It is generally agreed that autologous tissue is the material of choice for the rhinoplasty.
Alloplastic materials are inherently subject to risks of bacterial infection, extrusion, migration and other problems.
However, it is often overly emphasized or exaggerated for the risks of alloplastic materials by experts. Complications from alloplastic implants in rhinoplasty may decrease with the degree of experience of the surgeon as other complications of rhinoplasty.
The reported complication rates for alloplastic implants in various articles are mixed results of different surgeons with different levels of experience in dealing with alloplastic implants.1)
When they are carefully used with adequate precautions, alloplastic implants can be safely used in a medically acceptable range of complication rates.
There are minor but relatively frequent complications of alloplasts such as deviation and mobility which can be corrected without so much difficulty. However, there are some serious complications such as infection, extrusion, and contraction which must be treated promptly and decisively, but fortunately those complications are extremely rare for experienced surgeons.
Because of known complications from alloplasts, there is increasing demand from patients to use autologous materials only for rhinoplasty even in Asian countries recently.
Various autologous materials, such as dermis, fascia, fat and cartilages are used for nasal dorsal augmentation. Among them, rib cartilage is the most frequently used autologous material for dorsal augmentation, and dorsal augmentation with diced rib cartilages which are wrapped or glued is getting more and more popularity in Asian countries also.2)
Nonetheless, alloplastic implants have some clear advantages over autologous materials.
When viewed from the purely aesthetic standpoint, alloplasts are superior to autologous materials. There is no absorption, surface irregularity, serious deformation and warping. Carving of implants is much easier. Practically there is no limitation for the amount of augmentation. Alloplasts are relatively inexpensive and ready to use. There is no additional incisions and donor site morbidity with decreased recovery time.
Rhinoplasty is the one of the most common aesthetic procedures in Asian countries and therefore, aesthetic standards of patients are commonly high. However, the required amount of dorsal augmentation is substantial in many patients which is extremely difficult to provide with autologous materials, except for rib cartilages.
However rib cartilages are not immune to complications and related to numbers of problems also.
Use of rib cartilage is related to chest scarring, possible pneumothorax, prolonged operation time, and increased emotional or economic burden of the patient. The rigid immobile tip made of rib cartilages is often odd and unpleasing. Warping is frequent even with careful delicate carving and tension-releasing incisions. Resorption is often observed and infection is also possible even though uncommon. Because of its solid nature it may get fractured more easily by trauma than other materials for rhinoplasty.3)
Therefore, use of rib cartilage in a primary aesthetic rhinoplasty should be evaluated carefully on the benefits and costs, patient’s comfort level, and likelihood of overtreatment.
Recently diced rib cartilages are frequently used because they are free of warping. However, for diced rib cartilages, resorption, surface irregularity, insufficient volume, difficult shaping, increased operation time and difficult revision operation are the frequent concerns.4)
Revision surgeries are often requested by patients according to change of their own desires, social trends of the ideal nasal shapes, and various causes of dissatisfaction.
However, difficulty in revision surgery is another disadvantage of rib cartilages. Harvesting another rib cartilage for a revision surgery will be hardly acceptable for the patient, will pose a daunting task to the surgeon, will potentially jeopardize the patient-doctor relationship.
In this regard, augmentation rhinoplasty with alloplastic implants will remain popular for a long period of time especially in Asian countries, even though augmentation with autologous materials will gain more popularity.
Silicone versus ePTFE (expanded polytetrafluoroethylene)
There are many alloplastic materials that have been used for augmentation rhinoplasty.
However, this article will briefly review on the two most widely used alloplasts, which are silicones and ePTFEs, for the sake of conciseness.
When they are used in experienced hands with adequate sanitization measures, the infection rates for both alloplasts will be similarly low. And the chance of other complications and the aesthetic outcome also will be similar.5) In author’s experience of recent cases, the infection rate for the silicone implant is less than 0.1 % over 1000 cases of various follow-up periods from 1 month to 7 years.
ePTFE is preferred by a group of surgeons because of its softer appearance on the dorsum, stable settlement in the surgical pocket without significant mobility, easier carving, and minimal capsule formation.
ePTFE has unique characteristics as a porous implant. Through the pores, limited tissue ingrowth is permitted, therefore fibrous capsule formation around the implant is minimal. Limited tissue ingrowth immobilizes the implant, while removal of implant is still facilitated without extensive soft tissue dissection when it is needed.
