Nasal reconstruction has historically been a challenging art for surgeons. Straddling the realm of aesthetics and anatomic function, rhinoplasties are temperamental procedures and leave little room for error. Of nasal repairs, saddle nose is not uncommon and remains challenging.
Resulting from a broad spectrum of etiologies, and presenting with a wide degree of variation and severity, saddle nose has always been a disputed art. First described by John Orlando Rose in 1887, called the “Pug-Nose,” the deformity is characterized by a distinctive scooped out appearance of the nasal dorsum resembling a horse saddle.
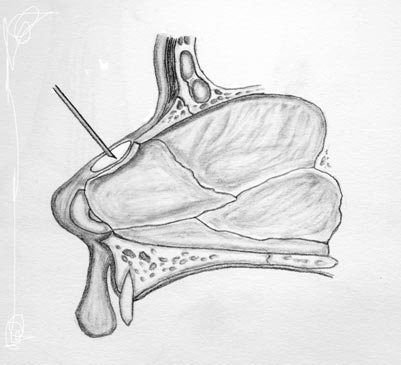
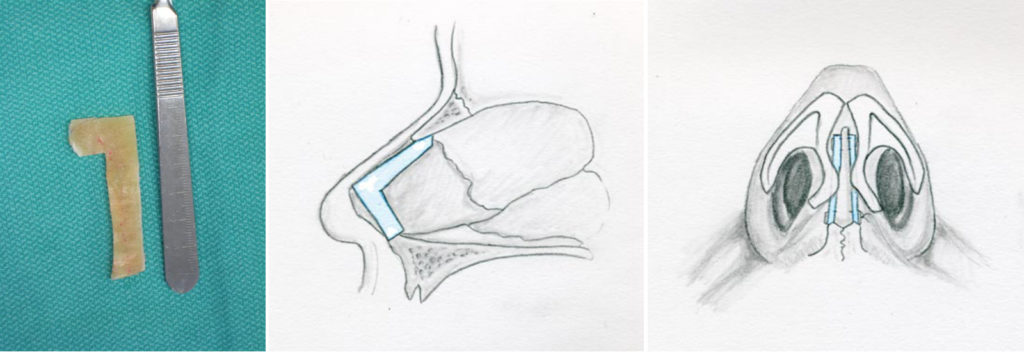
The shape represents a collapse of the intrinsic cartilaginous and/or bony support structures of the nose. Characteristics include a loss of dorsal height, middle vault and dorsal depression, a loss of tip support and definition, columellar retrusion, shortened vertical length, tip overrotation and retrusion of the nasal and caudal spine (image 1).
Many surgeons have proposed techniques to best repair a saddle nose. The first documented repair involved the implantation of the breastbone of a duck as a dorsal onlay graft.1 This was proposed by Robert F. Weir in 1892 to repair the cartilaginous damage seen in tertiary syphilis. Since then, multiple other methods have been described, each tailored to a specific patient subclass. In the following pages we will touch on the multitude of different approaches to Saddle Nose Repair.
Anatomy
Major structural support of the nose is performed by bony and cartilaginous anatomy. Bony components include the nasal bones, the bony portion of the intranasal septum, the pyriform aperture and the nasal floor. Cartilaginous components anchor to bony structures and provide a durable, yet flexible, component of nasal anatomy. This includes the cartilaginous portion of the nasal septum, which interlocks with the nasal bones and bony septum, forming a support wall for the middle vault and nasal tip. The upper lateral cartilages form the roof of the middle vault, and are supported almost entirely by the dorsal nasal septum. The lower lateral cartilages contribute to nasal tip projection and patency of the nasal valves.

The cartilaginous nasal septum requires special consideration in saddle nose deformity, as compromise of its integrity is one of the main factors leading to nasal dorsum collapse. The cartilaginous septum provides the main support for the structures of the caudal two-thirds of the nose. Seated on the septum are the upper and lower lateral cartilages, essential for maintaining nasal width, tip projection and nasal patency.
Two functional anatomic regions of consideration in saddle nose repair are the internal and external nasal valves. 2 The cross sectional area of these two regions largely determines the airflow through the nose. The internal nasal valve is formed by the junction of the upper lateral cartilage with the septum; anything affecting the angle of articulation between these two structures will potentially compromise airflow through this valve.
The external nasal valve is space under the alar lobule, often referred to as the vestibule. It is formed by the relationship between the nasal columella, sil, and alar lobule. This region is also highly dependent on support from the nasal septum.31 Thus collapse of the nasal septum can result not only in cosmetic deformity, but also a loss of nasal function.
It is important to note that the upper lateral cartilages arise from the dorsal septum, and are almost entirely dependent on the septum for support, besides some membranous connection to the lower lateral cartilages caudally and the nasal bones cephalad. In contrast, of the three major support mechanisms of the lower lateral cartilages (and subsequent tip position), only one relies on a connection to the septum. Thus, the loss of septal support is more noticeable in the middle 1/3rd of the nose compared to the tip region.
Etiology
There is an extremely broad differential of causes of nasal deformity. Broken down into categories (see Table 1):
Trauma:
Tramatic injury is one of the most common causes of nasal deformity. Nasal dorsum change can be caused from mechanical disruption of the structural integrity of the cartilage. A direct blow to the septum can lead to multiple fractures, many of which may sublux on themselves, creating loss in support and height. The mechanical disruption can lead to a saddle nose deformity. In addition, blunt trauma may lead to a septal hematoma and subsequent vascular compromise to the cartilage integrity (see below).
Iatrogenic:
Post operative deformity is a common complication of nasal surgery. Any disruption of the nasal floor, bony septum, nasal bones or dorsum of the nose can result in collapse.
Septoplasty usually involves the resection of a portion of the quadrangular cartilage. Though the overall risk of saddling is small (quoted somewhere between 0.4% and 3.4%) risk can be minimized by ensuring at least a 10-15mm strut of cartilage is left to support the dorsum and caudal border. 4-6 Anything less puts the patient at risk for dorsal collapse.
