Introduction
Rhinoplasty in African-Americans has become an increasingly common and accepted procedure, and facial plastic surgeons must be skilled in creating a harmonious “ethnic” nose. In a recent study by the American Academy of Facial Plastic and Reconstructive Surgery, when given multiple options for facial plastic surgery, African Americans most commonly choose a rhinoplasty (1). African American rhinoplasty presents a unique set of anatomical challenges and cultural differences. This chapter reviews the anatomy, pre-operative nasal evaluation, counseling, surgical planning and techniques, post-operative care and complications of an African American rhinoplasty.
Anatomy
In planning an African American rhinoplasty, one must understand the unique nasal anatomy. The characteristics of the African American or the platyrrhine (literally meaning broad and flat) noses (Figure 1 A & B) when compared to the Caucasian, leptorrrhine (literally meaning tall and thin) nose include:
- The skin-soft tissue envelope is thick with abundant fibrofatty tissue.
- The skin is inelastic and has abundant sebaceous glands.
- The radix is deep and inferiorly-set.
- The nasal bridge and dorsum feature short, wide and flat nasal bones.
- The nasal tip is bulbous, poorly projected, counter-rotated, abundant fibrous nasal SMAS, broad domes and poorly defined.
- The columella is short and retracted.
- The septum is short.
- Lower lateral crura are horizontally-orientated.
- The nasal spine is under-developed.
- The alae are wide, thick, horizontal and flared.
- Nasolabial junction is retracted and has an acute angle (< 90 degrees).
- Maxilla is retruded and/or hypoplastic.
- The bony base is wide.
- The base view is less triangular in shape.
- The soft tissue triangle is obtuse.
- Nostrils are oval with the central axis vertically-oriented.
Historically, it was thought that the lower lateral cartilages in African Americans were thin and weak. Recent studies have shown that the lower lateral cartilages are similar in size and strength to a Caucasian nose (2).
Preoperative Nasal Evaluation and Surgical Planning
A history is performed with an emphasis on the patient’s aesthetics concerns and nasal airway. If patient presents for a revision rhinoplasty, details of the previous operations and operative reports are reviewed.
On physical exam, a visual and tactile evaluation of the nose are performed from the frontal, oblique, lateral and base views. Bilateral paramedian vertical light reflexes along the dorsum are analyzed for symmetry. The middle vault is examined for narrowing and symmetry while the nasal bones are analyzed for their length, height, width and symmetry. An ungloved finger is used to palpate the nose, examining the bony and cartilaginous skeleton tip and the skin-soft tissue envelope. The nose is analyzed from the lateral view for the nasal starting point, shape of the dorsum, nasal length, nasal projection, nasofrontal angle, nasolabial angle, alar retraction, columellar show, depressor nasi function and chin projection. The nasal base is visualized from the frontal and basal views analyzing the width and shape. The ala is inspected for flaring and its width compared to the medial canthus. The width of the alar base should approximate the intercanthal distance and the extension beyond this point is noted. The alar canthal relationship is examined for a gentile transition. The caudal septum in viewed for deflection and ratio of the nostril/tip composition is documented. The nostrils ideally compose 2/3 of the base view.
The patient with nasal obstruction, its location and alleviating and exacerbating factors are documented. Anterior rhinoscopy may visualize additionally etiologies of nasal obstruction including the nasal septum, which is characteristically short. Due to its small size, the cartilaginous septum may be insufficient for reconstructive nasal grafting.
The nasal anatomy is documented on the nasal analysis sheet and the surgical plan is outlined.