No risk of long-term progressive capsular contracture is an apparent benefit of ePTFE over Silicone, even though an infected ePTFE may be accompanied with soft tissue contracture subsequent to inflammatory changes of the skin envelope.
An expanded polytetrafluoroethylene (ePTFE) has over a billion pores per square centimetre , their size (≈ smallest up to 0.2 μm in diameter) being orders of magnitude smaller than the smallest water droplet (±100 μm) and several times larger than a water vapour molecule (40 × 10−6 μm), and able to withstand a water pressure of up to 100 psi. The PTFE membrane is chemically inert, smooth, UV resistant, water repellent, and durable and can withstand high temperatures.
The ePTFE polymer has pore sizes ranging of 10 to 30 μm, averaging 22 μm in diameter. However, the pore size iis larger than the average size of most bacteria which is between 0.2 and 2.0 μm (diameter). But it is still smaller than the size of red (7 μm) and white blood cells (12-17 μm).
Implants with pore sizes greater than 1 μm are capable of harboring bacteria. Macrophages necessary for host antimicrobial activity need pore sizes greater than 50 μm to infiltrate materials. The ideal infection-proof implant would have no pores (i.e., silicone) to prevent bacterial invasion or pores greater than 50 μm to allow tissue ingrowth and cellular antimicrobial activity.5)
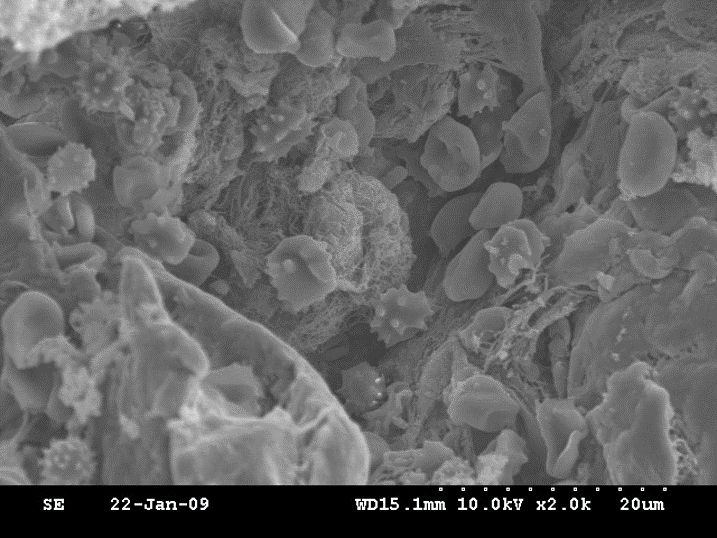
So, there is a chance of bacterial penetration into the implant matrix which cannot be eradicated easily.
A type of ePTFE in the recent market for rhinoplasty is claimed that it has the optimal pore size for tissue integration which is 30 μm (Surgiform®, Surgiform Technology, Ltd, 1566 Whiting Way, Lugoff, SC 290780) and its inter-nodal distance is 20-40 μm by the technical report of the company.
It is claimed that its pores stabilize the implant, minimizing migration and erosion with predictable tissue response and minimal scar capsule formation.
Despite numerous pores, its surface is hydrophobic in nature because of small pore sizes and fluoride ion. Therefore, the antibiotic or antiseptic irrigation cannot eradicate the bacteria inside the implant. And it is known that the porous surface is more susceptible to bacterial biofilm formation than the smooth surface. Therefore, the chronic indolent or chronic recurrent nature of infection is possibly more frequent for the ePTFE implant. The chronic recurrent nature of infection of ePTFE has been well known in hernia repair surgery or vascular graft using ePTFE.6), 7)
For silicone implants, when mild infection is suspected at the initial stage of infection, salvage treatment with vigorous irrigation and i.v. antibiotic treatment on daily basis could be tried, even though possible treatment failure must be discussed with patients.