The etiology of deformity in cosmetic rhinoplasty is much more commonly due to over-resection of the nasal dorsum, rather than loss of intrinsic support.7 Daniel and colleagues found that the nasal septal support remains intact in over 75% of rhinoplasty patients.
Complicating the diagnosis, post-operative saddling is a progressive process, believed to finally stabilize 3-6 months after surgery. 7
Vasoconstrictors and Vascular Compromise:
Use of intranasal drugs can lead to destruction of the mucoperichondrium and ultimately necrosis of the septal cartilage leading to perforation. This can be seen with illicit drugs such as cocaine, but also over–the-counter vasoconstrictors such as oxymetazoline (found in topical decongestants such as Afrin).7 Saddling is also a progressive process and can continue long after drug abstinence is obtained.
A septal hematoma can follow blunt trauma to the nose and is an urgent matter. It can progress to an abscess and cause significant toxicity. The separation of the perichondrium from the cartilage will lead to complete vascular compromise and subsequent necrosis. While the mucosa may remain intact, a saddle nose deformity can still arise.
| Table 1: Etiologies of Saddle Nose Deformity3,7 | ||
| Examples | Mechanism of Deformity | |
| Traumatic | Physical comminution | Mechanical disruption of septum |
| Surgical | Over-resection of nasal dorsum or cartilagenous septum | Removal or compromise of major support structures of the nose |
| Vascular | Drugs, e.g. Cocaine, Oxymetazoline; septal hematoma | Potent vasoconstrictors or mechanical separation from perichondrium |
| Systemic Disorders | Wegener’s Granulomatosis, Sarcoidosis, Crohns Disease, Relapsing Polychondritis | Chronic inflammatory diseases resulting in damage to the support structures of the nose |
| Neoplasm | Inverted Papilloma, Squamous Cell Carcinoma | Invasion and destruction of support structures |
| Infectious | Syphillis, Leprosy, Septal Abscess | Infection and resorption of cartilage |
Systemic Disorders:
Systemic etiologies of nasal deformity are less common, but must be considered prior to reconstruction; overlooking a systemic disorder will adversely affect reconstructive outcomes. Wegener’s Granulomatosis is commonly considered, causing inflammatory destruction of cartilaginous structures. Other culprits include Relapsing Polychondritis, Sarcoidosis, and Crohn’s Disease.3 These should be ruled out with a serologic evaluation, CT scan, and/or biopsy if another cause of saddling is not readily apparent.
Neoplasm:
Local neoplasia can result in invasion and destruction of support structures of the nose.3 Common neoplasms resulting in nasal deformity include inverted papilloma and squamous cell carcinoma.
Infectious Disease:
Infectious etiologies are uncommon but should be considered. Syphillis and leprosy were frequent culprits before the turn of the century, and can be seen in patients coming from underserved areas. Septal abscesses can also cause septal destruction, and resultant deformity.
Classification
There have been multiple classification schemes proposed for saddle nose deformity, all emphasizing different aspects of the malformation.3 Seltzer introduced the Joseph classification scheme in 1949, which divided patients into three subtypes based on degree of nasal support and length.3,7 Tardy and colleagues proposed a similar, simplified three tier classification scheme known as the “Three “M” Classification (Mild, Moderate, Major), which were less specific to characteristics of the deformity, but more easily summed up the degree of malformation.
Vartanian and Thomas created a classification system that divided deformities into four categories based on the degree of existing anatomic deficit, stratifying noses into the amount of tissue shifting they would require during reconstruction.3 This was done by dividing the nasal dorsum into thirds and identifying deficits in each region.
A recent major classification system was proposed in 2006 by Daniel and Brenner (Table 2). Their system attempted to integrate the appearance of the external nose with the degree of septal support, and the most viable surgical repair. They divided saddle nose into six detailed categories, progressing from minor supratip depression and columellar retraction in Type 0, to loss of septal support and tip progression, to loss of cartilage vault integrity, and eventually to involvement of the bony vault with major reconstruction needed for repair.
| Table 2: Daniel and Brenner’s Saddle Nose Classification Scheme7 | |
| Type 0 – Pseudosaddle | Relative Depression of cartilaginous dorsum compared to bony dorsum A stable deformity, causitive process has ceased Septal support wall is solid, deformity is due to dorsal changes Septal support test is negative |
| Type I – Minor: Cosmetic Concealment | Minor decrease in septal support Greater supratip depression and columellar retraction Stable process Repair only requires augmentation of dorsum/columella with soft tissue and fascia or diced cartilage |
| Type II – Moderate: Cartilage Vault Reconstruction | Progressive weakening of septal support Cartilagenous middle vault begins to collapse Columellar retraction Loss of tip support Complaints of nasal obstruction secondary to internal nasal valve collapse Requires reconstruction of septal support wall and relationships to upper and lower lateral cartilage to restore contour and nasal valve function |
| Type III – Major: Composite Reconstruction | Obvious flattening and depression of the middle vault Damage to septal support wall, including septal perforation, septal disarticulation, and splaying of the ULC such that they are now only supported by the nasal bones Repair necessitates re-establishment of a stable support wall ULC and LLC often require more bolstering to maintain internal and external valves After valve patency is addressed, nasal contour can be repaired |
| Type IV – Structural Restoration | Deformity precludes re-establishment of normal support wall Middle vault depressed and splayed, altering configuration of internal nasal valve “Short Nose” – columellar retrusion with overrotation and deprojection of nasal tip Splayed Ala Loss or contraction of nasal lining complicates repair Functional obstruction – resulting from septal perforation, internal/external nasal valve collapse and/or compromised mucosal function |
| Type V – Catastrophic: Major Reconstruction | Requires total reconstruction of internal lining of nose and bony cartilaginous vault Adjacent tissues are also affected and require attention A large flap (such as a paramedian forehead flap) may be required to cover any new framework |
Methods Of Repair
The primary goal is to provide a stable and rigid support for the dorsum, restoring function, and achieving cosmetic goals. An individualized approach must be utilized with each patient since no two deformities are identical. Staging the patient’s deformity is useful to take stock of what anatomic structures remain what is functioning, and what needs to be augmented or replaced. Additionally, general treatment considerations should include etiology, and whether the causative process has ceased, or is ongoing. The patient’s occupation or hobbies may factor in as well. For example, a professional boxer has a high likelihood of re-injury, which is obviously considered prior to definitive reconstruction.