Figure 1
NASAL ANALYSIS
Patient Name:__________________________________________________
Date: __________________
- Skin Quality: Thin Medium Thick Sebaceous Telangiectasias
- Primary Description: Big Twisted Large Hump Boxy Pinched Bulbous
Frontal View
- Dorsum: Twisted Deviated Straight Convex: R L Bony Bony-Cartilaginous Cartilaginous
- Width: Narrow Wide Normal Wide-Narrow-Wide Depressed L R
- Tip: Normal Deviated Bulbous Asymmetric Amorphous Pinched Parenthesis Deformity
- Support: Normal Weak
- Medial Canthal-Alar Relationship: Wide Normal Narrow Sill Weir
- Tip Defining Points: Uni Double Narrow
- Nasal Bones: Short Normal Long
- Middle Vault/Upper Lateral Cartilages: Narrow Normal Subluxed Asymmetric
Base View
· Trapezoidal Triangular
- Tip: Deviated Bulbous Wide Bifid Asymmetrical
- Base: Wide Narrow Normal Dislocated Caudal Septum: No Yes R L
- Rim Aperture: Narrow R L Normal
- Columella: Columellar/ Lobule Ratio (2:1) Normal Abnormal
- Medial Crural Footplates: Wide Normal
Lateral View
- Nasofrontal Angle: Shallow Deep Normal
- Nasal Starting Point: High Low Normal
- Nasal Length: Normal Short Long
- Dorsal Hump: Y N Bony Cartilaginous Over-Resected Bone Cartilage
- Tip Projection: Normal Decreased Increased Ratio (.55-.60)__________ (TDP-AFJ/Nasion-TDP)
- Alar-Columellar Relationship: Normal Abnormal A-C Show ________mm
- Naso-Labial Angle: Obtuse Acute Normal ___________ degrees
- Infratip Lobule: Over-rotated Counter-rotated Normal
- Supratip Break: Y N
- Nasal Ptosis Y N With Smiling: Y N
- Infratip Break: Y N
- Chin: Normal Microgenia Macrogenia
- Columella: Normal Hanging (Septum Medial Crura Soft Tissue) Retracted (Base)
- Ala: Normal Hanging Retracted R L
- Pollybeak: Y N Cartilaginous Soft Tissue
Intranasal
· Septum: Deviated Y N Spur R L
Caudal Deviation Y N R L
__________% Obtsruction R
__________% Obstruction L
Edematous Mucosa Y N Erythematous Mucosa Y N
Perforation Y N If yes, where ____________________
· Turbinates: Hypertrophic Y N R L Normal
· Internal Nasal Valve: Narrow Normal
- External Nasal Valve: Collapsed Intact
- More Prominent Ear: R L
PROBLEM LIST/PLAN:
Alar Batten Grafts L R Alar Rim Grafts L R Lateral Crura Strut Grafts L R
Columellar Strut Infratip Lobule Graft Dome Graft Shield Graft Plumping Grafts
Composite Grafts L R Medial Crural Overlay Lateral Crural Overlay Dome Sutures
Tongue-In-Groove Spreader Grafts L R Septal Extension Graft Reposition LLC
Conchal Cartilage L R Costal Temporalis Fascia L R
Onlays: Lateral Nasal Wall L R Radix Bony Vault Middle Vault
Alar Base Reduction: Sills Weir I II1 Septoplasty Turbinoplasty
Osteotomies Double R L Hump Reduction Bone Cartilage
Functional: Cosmetic:
Figure 1 A comprehensive nasal analysis is undertaken from the frontal, lateral, basal, and intranasal viewpoints. After analysis, a preliminary surgical plan is outlined.