However, for ePTFE, salvage treatment must be abandoned, because of ineffectiveness of irrigation and antibiotic treatments.
ePTFE is very stable in shape although it is stretchable and compressible to some degrees. But its stretchability, malleability or compressibility are obvious disadvantages for long-term outcomes of rhinoplasty.
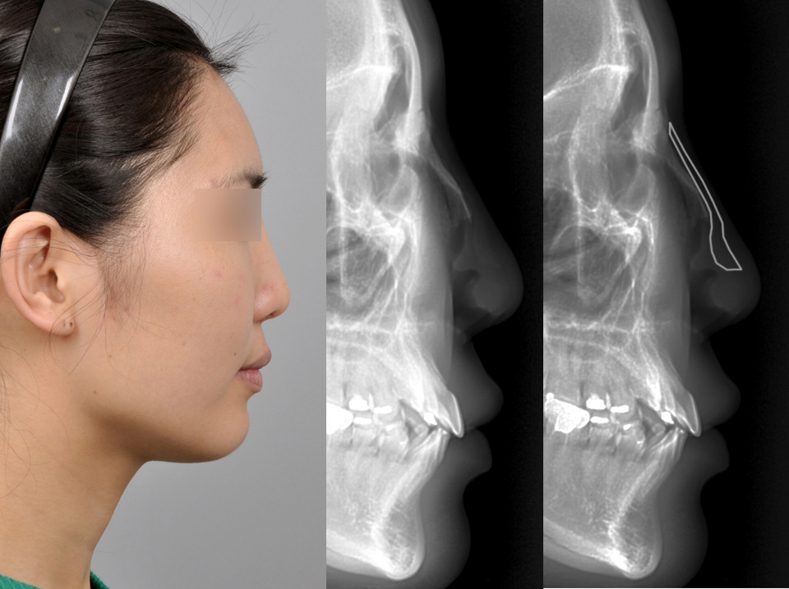
The anatomic nasal dorsum has natural convexity, where rhinion is the most projected area, nasion and anterior septal angle (ASA) are least projected areas. Especially in Asians, septal cartilages are relatively small, and therefore ASA is posteriorly located and weakly projected.
ePTFE tends to bend along this natural convexity of the dorsum with time. And its distal end is compressed down on ASA by overlying soft tissue. It is also true to the soft silicone implants.
This bending distortion will result in supratip depression to some degrees and distal margins of the implant will become noticeable by the gap between the implant and the alar cartilages.
Some surgeons make the distal part of ePTFE thicker to prevent this deformation, but it is not completely resolved even with careful design and carving of the implant.
Frequently the initial tip projection by septal extension graft or onlay grafts is gradually lost to some degrees during follow-up period from various factors such as weakening of caudal septum or graft and resorption of cartilages.
When the tip projection is lost significantly, the distal end of the implant becomes more conspicuous on the supratip area which may not be noticed during the immediate or mid-term follow-up period. The protruding or bulging distal implant with under-projected tip will give a very unnatural awkward appearance.


ePTFE is thought to give a smoother blended appearance on the dorsum right after surgery, comparing with the solid silicone implants which gives more defined appearance.
However, ePTFE may become even more conspicuous during long-term follow-up, because of progressive tissue ingrowth and tissue adhesions.
Tissue ingrowth can be a huge hindrance during revision surgery. Frequently, the adherent ePTFE implant is difficult to remove, especially when the implant is thin and implanted for a long period of time.
Some of surrounding tissue should be removed together with the implant inevitably and if subsequent skin irregularity arises, it is extremely difficult to restore.
This is in contrast with the silicone implant which is easy to remove when it is needed because of its presence in non-adherent fibrous capsular pocket.
Creation of smooth dorsal profile with a silicone implant
Silicone is the most widely used alloplastic implant material for rhinoplasty in Asian countries.
The advantages of silicone are many such as ease of use, inexpensiveness and there are various forms of silicone implants.
L-shaped silicones have been widely used in Asian countries, even though it has many drawbacks and possible serious tip skin problems.