Functional and aesthetic goals must be addressed with all patients seeking saddle nose repair. Analysis of lateral views of the nose will help quantify and localize areas where cartilage and bone are deficient. Focus on the bony dorsum and tip position can help a surgeon extrapolate ideal nasal contour.8 Intranasal examination is important to assess the patency of the internal valve area, identify septal perforations, and further quantify the extent of the structural defect.
The integrity of the nasal support can be assessed by palpation of the nasal dorsum. The amount of resistance or recoil can allow a surgeon to gauge the compromise in dorsal support.3
Finally, the skin and mucosal lining of the nose should be assessed, in case there is not enough to cover a potential repair. 8 If the existing nasal lining cannot expand to adequately cover the reconstructed nose, additional tissue may have to be recruited in the form of local flaps, skin grafts, or composite grafts.
Grafting Materials
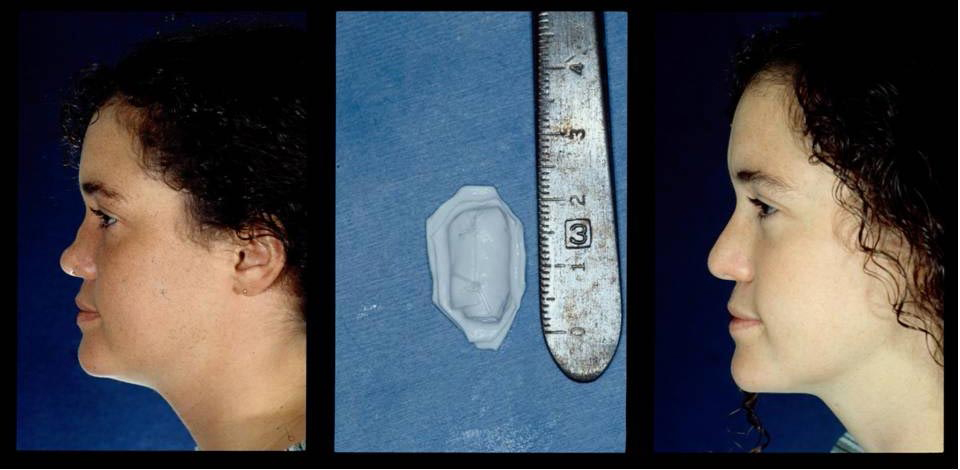
Injectables
While not endorsed by the authors, injectable soft tissue fillers offer a less expensive, in-office alternative to surgical repair of smaller saddle nose deformities . They are able to fill minor tissue defects, and are especially useful in correction of post-rhinoplasty asymmetry (image 2). The “catch” of injectable fillers is that they are temporary, must be replaced at regular intervals to maintain the aesthetic effects, and should not be used in the lower 1/3rd of the nose. Of note, this treatment method is controversial, and has been associated with small vessel thrombosis, skin necrosis, infection, and granuloma formation.9 Silicone in particular has been identified as putting the patient at significant risk of necrosis, and risks verses benefits should be carefully weighed before use. However, its role may become more defined in the future and the practitioner should be familiar with the current fillers and techniques.
Implants
North first defined the ideal characteristics for an implantable material in facial reconstruction in 1953.10,11 A graft should be easily obtainable, well tolerated by the tissues of the host site, show no
tendency to perforate through skin or mucous membranes even in areas prone to repeated minor trauma (such as the nose), and it should not show tendency to distort or resorb. Over the last century, surgeons have attempted to meet these criteria with a wide variety of materials in the face.
Xenografts
Harvested from non-human sources, these have been historically popular areas of investigation, but for the most part are not recommended for nasal reconstruction.3,10 Implantation of bovine cartilage resulted in intense inflammatory reactions and high rates of resorption.3 Some studies have explored the use of porcine small intestinal mucosa (PSIS) for nasal septal perforations with mixed results.
Alloplasts:
Advantageous in that no donor is required, several different substances have been tried for implantation into the body.3 Requirements include a substance that’s nontoxic and nonallergenic, easy to sculpt and sterilize, and a substance that resists resorption, rejection and extrusion. These should not be used in patients with a systemic chondritis or other reactive process, as these patients will be at an increased risk for implant rejection. Best results are obtained with deformities in the earliest stages.
Plastic: Tends to be well tolerated in the body, and is non immunogenic. Infection poses a serious threat to the graft, however, and can lead to extrusion.3 Plastics tend to be hard and immobile as well, and can shift with trauma.
Silicone: Silicone is the most commonly used alloplast in the nose due to its widespread use in Asia. It is a biologically inert polymer that induces a fibrous capsule around itself when implanted in the body. This capsule helps keep implants in place, which is advantageous in many parts of the body.3 Silicone is easy to use, can be manufactured in almost any consistency, and is easy to remove if revision is necessary. In the face, however, a significant percentage of silicone implants will shift, buckle, or extrude, and many require replacement.
High-Density Porous Polyethylene: Medpor (Porex Medical, Fairburn Ga.) offers a highly porous, noncompressible, somewhat flexible augmentation material that can be easily carved for nasal augmentation. The product has the ability of being malleable when submerged in hot saline (80-100 degrees C) for several minutes, then retaining its shape permanently.12 The highly porous nature allows for fibrous tissue ingrowth and phagocyte access to the graft, allowing for lower rates of shifting and infection respectively. The heavy ingrowth of surrounding tissue may make future removal of the graft challenging during revision surgery.