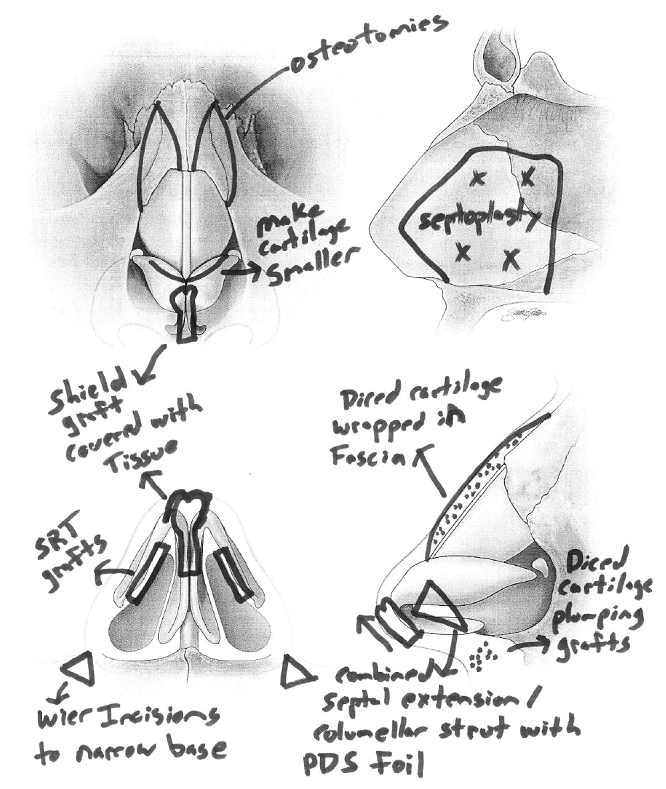
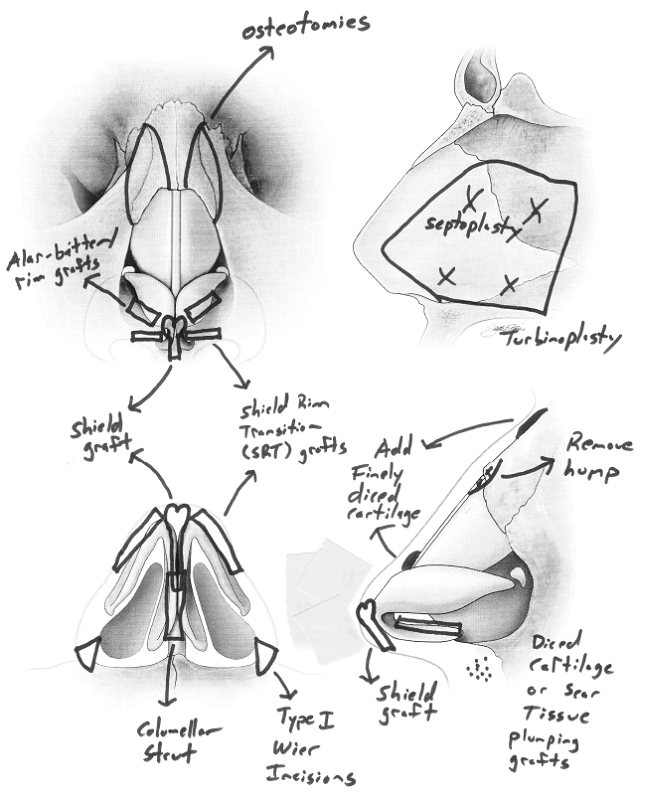
For example: 1. If structural grafting is necessary, a decision is made regarding the source (septal, conchal, costal cartilage and deep temporalis fascia). 2. Bulbous, poorly projected tip with a plan of open rhinoplasty 3. Cephalic trim and tip suturing to define nasal tip 4. Combined septal extension/columellar strut to counter rotate nose 5. Shield graft to project nose 6. Shield-Rim Transition grafts (SRT grafts) to create smooth contour from the shield graft to ala 6. Low dorsum with a plan of augmentation with diced cartilage and deep temporalis fascia 7. Close columellar incision 8. Infratip diced cartilage graft to create a smooth infratip break 9. Close remainder of incisions 10. Wide ala with a plan of bilateral alar base reduction. 11. Doyle splints, nasal taping and aquaplast splint. A thorough understanding of autologous cartilaginous sources and alloplastic reconstructive options are essential to creating an operative plan. Computer imaging and morphing software can be a useful method of communication, It facilitates an atmosphere where the surgeon and patient have an opportunity to communicate about possible aesthetic results.
It is important to communicate that imaging is not a guarantee of results. Imaging software is used to evaluate surrounding facial features including the chin. African Americans may have microgenia, in which a chin implant may be recommended. Prior to surgery, standardized rhinoplasty photographs are taken.
In general, the primary goals in African American rhinoplasty include:
- Bridge: Moderately thinner on frontal view.
- Dorsum: Augmented height on lateral view.
- Tip: Improved definition, increased projection and increased rotation.
- Base: Vertical-oblique nostrils and nasal base approximating an equilateral triangle.
- Columella: Increased columellar show and length.
- Nasolabial junction: Increase nasolabial angle.
- Maxilla: Augment on lateral view.
Communication of expectations, goals and informed consent in the pre-operative consultation is essential in creating an environment and plan for a successful procedure. This is best accomplished by reviewing the exam, nasal analysis sheet, previous operative reports, photos, problem list and surgical plan before proceeding with the surgical treatment. The surgical plan is outlined on a nasal diagram during the pre-operative examination. Each surgical step is explained to the patient and the sheet is signed by the patient indicating agreement to the surgical plan. (Figure 2)
Surgical Sequence and Techniques
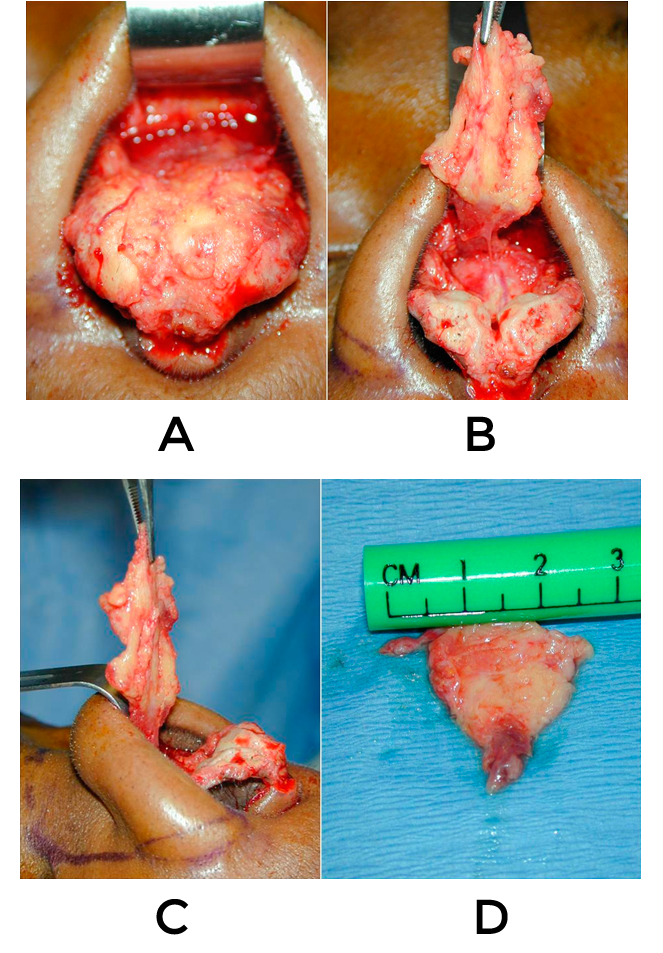
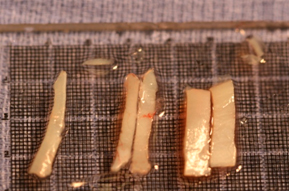
Cartilage Harvest
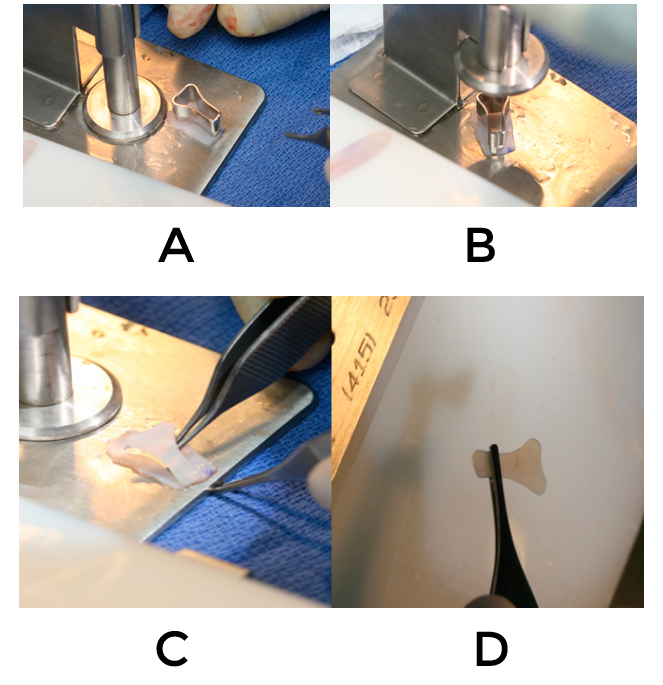