It is easy to create a smooth unbroken augmented dorsal profile from the dorsum to the tip with L-silicones, and tip projection is conveniently provided with the vertical columellar part of the L-silicone.
Considering the extreme difficulty in achieving sufficient tip projection and definition with autologous materials in Asian patients with thick skin envelope and thin cartilages, its wide use in Asian countries will be understood.
Surgeons with good amount of experience dealing with L-silicones may produce aesthetically pleasing results with favorable complication rates. However, L-silicones are inherently prone to tip skin problems.
To prevent tip skin problems with the L-silicones, autologous cartilages are used in combination and a piece of autologous cartilage is sutured to the tip (onlay-like) or the front side (shield-like) of the implant. However the piece of cartilage sutured to the implant tends to become noticeable and unsightly during follow-up.
Instead of applying autologous cartilages on the tip of the implant, some surgeons dissect the undersurface of alar cartilages and the implant is placed underneath the covering of domal segment of alar cartilages.
With L-silicones, nasal tip is projected and also rotated, however it is difficult to elongate the tip with L-silicones without compromising tip skin, and therefore over-rotation is common for L-silicones.
Overzealous tip projection expecting the tent-pole effect with over-sized L-silicones will inevitably compromise the tip skin, resulting in skin thinning, chronic skin irritation or inflammation, and even extrusion of the implant.
Also, L-silicones are aesthetically unpleasing in many occasions.
The tip of the implant will generate a narrow uni-dome appearance, which is disharmonious with the wide alae of Asians. Tip will be augmented sharply on the midline only, and it will induce a pinched appearance with collapsed alar lobules.
Its vertical segment will elongate the infratip lobule, and it will make the nose look unnatural and unattractive along with the over-rotated tip
Rotated tip appearance by L-silicone will be beneficial in some patients with under-rotated and under-projected noses. However for short or small noses, over-rotation will be aesthetically detrimental.
The bird-shaped implant, a type of L-silicone which has a short vertical segment is claimed that it causes less skin problems with less skin tension on the tip. However, inherent problems such as uni-dome appearance, over-rotation are not different and clinically even there is no difference for the risk of tip skin problems such skin thinning, extrusion.8)

So called, I-shaped or straight shape silicone implants are used instead by other surgeons. However, some surgeons place I-shaped silicones on top of the alar cartilages expecting tip projection by the mass of silicone, with or without combined use of autologous cartilages.
However, placing the implant on the tip, the columellar-lobular ratio will be inevitably deteriorated by increased height of infratip lobule on top of the short collapsed columella. This unnatural columelar-lobular ratio gives a sense of operated look and a blunt or dull appearance of the nose. Over-rotated appearance, and tip skin problems are also same as in use of L-silicones.
Surgeons are easily tempted to use L-silicones or long I-shaped silicones because they want to make a smooth unbroken dorsal profile, and a proportional dorsal and tip augmentation simultaneously with silicones. And extreme difficulty of tip-plasty in Asians is another reason for the use of silicones on the nasal tip.
However, nasal tip is a soft and mobile structure by nature. Therefore, alloplastic material on the nasal tip will damage the tip skin easily by continuous tip motions.
Therefore, non-autologous materials must not be used on the nasal tip and they must be used only on relatively immobile nasal dorsum. Only when they are used on the dorsum, the risk of complication is low enough. And the procedures for the dorsum and tip should be separated.
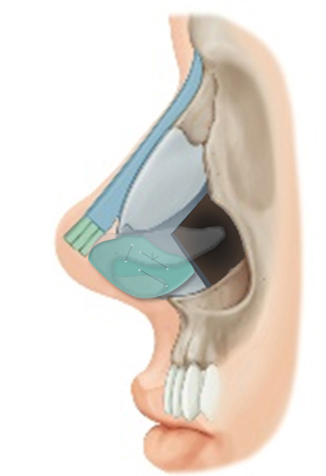
However when separate procedures for the dorsum with alloplastic implant and for the tip with autologous cartilages are performed, one of the most difficult task of augmentation rhinoplasty will be to make a smooth unbroken dorsal profile.
One solution is placement of the silicone implant right behind the onlay tip grafts by autologous cartilages or direct suturing of the distal implant to the back surface of the onlay tip grafts.