Polytetrafluoroethylene: A synthetic polymer of tetrafluoroethylene, best known as its DuPont brand name Teflon, can be used to fill minor nasal soft tissue defects.3 A drawback of this polymer’s use is that it seems to be prone to infection, and proper implantation requires meticulous handling during implantation and perioperative antibiotics. Long term follow up is essential to monitor future infection, rejection and fistula formation.
Expanded Polytetrafluoroethylene (Gore-Tex): Gor-Tex (e-Polytetrafluoroethylene) (W.L. Gore Associates, Flagstaff, Ariz) was introduced in 1993 as medical filler, and has provided surgeons with a pliable, natural feeling material ideal for dorsal augmentation. 13 Gore-Tex comes in multiple thicknesses, and can be carved with a scalpel to the correct shape. Disadvantages include a possible increased risk for infection and extrusion due to the limited tissue ingrowth.
| Table 3: Grafting Materials | |||
| Definition | Pros | Cons | |
| Injectables | Filler substances that can be injected dermally or subdermally to correct minor cosmetic deformities | Inexpensive, available in-office, no need for general anesthesia, immediate results | Temporary, must be re-administered at regular intervals Significant complication rates including small vessel thrombosis, skin necrosis, infection and granuloma formation Should not be used in lower third of the nose |
| Xenografts | Grafts harvested from non-human species, such as bovine cartilage or porcine small intestine | Easily obtained, abundant sources | High rates of resorption and intense inflammatory reactions to most grafts |
| Alloplasts | Non-organic grafting materials composed of a wide variety of compounds, such as plastic, silicone, and polytetrafluoroethylene | No donor required, abundant, frequently very moldable, a wide variety of characteristics available | Higher rates of rejection and extrusion, infection is a concern, cannot be used in patients with a systemic chondritis, as they are at an increased risk for implant rejection |
| Autografts | Grafts taken from a donor site on the recipient, including septal, conchal and costal cartilage, and calvarial bone | The gold standard in grafting due to lowest rates of extrusion and resorption, perfect immunogenicity | Additional scars, multiple operative fields, longer operative times, additional potential complications |
| Homografts | Grafts donated from a member of the same species, examples in rhinoplasty include cadaveric costal cartilage | Offer many of the same advantages as autografts without the added harvest risk. | Debates regarding resorption rates, some say all eventually resorb completely |
Autografts
Autografts will always represent the gold standard for human implantation. Advantages include the lowest rates of extrusion and resorption, and perfect immunogenicity. Unfortunately, the use of autografts frequently requires multiple operative fields, prolonged anesthesia time, and additional scars and complications from the donor sites.
Nasal reconstruction frequently uses either autologous bone and/or cartilage. There are multiple potential donor sites, each with their own characteristics.
Cartilage Autografts:
Septal Cartilage: The nasal septum is a preferred site since it is in the same operative field. It is firm and flexible and can be used to provide significant structural support to the compromised nose in most patients. Unfortunately, in many saddle nose patients the quantity or quality of remaining septal cartilage is insufficient and jeopardizes further destabilization.
Conchal Cartilage: Cartilage from the ear can also be safely harvested without cosmetic deformity as long as the antihelical rim is left intact. This cartilage tends to be more maleable and better suited for secondary support rather than providing a central structural foundation for the nose. Its curved shape makes it less useful for many types of caudal struts
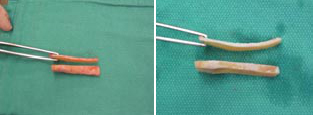
Costal Cartilage: Cartilaginous ribs provide an abundant source of stiff cartilage that is utilized for many reconstructions requiring a larger graft (image 3). 2 The structural properties of costal cartilage allow its use in larger reconstructions, and extra material can be banked in a posterior auricular pocket for future use. Harvesting does require an additional surgical field, however, as well as prolonged operative and anesthesia time.
The procedure is associated with other unlikely complications, such as pneumothorax, chest deformity and post-operative pain. Cartilaginous ribs also continue to ossify as we age, so autologous costal grafts may not be an option for cartilage in older patients.14
Studies suggest that when harvesting cartilage, grafts cut from the center of the rib show fewer propensities for warping than those cut from the periphery. Bone can also be harvested from the rib if necessary (Image 3).
Bone Autografts: Bone can be harvested from the calvarium, rib, septum, or illium, and provides a rigid structure for reconstruction.10 It is more metabolically active than cartilage, however, and can be prone to resorption. Bone is used less frequently than cartilage in saddle nose repair as the rigidity leaves an unnatural feel that can be problematic, especially from minor trauma. It can be used for major repair and drilled into the existing frontal or nasal bones.
Split Calvarial Bone: Bone grafts offer an enticing stability to an unstable deformity. They resist deformity due to contraction and scarring after reconstruction, provide good stability and are available in abundance. Split calvarial bone has emerged as a preferred graft, with low rates of donor site morbidity, superior strength, and a lower resorption rate when compared to other sites. The dense cortex allows calvarial bone to be thinned to 1mm and arranged in an L-configuration to provide both dorsal support and tip projection. Drawbacks include an unnatural feel in some cases, and potential prolonged donor site pain. Central nervous system injury, although rare, has been documented.
Osseocartilaginous Rib Graft: As mentioned earlier, bone can also be harvest from rib when the dissection is carried more laterally along the rib. Some surgeons will utilize the natural osseocartilaginous junction within the graft to create a chimeric implant that replaces like with like: the bony portion overlies the nasal bones, and cartilage overlies the lower cartilaginous dorsum.
Homografts
Homografts are from another individual of the same species. Grafts are harvested from cadavers and are usually costal cartilage. They have the advantage of abundance over autologous grafts, and do not share the same risk of donor site morbidity. If prepared correctly, they carry no risk of antigenic response. The antigenicity of cartilage is mediated by class II antigens that exist on the perichondrium.10 These can be destroyed by either removing the perichondrium or irradiating the graft with gamma radiation.
Irradiation of the graft is a method to sterilize and preserve cartilage.10,14 This has not shown to change the structural properties of the graft, such as warping, when compared to non-irradiated cartilage.