Cartilage grafts are carved and secured to the native cartilage framework to improve the airway and refine the nose. This cartilage may be harvested from the septum, ear or ribs. Many times, the septal cartilage is inadequate for nasal reconstruction; therefore, additional autologous cartilage is harvested (3). Auricular cartilage is harvested from the concha cavum and concha cymba. This is approached from either the anterior or posterior surface. If a surgical plan entails extensive cartilage grafting, we commonly recommend using costal cartilage. If the patient is adverse to costal cartilage harvest, bilateral conchal cartilage harvest with the use of polydioxanone plate, PDS plate TM (Mentor worldwide, LLC, Santa Barbara, Ca.) is an additional option. A PDS plate TM is a thin sheet of polydioxanone that is flexible enough to secure cartilage yet strong enough to straighten it. PDS plate TM is secured to the convex side of the conchal cartilageTM to straighten the cartilage.


External Rhinoplasty Injection
In the majority of African American rhinoplasties, the external approach is preferred. Local injection with 1% lidocaine with 1:100,000 epinephrine is injected throughout the surgical area. Injection used for hemostasis and in hydrodissecting the cartilage framework from the skin-soft tissue envelope and vestibular tissue. Once the soft tissue envelope has been elevated, dissection is carried in a subperiosteal plane over the nasal bones.
Wide dissection in this area is not recommended. The mucoperichondrium overlying the lower lateral crura is hydrodissected, and then sharply excised. This mucoperichondrium may be used as a graft or placed over a shield graft.
Septoplasty and Inferior Turbinoplasty
Septoplasty is performed for either a deviated septum or cartilage harvest. At least 10 mm of a caudal and dorsal strut is left for support. If hypertrophic turbinates are present, then a conservative turbinoplasty is performed. Turbinectomy is discouraged, as it carries the risk of empty nose syndrome and paradoxical sensation of nasal obstruction.
Nasal Tip Surgery
Frequently, African American noses will need narrowing and definition to the tip while increasing projection and rotation. Surgery of the African American tip is challenging as their thick skin will limit results. In order to increase projection and rotation, structural grafting is necessary.
Initially, cephalic trim of the lower lateral crura may be performed to help define the nasal tip. We preserve approximately 7 mm of the lower lateral cartilage to maintain nasal support. If the lower lateral cartilages are going to be further manipulated, the vestibular tissue is dissected from the medial and lateral lower cartilages. This release, which is facilitated by hydrodissection, will enable the natural curvature of the lower lateral crura. Many times, this maneuver will add tip projection as it releases the constraints of the soft tissue envelope on the lower lateral crura.