However, the direct suturing method will be more reliable rather than the end-to-end placement of the implant, because of difficulty in deciding an accurate length of the implant, and probable gap from tip motions and long-term loss of tip projection.
Using this method, to make a gentle upward curvature, in which the tip is gently more projected than the dorsum as desired by most of women, fine beveling of both the implant and tip grafts will be done. And combined use of other tip techniques such as the septal extension graft or columellar struts are recommended for a strong and stable long-term tip support.
To make a smooth unbroken dorsal line, different thickness of soft tissue in supratip and tip areas must be considered. And also when a soft silicone is used, gentle downward bending of the implant especially in the supratip area must be considered.
In this technique using onlay grafts, proper alar rim supporting measures such as the wing grafts to prevent collapse of alar sidewalls, alar rim retraction, pinching deformity and visibility of the onaly tip grafts, will be essential.9)
By the nature of the complexity of the technique, it takes a good period of time for a surgeon to be fully accustomed to the technique.

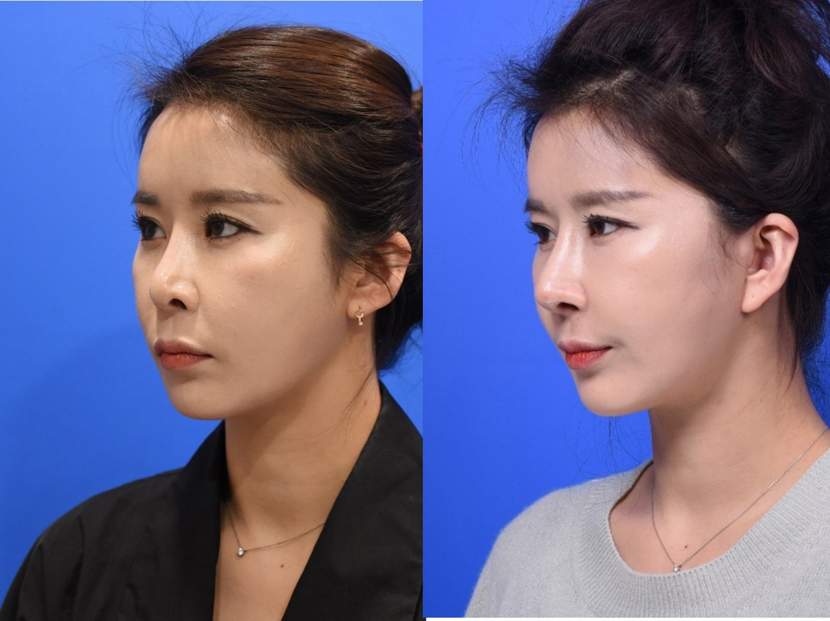


<Figure 7-1~4. Representative case who had revision rhinoplasty and facelift. The previous long I-shaped silicone implant was replaced with a new soft silicone and tip augmentation was done using septal extension graft, onlay grafts and wing grafts >
In another technique, the implant is placed right behind the cephalic margins of alar cartilages. However distal margins of the implant can become noticeable during the long-term follow-up with resolution of edema, soft tissue shrinkage, and loss of tip projection. Therefore, using this technique, the distal implant may be better to be tapered to become paper-thin distally beyond the cephalic margins of alar cartilages.
Safe use of silicone implants
Silicone may not be the ideal material for augmentation rhinoplasty as there is no such thing as the ideal material for augmentation rhinoplasty until now. However it is still one of the most practical and reliable material for augmentation rhinoplasty.
There are two most important requisites for the safe use of silicone implants.
One is the complete sanitization of the implant and the operation field, the other is the proper size of the implant.
As an alloplastic material, silicone is prone to bacterial infection. The surgeon must be vigilant against contamination of the implant throughout the surgery.
Complete sanitization of the surgical field is crucial, including occlusive taping of the hairlines, shaving of the vibrissae, scrubbing of the vestibule and anterior nasal cavity, packing of posterior nasal cavity with antiseptic soaked gauzes, and appropriate covering of the oral cavity.