There has been debate regarding the efficacy of homologous costal cartilage grafts.10,15 The potential benefit of homografts are huge; a large donor pool allows the use of young, non-ossified costal cartilage, and the lack of a second surgical site for harvesting avoids potential surgical complications. Resorption compared to autografts is the main point of contention.7 Opponents of homografts state that cadaveric cartilage is rarely an acceptable option for reconstruction, citing reports of near total resorption as late as 15 years post implantation.16 Welling and colleagues claimed that complete resorption of the graft should be expected, though rates of resorption remain variable. This would suggest that irradiated homografts should be contraindicated in reconstructions requiring support. Of note, many of the studied grafts were replaced by fibrous tissue, which maintained the cosmetic benefit, but did not provide the same support as cartilage.17 This may account for the discrepancy in patient satisfaction when these grafts are used for auricular reconstruction, where shaper margins are critical for accurate definition, in contrast to the nose where the implant serves as a filler.
A recent study by Kridel and colleagues, long term advocates of homografts, describe a retrospective review of patients whom had undergone irradiated homologous costal cartilage grafting.10 Their follow up extended to 24 years after grafting. They evaluated 1025 IHCC grafts for warping, infection, infective and non-infective resorption, mobility and extrusion, and comparing them to autografts performed by the same surgeon. Results of the study yielded equivalent rates of warping and infection. Complication rates were much lower in patients receiving homografts (2.46% vs 8%) due to the lack of a secondary surgical site.
Alloderm (acellular cadaveric dermal matrix) is an example of a non-cartilagenous homograft, useful in certain reconstructions. The pre-implantation treatment ablates viable cells and yields a highly biocompatible implant. Partial resorption occurs and some surgeons attempt to over-correct the deformity. Septal perforations in saddle nose deformity can be addressed with these grafts.
Surgical Techniques
Surgical techniques have a variety of clinical applications and can be used in a variety of situations. Some surgeons are comfortable with only one or a few methods of recreating the nasal dorsum, and will apply their technique to various types of saddles by varying the size of the graft used in their technique. However, some techniques are better suited for repair of a small saddle, while others are more appropriate for major repair. While not universally limited to repairing a single type of saddle (minor vs major), it is useful to categorize the various types of reconstructions by their general application.
Minor Dorsal Augmentation
Less severe deformities tend to fall more in the aesthetic than functional reconstruction category. Septal support usually remains intact, and repair is focused on augmentation of the nasal dorsum and columella. There are several described ways to approach such deformities.
Injectable Fillers
Injectable soft tissue fillers are sometimes an option for minor dorsal augmentation.10 As described in detail previously, they have the advantage of low cost and convenience, but must be repeated at regular intervals to maintain repair. Injectable fillers are strictly considered for only minor soft tissue defects, such as post rhinoplasty asymmetries and contour irregularietis.
Good candidates for injectable fillers are patients that would prefer to avoid surgery, have thick skin, and have deformities that do not involve the nasal tip or the alae.9 The dorsum and sidewalls of the nose are generally considered safest to treat with injectable augmentation agents as vascular compromise is rarely seen in these areas.
In general, the smallest needle tip the agent will flow through is preferable, as it limits patient discomfort and maximizes precision of placement. Techniques for injection include fanning, threading and serial microdroplet methods.
Fanning involves injection of filler material with several passes over an area, at perpendicular angles to maximally camouflage filler. Threading involves laying down thin lines of the material by inserting the needle perpendicular to the skin surface and retracting while injecting, leaving a thin band of material. Serial droplet deposition is performed by injecting multiple miniscule droplets with separate needle insertions, which is great for correction of spot deformities with HA or CaHA.9
The modified serial droplet technique, termed the “microdroplet” technique can be used for silicone, injecting 0.01ml per droplet.18 Any more than this puts the patient at risk for a severe granulomatous reaction.9 As with HA, undercorrection is important with silicone as a fibroblastic reaction is seen in the corrected area weeks to months after treatment.
While fast, convenient, and inexpensive, injectable filler materials may seem like great options to patients with minor cosmetic saddling deformities without functional compromise. Their repair capability is limited, however, and they are not without risk. Careful thought should be given to the decision, and all potential complications described to patients.
Dorsal Camouflage Graft
Even minor depressions are amenable to other techniques. It is relatively straight forward to implant a small disk of crushed cartilage through a stab incision endonasally. Other materials can be inserted this way as well.
Diced cartilage has been described as a filler material. The cartilage is usually harvested from the septum, and inserted into the depressed area. When inserted alone, some surgeons run into complications with shifting, despite placement in a secure pocket.3 Patients will frequently complain of palpable irregularities over the repair.
Moderate Dorsal Augmentation
Moderate Saddle noses (Daniel and Brenner types II, III) have lost significant structural support and most patients have a functional component that needs to be addressed. However, if patients do not complain of nasal obstruction, and there is no need to resuspend the upper lateral cartilages, one can still consider larger camouflage grafts.
Dorsal Onlay Grafts:
Dorsal onlay grafts provide moderate augmentation of the nasal dorsum. This technique involves placement of a filler material or graft along the dorsal surface of the nasal cartilage to restore natural dorsal contour.
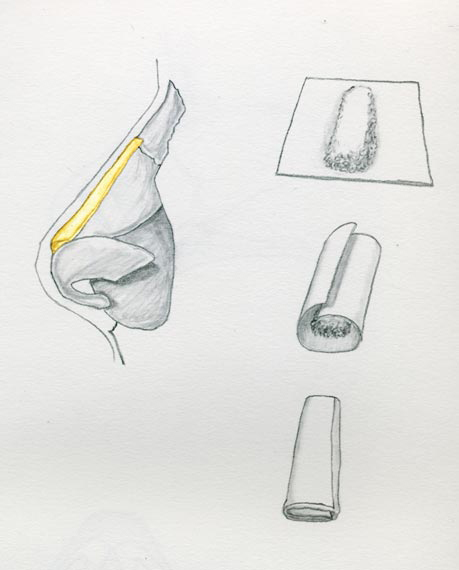
When used for a more significant saddle repair, the amount of diced cartilage required can leave palpable irregularities along the dorsum. One proposed solution to this has been wrapping the diced cartilage in a sheet of material before insertion.