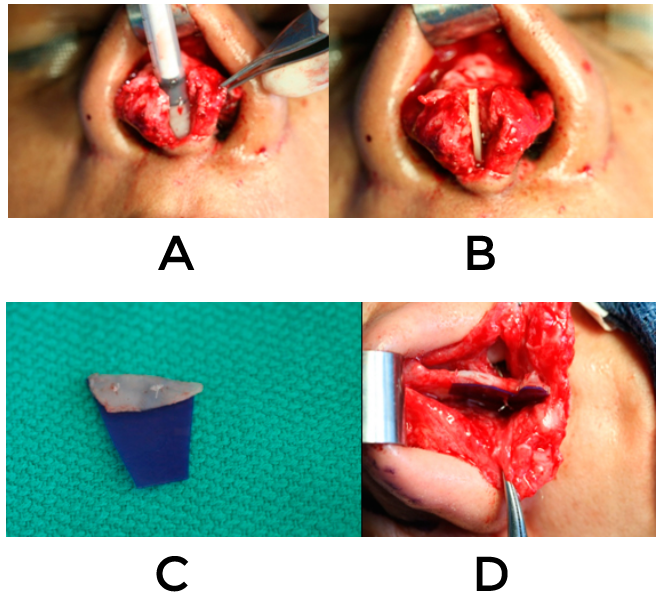
A pocket is made between the medial crura down to but not abutting the nasal spine. If the patient requires plumping grafts, approximately 0.3 cc of finely diced cartilage injected through a syringe is placed in a small pocket near the anterior nasal spine. The columellar strut, ideally carved from septal or costal cartilage, is secured to the medial crura using a 4-0 absorbable suture. If the nose requires lengthening or counter rotation, a combined septal extension/columellar strut is secured to the caudal septum and the medial crura. A PDS plate TM is used to secure this graft to the septum in an end-to-end fashion. The plate is only placed on one side to allow for imbibition on the contralateral side to ensure the graft’s survival.
A columellar strut may be created with auricular cartilage by suturing a double-layered segment with the concave sides facing one another. It can also be created by suturing the convex side of the auricular cartilage to PDS plate TM to straighten it.
Fine tuning of the tip is performed using a variety of tip grafts and suture techniques. Commonly, a lateral crura steal, advancement of the lateral crura onto the medial crura, increases the nasal tip projection and rotation (4). If patient does not require cartilage grafting, this maneuver may be used as the primary technique to increase projection and increase rotation. Interdomal and bilateral transdomal sutures are placed using 5-0 polydioxanone sutures (Ethicon, Somerville, NJ) to symmetrize, refine and support the tip.
Additional grafts may modify tip projection such as a shield tip graft, bruised onlay dome and/or infratip lobular grafts (Figure 7).
These grafts will add length to the infratip lobule and create proper tip defining points. Shield grafts made from auricular cartilage are usually less rigid than septal grafts. Shield grafts that are curved or weak may be secured to PDS plate TM to straighten and support the graft. If the graft extends a moderate amount above the native tip, a buttress graft is placed cephalad to the shield graft to prevent “bending”.
In thin to medium skinned patients’ harvested tip mucoperichondrium, rib perichondrium or deep temporalis fascia can be placed over the tip complex to camouflage the visibility of the graft edges.
After closing the columellar incision, shield rim transition grafts, SRT grafts, are placed if a shield graft is used. SRT grafts abut the shield graft and traverse the majority of the ala. They create a balanced alar-dome contour and camouflage the lateral edges of the shield graft. Failure to place these grafts will result in retraction of the ala, most pronounced at the soft tissue triangle.
The remaining incisions are closed and the infratip break is examined for a contour. The infratip lobule is frequently deficient and finely diced cartilage is added as an infratip lobule graft. If a shield graft has been placed, the finely diced cartilage is added similarly to fill and counter rotate the tip.
An infratip lobule graft is infrequently required if a combined septal extension/columellar strut has been placed, as this graft frequently creates a smooth infratip break.

Osteotomies
Many African American patients have low nasal bones; therefore, osteotomies are difficult to perform. If indicated, high-low-to-low lateral osteotomies with infracting or fading medial osteotomies are performed.
Radix and Dorsal Augmentation
It is our preferred method to augment the nasal dorsum with autologous grafts, including septal, conchal or costal cartilage over alloplastic grafts. To ensure proper graft placement, a precise pocket is created over the desired area of augmentation to prevent migration.
Surgical options for conservative radix and/or dorsal augmentation are nasal mucoperichondrium, rib perichondrium or deep temporalis fascia (Figure12).
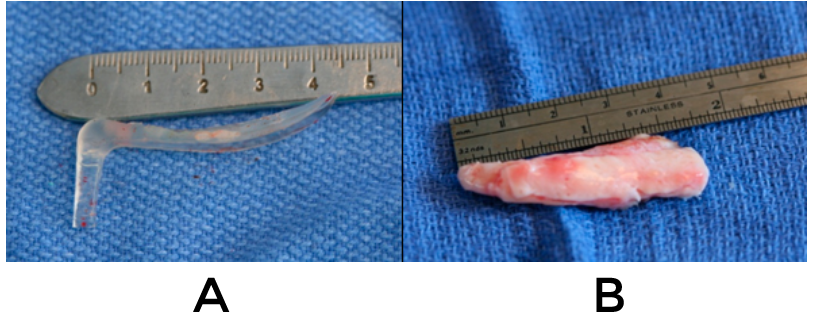

Finely diced cartilage is used for the majority of radix and/or dorsal augmentation. Finely diced cartilage is placed in a 1 cc Braun tuberculin syringe TM (Braun Mesungen AG, Melsungen Germany) and injected into the radix/dorsal pocket.