The surgeon must minimize manipulation of the implant. And the implant must be soaked in an antiseptic solution throughout the surgery before and after any manipulation.
Frequent scrubbing of surgical gloves and operation field during the surgery is important, especially right before manipulation of the implant. Irrigation with antiseptic solution of the surgical pocket before insertion of the implant is also recommended.
If there is any chance of tear of mucosal barrier, judicious use of implant is warned. Although osteotomies are not a contraindication for the use of implant, when osteotomies are executed, they must be as clean and non-traumatic as possible. Medial osteotomies can be done without significant underlying mucosal damage when they are done with a small 4 mm osteotome while only the part of its tip is engaged superficially under direct visual control. For lateral osteotomies, percutaneous osteotomies are advantageous because generally they cause less trauma and minimal mucosal tear.
The other important prerequisite is the proper size of the implant.
Non-experienced surgeons in dealing with alloplastic implants tend to make an implant over-sized and excessively long.
A well-fitted implant must be placed snugly in the surgical pocket without tension. Tension may create deviation or extrusion of the implant.
An over-sized implant is at risks of dorsal and tip skin problems and movability also.
Surgeon should keep in mind that the anatomical length of bony-cartilaginous nasal dorsum is shorter than the surface length of nasal dorsum measured from the skin. Therefore, the proper length of the implant should be measured when the implant is placed inside the surgical pocket, not on the skin surface.
The exact length of the implant inside the pocket is measured carefully from the radix to the onlay tip graft or cephalic margins of the alar cartilages according to the surgeon’s technique, and it is marked on the implant and the extra-length of the implant is severed.
There are some other precautions for using alloplastic implants.
The nasal starting point in radix is usually located between the pupil and supratarsal crease or double-fold line in Asians. So proximally the implant should not be placed high above the supratarsal crease in most of cases. A highly placed implant often creates an unnatural operated look with an obliterated nasofrontal angle. It is especially true for Asians because Asians, especially females, have a smooth gentle curvaceous profile of radix area rather than an angle as in Caucasians. And the proximal margins of the implant must be tapered carefully to avoid later visibility.
Every patient has a degree of facial asymmetry. Therefore for the augmentation, midline should be assigned first in a sitting position before the start of the operation, which looks most straight to the surgeon’s eyes. It may be different form the line connecting the nasion and the nasal tip or midline of nasal bones.
On this midline marked on the skin, the subperiosteal pocket on the nasal bones is elevated symmetrically. And the pocket should be a little bit wider than the implant width, about by 10%. If the subperiosteal pocket is too wide or too narrow, it will cause deviation of the implant.
Cephalic dissection of the pocket should be limited just above the nasion. If cephalic dissection is more extended, unnecessary bleeding will arise which can cause hematoma postoperatively and cephalic migration of the implant will happen.
For an optimal outcome, individualized carving of implants are recommended. There are various types and shapes of ready-made implants in the market, however these implants cannot completely match with widely variable nasal shapes and soft tissue profile of patients.
Plaster models, computer imaging or 3D-printing technology may be used to design and prepare an implant preoperatively. However it is more desirable to carve, or at least modify, the implant intraoperatively, because the nasal profile will be determined not only by the static components which can be determined preoperatively such as bony or cartilaginous profiles but also by dynamic components which will change intraoperatively such as the strength of the tip support, skin tension, and soft-tissue redistribution.
Even though how accurately carved an implant is, it is practically impossible for an implant to be perfectly fitted in the anatomic dorsum. Minor dead spaces especially in the radix and supratip area will be unavoidable. However, minor dead spaces are usually filled with fibrotic tissue quickly in the early postoperative period causing no problems, however a significant dead space from a mal-designed implant will have significant negative effects causing fluid accumulation and subsequent infection and movability.
Soft silicone implants has an advantage to decrease the dead space, because soft silicone is easier to carve with usual surgical blades meticulously during the operation, and more pliant on the convex nasal dorsum. Theoretically it will cause less problems related to mechanical friction of the implant with skin envelope also. Mechanical friction is thought to be a cause or aggravating factor of unusually thick silicone capsule, skin irritation or inflammation, and skin thinning.