Erol described wrapping the graft material in Surgicel (polyanhydroglucuronic acid), which he dubbed “Turkish Delight (Image 4).”19 He reports using this graft to fill minor dorsal contour irregularities, including post rhinoplasty imperfections.19 The wrapping prevents post-operative palpation and irregularities, while it holds the diced cartilage in place well enough for the surgeon to mold the graft with his or her fingers. A degree of resorption can occur and require minor overcorrection. Polyanhydroglucouronic acid has been described to cause a foreign body reaction by some studies.
Temporalis fascia has been described as another wrapping material. Providing a stable pocket for the diced graft, fascia demonstrates minimal resorption while retaining the regenerative capacity of the cartilage.3 Daniel and colleagues found that fascial grafts provide a smooth dorsal contour with minimal resorption, decreasing the need for initial overcorrection.
Dorsal onlay grafting is also frequently performed with stiff grafts, such as non-crushsed cartilage.
Used in patients with intact septal support, a cartilaginous graft can help restore dorsal contour. The graft is carved in the shape of a shallow canoe, and tapered at both ends. A sub-periosteal pocket is tunneled over the nasal bones cephalically, and the graft is inserted to prevent lateral migration during the healing process.8 Care must be taken in thin-skinned patients to adequately taper dorsal onlay grafts to prevent palpation or visible graft margins. If significant tip support is required, an integrated graft should be used, with a columellar strut to provide tip support.
Endonasal Spreader Grafts:
Most patients with a moderately sized saddle will require more than camouflage grafting, and need to have structural components addressed.
Minor structural reconstruction can be addressed with an interposition spreader graft sandwiched between bilateral mucoperichondrial advancement flaps. This can be performed endonasally through a small incision in the septal mucosa and insertion of a cartilaginous graft interposed onto the existing nasal septum. Discrepancies in mucoperichondrium are addressed by creating advancement flaps from the nasal floor and superior portion of the septum. This is useful in patients with a relatively stable, well-supported nose that is lacking in dorsal height.
Dorsal Spreader Grafts:
More significant dorsal reconstruction requires more significant grafts.
Spreader Grafts are the workhorses of major dorsal augmentation.They can be a simple onlay graft or can be integrated with the existing septum and upper lateral cartilages. These are frequently composed of costal cartilage, and carved intraoperatively into 20-25mm x 3mm struts. Proximally, they are secured to the nasal bones. Distally, they are frequently sutured to a columellar strut (Image 5).
Columellar struts are used to restore nasal height, rotate the nasal tip inferiorly and provide support for the entire lobule.7 These are inserted between the lower lateral cartilages and secured to the anterior nasal spine. It is then secured superiorly to the distal end of the septal strut to create an L-shaped graft (Image 6).
Different grafts provide a variable amount of support and projection. One can add nasal length to the nose as well and the powerful caudal extension graft is very useful for this. This combination of a spreader grafts affixed to a columellar strut creates an L-shaped graft that determines the basic dorsal profile of the nose.
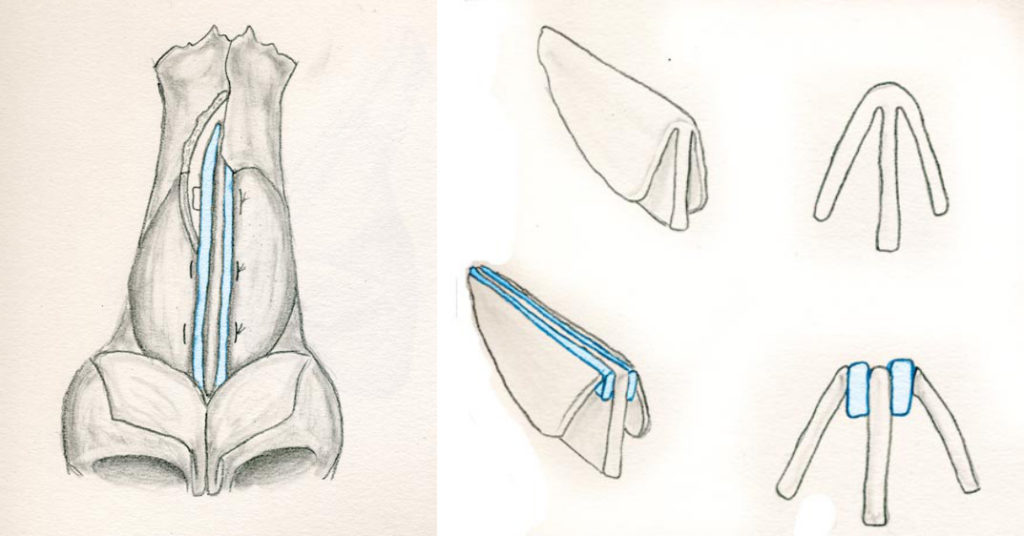
Septal Replacement Graft:
When using rib, it is possible to create the L-shaped graft out of one piece of cartilage. (Image 5) Once this is achieved, additional modifications can performed to tweak the repair. The ULC and LLC are secured to the new struts to reconstruct the ceiling of the middle vault and the nasal tip.20
Additional tip modifications can be made with sutures or tip grafts to achieve desired projection.
Variations to this approach have been discussed in the literature. Daniel and colleagues advocate the replacement of a columellar strut secured to the anterior nasal spine with an extended spreader (or “pistol”) graft to support the lobule.7
This graft is split on one end, and designed to straddle the anterior nasal spine to hold it in place. A shield graft here can provide much needed definition and natural contours to the tip.