An interposing layer of deep temporalis fascia, harvested scar tissue, perichondrium or mucoperichondrium is placed between the overlying soft tissue and the finely diced cartilage to camouflage any irregularities. Usually, 1 to 3 cc of finely diced cartilage is injected along the dorsum to prevent migration of the diced cartilage to the lateral nasal wall. To soften the transition between the tip, supratip augmentation is performed with finely diced cartilage.
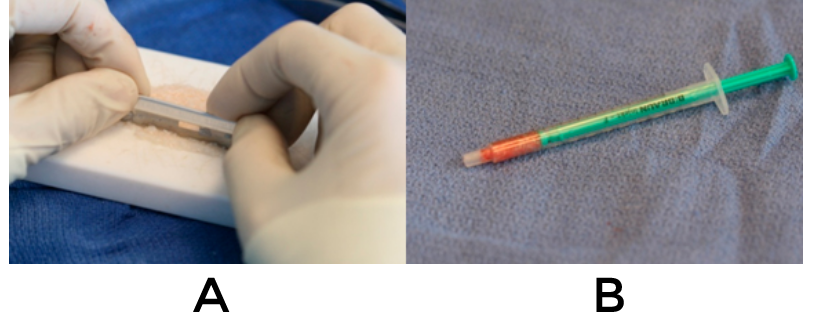
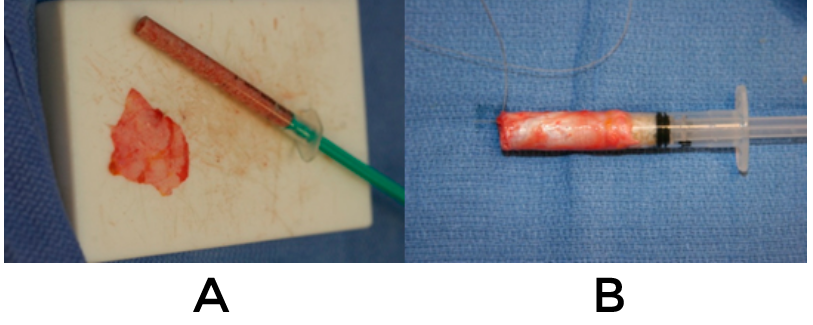
Diced cartilage wrapped in fascia (DCF) is another option for moderate dorsal augmentation (5). It is constructed by wrapping deep temporalis fascia around the diced cartilage filled tuberculin syringe and the fascia is close on itself using a running 5-0 chromic suture. To ensure smooth dorsal augmentation, the DCF graft should extend to the cephalad supratip region. This will tent the overlying soft tissue envelope and allows for a natural appearing dorsal augmentation. Historically, en bloc cartilage grafts placed over the dorsum have been used for dorsal augmentation. They have been associated with warping, unnatural appearance or may resorb. (6)
Alar Flare and Base Reduction

Alar base procedures in the African-American patient can be subdivided into alar base reduction and correction of alar flare. The surgical plan will depend on pre-operative evaluation of the alar base and nostril.
Alar base procedures in the African-American patient can be subdivided into techniques that narrow the alae with or without modifying the nostril sill and floor or a combination of these.
Sheen has described several ways to reduce the alar lobule and nostril, which if performed properly, will create an aesthetically pleasing result with a minimally visible scar (6). Two frequently encountered alar base configurations in the African American nose are described:
- Type I: Larger than ideal alar lobule with appropriately sized nostrils.
- Type II: Larger than ideal alar lobule with larger than ideal nostrils.
Type I configuration involves conservative cutaneous elliptical excision at the alar groove without excision of the vestibular skin. Dissection is carried down to the dilator nasalis muscle, and the overlying soft tissue is excised. Commonly, 3-5 mm of reduction will provide a significant degree of change. Conservative resection is encouraged in this technique to achieve a natural appearing nasal base.
In Type II configuration, cutaneous alar lobule elliptical incision is combined with a nostril sill and floor excision.
Traditional teaching places the alar incision approximately 1 mm on the nasal side of the alar-facial junction. We believe this may create a visible scar at the cephalad alar lobule due to the placement of the incision.
To best camouflage the scar, the incisions are made in the alar-facial junction to camouflage the scar. Bipolar cautery can be used sparingly for hemostasis followed by subcutaneous closure using 5-0 vicryl for the deep tissues, and a running 6-0 polypropylene or fastgut suture for the skin closure. The sutures are typically removed in 5-7 days.