However because of its pliability, it is more difficult to make a smooth dorsal profile using soft silicones comparing with using a solid silicone implant,
Silicone-Soft tissue Hybrid
Even though Asians generally have thicker skin than Caucasians, Asians have a wide range of skin thickness, and some have very thin skin envelope.
And especially in revision cases, skin thinning and irregularity are common problems from repeated procedures and consequent soft tissue damages.
In thin-skinned patients, implant margins will be more noticeable and skin irritation by the implant is more common.
For these patients, implant should be as thin as possible, and implant margins must be tapered very carefully. And also soft tissue augmentation should be considered to soften the skin irregularity and implant contour.
Temporalis fascia, dermis or dermofat grafts are generally used for soft tissue augmentation in rhinoplasty, and these soft tissues can be directly sutured to the implant to cover the surface and margins of the implant.
With soft tissue is sutured to the implant, more augmentation volume can be obtained, and if the soft tissue has enough length, it can be extended caudally to cover the onlay tip grafts also.
It is also helpful in patients with combination of bossing frontal bones and low radix, because in these patients, the proximal margins of the implant is frequently noticeable even with careful tapering of the margins because of the considerable height difference between the forehead and radix, and significant thickness of the proximal implant to augment the low radix. Soft tissue covering of the proximal end of the implant will soften the contour in the radix area and decrease the implant visibility.
Contraindications
Because of inherent vulnerability to infection, alloplastic implants are judiciously used when there is a significant risk of infection.
In multiply revised noses, mucosal integrity is severely damaged and it is extremely difficult to completely restore the mucosal lining even with careful grafting and suturing. In this situation, alloplastic implant will be contraindicated.
And also when there is ongoing, or concealed infection is suspected, use of alloplastic implant is contra-indicated. In the revision surgery for an infected implant without convincing evidence of complete eradication of infection after an enough observation period, alloplastic implant is contraindicated. When unusual discharge or granulation in the surgical field is found during the surgery, alloplastic implant is also contraindicated.
Complications
Some complications related to silicone implants are serious, requiring immediate and decisive management, and some complications are less serious and can be treated with less aggressive maneuvers.
Serious complications are infection, implant extrusion, and severe capsular contracture. Less serious complications are deviation, visibility, calcification, and others. Serious complications are very rare in experienced hands, and related to technical errors by the surgeon rather than the inherent traits of silicone material, as discussed later. Fortunately, serious complications are avoidable and can be reduced.10-13)
Infection
Infection is the most dreaded and troublesome complication, which must be avoided with meticulous preventive measures. Alloplastic implants are susceptible to infection and, when infected, exhibit typical symptoms, such as erythema, swelling, and purulent discharge.
Delayed infection is also possible, and it is often subtle and less obvious, presenting as late recurrent swelling or mild erythema. There is evidence that chronic indolent but relapsing infection is related to bacterial biofilm on the surface of the implant.
Bacterial biofilm causes infection and inflammation of indolent nature in which traditional culture fails to recover any isolates.
Extrusion
Reported extrusion rates of silicone implants vary from 0.48% to 50%, probably due to the differences in surgical technique, implant shape, and the surgeon’s level of experience.
Roughly, there are 2 sources of the problem.
One is a poorly designed implant with excessive length, and the other source is infection. An excessively long implant may extrude through the tip skin or into the nasal cavity. A poorly designed implant, which is not stabilized in the nasofrontal angle or in the subperiosteal pocket, may migrate distally. Excessive pressure exerted by the L-silicone on the tip is associated with higher risk of extrusion.
Extrusion is often caused by infection also. An implant may extrude through inflamed and macerated soft tissue with a variable degree of purulence Sometimes, infection is less obvious with only minimal granulation tissue surrounding the implant. In such cases, the surgeon should be aware of the possibility of infection.
