacobs W, et al. Safety and efficacy of office-based surgery with monitored anesthesia care/ sedation in 4778 consecutive plastic surgery procedures. Plast Reconstr Surg 2003;111:150-156.
- Hoefflin SM, Bornstein JB, Gordon M. General anesthe- sia in an office-based plastic surgery facility: a report on more than 23,000 consecutive office-based procedures under general anesthesia with no significant anesthetic complications. Plast Reconstr Surg 2001;107:243-248.