Postoperative Nasal Care
At the conclusion of the rhinoplasty, a thin sheet of gelfoam, tape and nasal cast is placed. It is removed at post-operative day 7 as well as the sutures, and the nose is re-taped for 1 week. During this time period, patients are instructed regarding:
- Meticulous cleansing of incisions
- Nasal saline spray
- Nasal suction bulb as needed
- Head elevation
- Cold compresses
Patients that develop prolonged swelling, nighttime taping is continued for 6-10 weeks. For early post-operative edema and for eradication of scar tissue, subcutaneous injection of a combination of 0.4 cc of 5-fluorouracil and 0.04 cc of and Kenalog 5 mg/cc are administered. 5- Fluorouracil inhibits thymidylate synthase, interferes with RNA synthesis and has been used safely in the treatment of keloids and hypertrophic scars (10). We believe this injection has a powerful yet safe anti-inflammatory effect and is effective in treating early pollybeak deformities and nasal scar formation. We have yet to experience an adverse reaction to this injection. 5-Fluorouracil is injected in the supratip, infratip, tip and lateral tip with an average of 0.05 cc into each location. The injections can begin as early as 2 weeks following surgery and can be repeated every 3 weeks as needed.
Risks and Complications
- Over-aggressive cartilage removal causing an amorphous tip appearance.
- Prolonged bruising or hyperpigmentation.
- Infection.
- Prominent alar scarring.
- Excessive alar reduction.
- Abnormal appearing ala.
- Flat ala with loss of natural base curves.
- Nasal asymmetry.
- Graft irregularities, displacement, or extrusion.
- Graft absorption.
- Prolonged swelling.
Conclusion
In order to perform an African American rhinoplasty, one must master the unique nasal anatomy and qualities of an ethnic nose. In the pre-operative consultation, a detailed evaluation and surgical plan is created and discussed with the patient. Realistic goals are established for both the patient and the surgeon. In order to create an aesthetic pleasing and functional ethnic nose, adequate cartilage is made available for grafting from the septum, ear or rib. Secondary to African Americans frequently have a short septum, autologous cartilage options such as costal cartilage are frequently necessary. With the advent of PDS plate TM, bilateral auricular cartilage grafts may be used as an option to costal cartilage harvesting. With the advent of the PDS plateTM, bilateral auricular cartilage harvest may be an option in a patient that historically would of required reconstruction with costal cartilage.

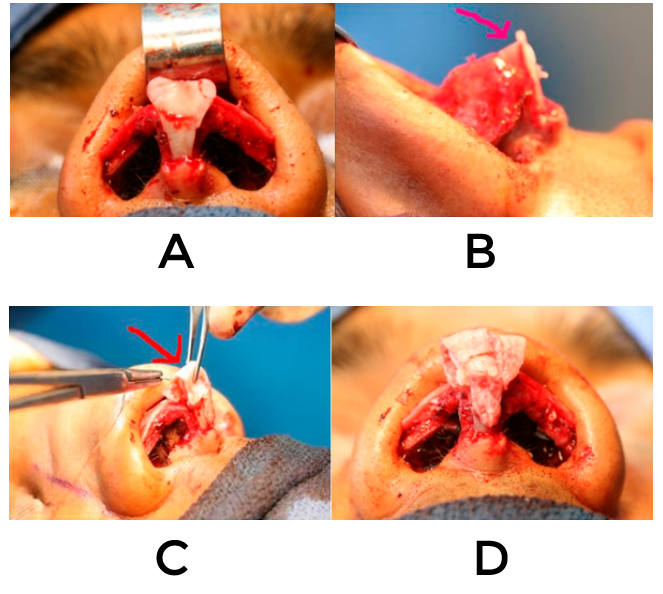
Note the improper placement of her previous columellar incision (red arrow)
Long term results with PDS plate TM are unknown but are promising. Moderate to significant dorsal and radix augmentation has been traditionally achieved with large en bloc cartilage grafts.
We believe that finely diced cartilage injected posterior to rib perichondrium or deep temporal fascia is a viable alternative. African American rhinoplasty remains a challenge secondary to their thick skin, small septum, and requirement for cartilage grafting to project and counterotate the nose.