Capsular Contracture
Capsule formation is a natural host reaction to silicone implants. Fibrous capsule protects the skin and surrounding tissue isolating the implant. However capsular contracture is serious in some cases. Infection is the most well-known cause of serious capsular contracture. Severe capsular contracture often occurs after apparent infection or after removal of an infected implant. There are multiple clinical studies that have demonstrated significant correlation between presence of biofilms/bacterial colonization and capsular contracture of breast implants.An abnormally thick capsule will accompany varying degrees of contracture, which is related to various factors as well as infection, biofilm, such as nonimplantable or even nonmedical grade silicones, excessive soft tissue damage by overly aggressive techniques, and chronic inflammation or irritation by micromovement of the implant.
Capsular contracture is a frequent problem for silicone breast implants as well. Normally, severe capsular contracture of breast implants is reduced by antibiotic irrigation, antifibroblastic medications, and elimination of aggravating factors, such as soft tissue damage and intraoperative bleeding. These preventive measures and techniques may be applied to nasal implants.
Minor Complications
There are less serious complications, such as calcification, deviation, implant movability, and
Displacement and others.
Calcification is more common in silicone implants than in porous implants. It is more frequent for long-seated implants and may worsen with time. However, it is also influenced by technical factors, such as chronic mechanical stimulation of soft tissue by poorly designed movable implants and intraoperative damage to surrounding soft tissue. Use of a softer implant, decreasing implant movability, and decrease of soft tissue damage during operation may reduce calcification.
Deviation, movability, and displacement issues are avoided by proper implant design, adequate dorsal pocket formation, implant fixation, and nasal splinting after surgery. Careful implant placement in a properly created subperiosteal pocket as opposed to the subfascial or subcutaneous space reduces implant mobility and may decrease risk of displacement.
Conclusion
Alloplastic implants can be safely used in a medically acceptable range of complications. The range of complication rate vary significantly according to surgeon’s experience. For the safe use of alloplastic implants, thorough understanding of the nature of alloplastic materials, surgical proficiency and meticulous preventive measures against problems will be necessary. Alloplastic implants are preferably used only for dorsum and it is recommended to use autologous materials only for the mobile tip.
References
- Peled ZM, Warren AG, Johnston P, et al. The use of alloplastic materials in rhinoplasty surgery: a meta-analysis. Plast Reconstr Surg 2008;121(3):85e–92e.
- Yoo SH, Jang YJ. Rib cartilage in Asian rhinoplasty: new trends. Curr Opin Otolaryngol Head Neck Surg. 2019;27(4):261-266.
- Varadharajan K, Sethukumar P, Anwar M, Patel K. Complications associated with the use of autologous costal cartilage in rhinoplasty: A systematic review. Aesthet Surg J. 2015;35(6):644-52.
- Tasman AJ. Dorsal augmentation-diced cartilage techniques: The diced cartilage glue graft. Facial Plast Surg. 2017;33(2):179-188.
- Ham J, Miller PJ. Expanded polytetrafluoroethylene implants in rhinoplasty: literature review, operative techniques, and outcome. Facial Plast Surg. 2003;19(4):331-9.
- Perez-Ko¨hler B, Bayon Y, Bellon JM. Mesh infection and hernia repair: a review. Surg Infect (Larchmt) 2016;20(10):1–14.
- Walker TJ, Toriumi DM. Analysis of facial implants for bacterial biofilm formation using scanning electron microscopy. JAMA Facial Plast Surg 2016;18(4):299–304.
- Lam SM, Kim YK. Augmentation rhinoplasty of the Asian nose with the “bird” silicone implant. Ann Plast Surg 2003;51:249–56.
- Kim IS. Augmentation Rhinoplasty Using Silicone Implants. Facial Plast Surg Clin North Am. 2018 Aug;26(3):285-293.
- Genther DJ, Papel ID. Surgical nasal implants: indications and risks. Facial Plast Surg 2016;32:488–99.
- Ferril GR, Wudel JM, Winkler AA. Management of complications from alloplastic implants in rhinoplasty. Facial Plast Surg 2013;4(21):372–8.
- Erlich MA, Parhiscar A. Nasal dorsal augmentation with silicone implants. Facial Plast Surg 2003;19: 325–30.
- Peled ZM, Warren AG, Johnston P, et al. The use of alloplastic materials in rhinoplasty surgery: a meta-analysis. Plast Reconstr Surg 2008;121(3):85e–92e.