Mirror Image Costal Cartilage Spreader Grafts
Ahmed and colleagues have written a specific reconstructive technique geared towards minimizing warping of grafts. They’ve settled on costal cartilage as the ideal grafting material, stating that it meets both rigidity criteria (unlike conchal cartilage) and longevity criteria (low rates of extrusion, infection and resorption). The only issue with costal cartilage is its tendency to warp after carving. 90% of warping happens in the first 60 minutes after harvesting, with the remaining 10% of shape change occurring slowly over the next 4 months. Ahmed combats this with his idea of mirror image spreader grafts.
The technique involves shaving two spreader grafts from either side of a harvested rib graft, which immediately bow upon being released from tension. The originial graft is used as a septal strut, secured to the anterior nasal spine and oriented in line with the columella. The two spreader grafts are secured to either side of the ventral portion of the strut, extending cephalically to create the “L” shaped graft that is commonly used in saddle reconstruction. Ahmed’s dorsal spreader grafts, however, naturally bow away from each other in the middle portion, “kissing” at both ends. These grafts are secured to either side of the nasal dorsum, their opposing bowing forces counteracting any warping. These are positioned just above the lower lateral cartilage, lending more height to the middle third of the nose, with the upper lateral cartilage secured to the graft. Minor imperfections are then addressed with soft tissue grafts or bruised cartilage.21 They boast no incidence of graft warping, visibility or displacement in 14 patients this has been performed in.
Major Dorsal Augmentation
More severe deformities are associated with a loss of structural support as well as external dorsal collapse. Both aspects should be addressed simultaneously.
Repairs focus first on restoring support to the nose. Once this has been corrected, aesthetic components of the repair can be addressed. There are several potential solutions to restoring the middle vault, but the fundamental tenet remains the same: a large graft to recreate the nasal dorsum strong enough to resuspend the contracted soft tissue of the nose. This amount of support often requires cantilevering the graft off the frontal bones, articulating it with a rigid columellar reconstruction, and potentially rebuilding the premaxilla. Regardless of the grafting material used, the upper lateral cartilages must be resuspended to the lateral aspect of the spreader grafts.
Dorsal Onlay Spreader Graft:
Christophel and Hilger noted that an osseocartilaginous rib graft had improved viability compared to a cartilaginous only graft when used as an onlay spreader for major dorsal reconstruction.22 This graft replaces like with like: the bony portion overlies the nasal bones, and cartilage overlies the lower cartilaginous dorsum (Image 7). The bone over the dorsum allows for bony fusion and integration with the nasal bones and does not have the potential to warp. The cartilage portion at the tip allows the surgeon to carve the implant and to attach the lower lateral cartilages using suture techniques.

Mutaf and colleagues proposed a reconstructive technique involving an autogeneous osteocartilagenous rib graft. Their theory is that using a costal graft that includes a portion of the ossified rib will allow for a more natural reconstruction. The process involves orienting the cartilaginous portion of the rib graft distally, and elevating a columellar strut from the graft to form an “L”. The remaining graft is then carved to resemble the missing nasal components; a concave roof the resemble the LLC, thinning of the distal end to allow tip mobility, slits along the columellar strut to allow more movement, and sculpture of the proximal bony component to resemble nasal bones. The structure is then secured to the existing bony anatomy proximally with K-wires, with the columellar strut secured to the anterior nasal spine via an upper buccal sulcus incision distally.23
Mutaf reports that repairing saddle nose with this anatomic replica effectively restores all anatomic and functional features to the nose. When repairing major saddle deformities, it is important to consider simultaneous reconstruction of the lateral nasal wall and/or external valve. The lateral nasal wall is commonly reconstructed with batten grafts, often composed of either conchal or costal cartilage. These are secured at the superolateral border of the lateral crura and positioned over the piriform aperture.
The external valve can be reconstructed with alar rim/lobule grafts. These are secured along the caudal border of the lower lateral cartilage and inserted into the alar soft tissues, lending support to the vestibule.
Special Considerations
Other surgeons have proposed more complex reconstructive techniques attempting to replicate more exactly missing nasal anatomy.
Cocaine Nose
Daniel and colleagues give special mention to the repair of cocaine nose. Because of the vasoconstrictive effects of cocaine, these patients will frequently start with a septal perforation that progress into complete cartilaginous destruction, with a relatively intact bony vault.7 These patients frequently require larger columellar/septal struts to restore stability to the nose. As a general rule, the soft tissue condition of the nose is unhealthy and unpredictable. Unlike a traumatic injury where the remaining lining is normal and healthy, the cocaine nose represents marginal tissue that survived but will not respond to stress. Major reconstruction and augmentation can lead to further soft tissue necrosis and exposure of grafts and implants. On occasion, a healthy, vascularized soft tissue flap must be brought into the field.
Granulomatous Disease
In saddle repairs involving patients with a systemic inflammatory process, care should be taken to ensure that the disease progression has ceased. A rheumatology consult should be obtained to better define the patient’s disease state. Alloplasts should be avoided in these patients as they are at a higher risk for extrusion.
Severely Retracted Lining
In cases of severely retracted nasal skin or lining, skin can be taken from other areas to cover the internal defect. Many times the retracted internal lining that correlates with the external appearance of a saddle nose will be the limiting factor. There are a host of options for repairing the internal lining defect, not unlike the methodology of major nasal reconstruction for Mohs surgery. Even a forehead flap can be mobilized to provide epithelium for the nose, both internal and external.
Premaxillary Grafts
Childhood nasal injuries can result in midface hypoplasia, as septal growth is responsible for outgrowth of the bony and cartilaginous pyramid, lobule and midface. Severe trauma in adults can also affect premaxillary position.
A depressed premaxilla can compound nasal deformities; without a strong platform for projection, the columella will appear more retracted. This can also affect nasal dorsum contour and tip projection.
Augmentation of the premaxilla can be performed at the same surgery as the nasal reconstruction with a direct graft placed through an external rhinoplasty approach.24 Seyhan suggests a combined external open rhinoplasty and intraoral approach using crescent shaped autogenous rib cartilage, citing a one-stage approach with good functional and cosmetic results. There are also more involved procedures such as Le Fort osteotomies or various distraction methods.
Case Studies
Case 1.
A 20 year old woman with a typical saddle nose deformity. She had declined autogenous materials for correction.
The middle vault was augmented with stacked sheets of ePTFE (Gore-Tex). This was inserted endonasally. Two years postoperatively, the dorsum is well aligned (Figure A).
Case 2.
32 year old gentleman with nasal obstruction following trauma as a child. He developed collapse to the upper and middle third of his nose.
Costal cartilage was carved to re-create an onlay graft, coupled with a strong columellar strut. These were suture secured and implanted via an external approach.
18 months postoperatively, he maintained improved projection and nasal function.





Case 3.
A 60 year old woman with a history of advanced Wegener’s Granulomatosis that has become quiescent. She developed total collapse of her nose with associated complete bilateral nasal obstruction. Reconstruction utilized split calvarial bone for rigid dorsal support. In addition, she had a strong columellar strut and lateral batten grafts. Two years postoperatively, she maintained sufficient projection and a significant improvement in nasal function.



Conclusion
Saddle nose deformity is a common yet challenging deformity, with a multitude of etiologies and a wide range of reconstruction options. When attempting a repair, each case must be evaluated individually, and the pros and cons of individual methods weighed. Each patient should receive a thorough evaluation, taking stock in remaining structures, exact etiology, and severity, in order to best select a reconstructive method. While methods vary and different grafting materials are widely described, autogenous autografts still remain the gold standard for saddle nose repair.
Works Cited:
1. Weir RF. On restoring sunken noses without scarring the face. 1892. Aesthetic Plast Surg. 1988;12(4):203-206.
2. Gassner HG, Friedman O, Sherris DA, Kern EB. An alternative method of middle vault reconstruction. Arch Facial Plast Surg. 2006;8(6):432-435.
3. Pribitkin EA, Ezzat WH. Classification and treatment of the saddle nose deformity. Otolaryngol Clin North Am. 2009;42(3):437-461.
4. Yanagisawa E, Ho SY. Unintended middle turbinectomy during septoplasty. Ear Nose Throat J. 1998;77(5):368-369.
5. Yeo NK, Jang YJ. Rhinoplasty to correct nasal deformities in postseptoplasty patients. Am J Rhinol Allergy. 2009;23(5):540-545.
6. Ketcham AS, Han JK. Complications and management of septoplasty. Otolaryngol Clin North Am. 2010;43(4):897-904.
7. Daniel RK, Brenner KA. Saddle nose deformity: A new classification and treatment. Facial Plast Surg Clin North Am. 2006;14(4):301-12, vi.
8. Kim DW, Toriumi DM. Management of posttraumatic nasal deformities: the crooked nose and the saddle nose. Facial Plast Surg Clin North Am. 2004;12(1):111-132.
9. Humphrey CD, Arkins JP, Dayan SH. Soft tissue fillers in the nose. Aesthet Surg J. 2009;29(6):477-484.
10. Kridel RW, Ashoori F, Liu ES, Hart CG. Long-term use and follow-up of irradiated homologous costal cartilage grafts in the nose. Arch Facial Plast Surg. 2009;11(6):378-394.
11. NORTH JF. The use of preserved bovine cartilage in plastic surgery. Plast Reconstr Surg (1946). 1953;11(4):261-274.
12. Sajjadian A, Rubinstein R, Naghshineh N. Current status of grafts and implants in rhinoplasty: part I. Autologous grafts. Plast Reconstr Surg. 2010;125(2):40e-49e.
13. Sajjadian A, Naghshineh N, Rubinstein R. Current status of grafts and implants in rhinoplasty: Part II. Homologous grafts and allogenic implants. Plast Reconstr Surg. 2010;125(3):99e-109e.
14. Adams WP,Jr, Rohrich RJ, Gunter JP, Clark CP, Robinson JB,Jr. The rate of warping in irradiated and nonirradiated homograft rib cartilage: a controlled comparison and clinical implications. Plast Reconstr Surg. 1999;103(1):265-270.
15. Song HM, Lee BJ, Jang YJ. Processed costal cartilage homograft in rhinoplasty: the Asan Medical Center experience. Arch Otolaryngol Head Neck Surg. 2008;134(5):485-489.
16. Welling DB, Maves MD, Schuller DE, Bardach J. Irradiated homologous cartilage grafts. Long-term results. Arch Otolaryngol Head Neck Surg. 1988;114(3):291-295.
17. Burke AJ, Wang TD, Cook TA. Irradiated homograft rib cartilage in facial reconstruction. Arch Facial Plast Surg. 2004;6(5):334-341.
18. Webster RC, Hamdan US, Gaunt JM, Fuleihan NS, Smith RC. Rhinoplastic revisions with injectable silicone. Arch Otolaryngol Head Neck Surg. 1986;112(3):269-276.
19. Erol OO. The Turkish delight: a pliable graft for rhinoplasty. Plast Reconstr Surg. 2000;105(6):2229-41; discussion 2242-3.
20. Sheen JH. Tip graft: a 20-year retrospective. Plast Reconstr Surg. 1993;91(1):48-63.
21. Ahmed A, Imani P, Vuyk HD. Reconstruction of significant saddle nose deformity using autogenous costal cartilage graft with incorporated mirror image spreader grafts. Laryngoscope. 2010;120(3):491-494.
22. Christophel JJ, Hilger PA. Osseocartilaginous Rib Graft Rhinoplasty: A Stable, Predictable Technique for Major Dorsal Reconstruction. Arch Facial Plast Surg. 2010.
23. Mutaf M. The anatomic replication technique (ART): a new approach in saddle nose correction. Ann Plast Surg. 2008;61(2):169-177.
24. Seyhan T. Correction of major saddle nose deformities with nasomaxillary depression using an intraoral and external open rhinoplasty approach. Aesthetic Plast Surg. 2010;34(5):587-595.