Case Presentation
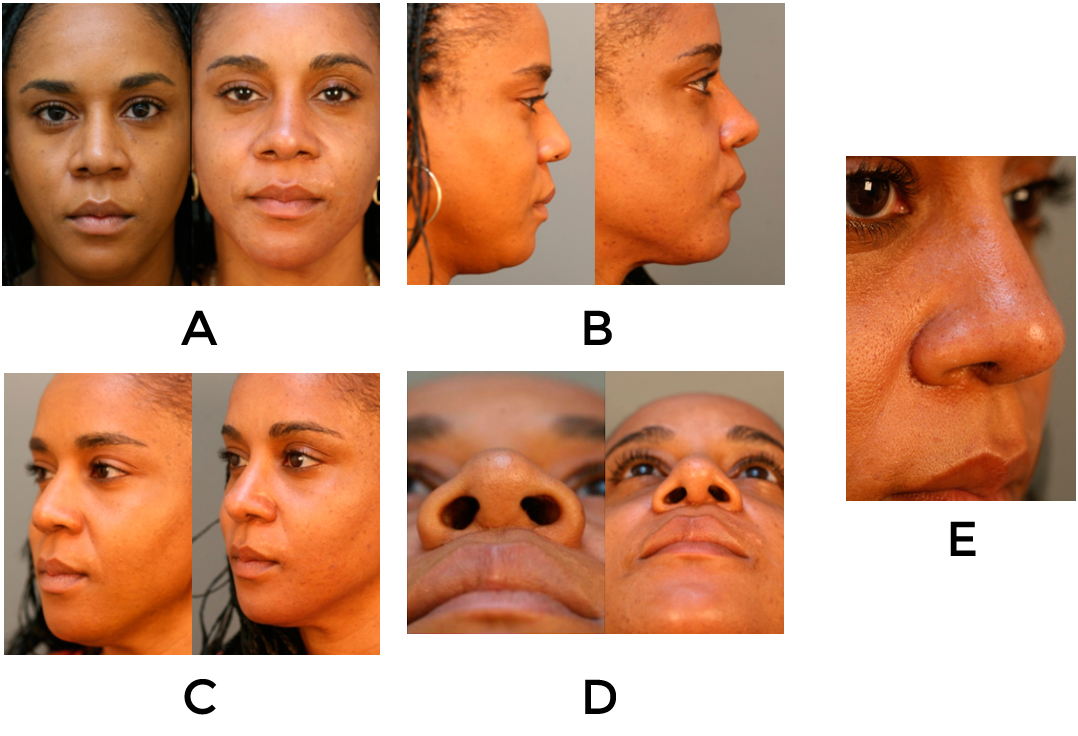
Patient is a 40 year old African American female who dislikes the width of her nose and nostrils. She has bilateral nasal obstruction and had an open rhinoplasty and alar base reduction 8 years previously.
Examination
The skin is thick and sebaceous, and the cartilaginous dorsum is deviated to the right. On frontal view, the tip is bulbous, deviated to the right with a unilateral tip defining point. The alar base and dorsum are wide and the right alar base is lower than the left. On palpation, the nose has poor support.
On base view there is alar flaring (right greater than left), oversized nostrils (approximately 50% of the base height), and there is an improperly placed columellar scar from her previous incision. In regards to her profile, her radix is deep, columella is retracted with poor columellar show, weak anterior nasal spine, underprojected tip, acute nasolabial angle, and a caudal bony/cartilaginous hump.
Operative Technique:
1% lidocaine with 1:100,000 epinephrine was infiltrated into the turbinates and septum. Pledgets soaked in 1:100,000 epinephrine and pontocaine were placed in the nasal cavity. The face and neck were prepped and draped in the usual sterile manor. A left hemi-transfixion incision was made and the mucoperichondrium was elevated on the left side of the incision and extended to beyond the junction of the bony and cartilaginous septum. The septum was disarticulated from the bony septum and the contralateral mucoperiosteal flap was then elevated off the bony septum. Takahashi forceps were then used to remove the deviated bony septum. For the spur, a 4 mm osteotome was used to remove it. The cartilaginous septum was excised leaving a 10 mm dorsal and caudal strut. The septum was then closed with running 5-0 chromic.
Additional cartilage was required. Bilateral conchal cartilage was harvested in identical fashion. 1% lidocaine with 1:100,000 epinephrine were infiltrated into the postauricular incision and ear. A 3 cm postauricular incision was made and a combination of blunt and sharp dissection was performed elevating in a submucoperichondrial flap along the cartilage. Next, the cartilage was excised laterally to the EAC with support intact for the external auditory canal.
The mucoperichondrium was left intact anteriorly. Support was left intact medially in the conchal region. Hemostasis was controlled with bipolar cautery. The wound was irrigated with antibiotic irrigation. Approximately 1cc of ¼% marcaine with 1:200,000 epinehprhine was sprayed into the wound. The wound was closed with a running locking 4-0 chromic. A bolster suture (3-0 nylon) was placed through the two flaps with cotton soaked in antibiotic ointment and contoured to fit the conchal bowl.
The incision was made at the columellar base at the previous scar. Using a 15 blade, bilateral marginal incisions connected to a transcolumellar incision were made and the soft tissue was then elevated off the lower lateral cartilages and nasal dorsum. Dissection was then subperiosteal over the nasal bones. Scar and mucoperichondrium was then harvested off of the lower lateral cartilages and saved. The bony dorsum was reduced by 2mm with number 3 and 4 rasps. The nose was irrigated. Using sharp dissection, the interdomal ligament were divided and the anterior septal angle was identified.
The upper lateral cartilages were divided off their attachment to the dorsal septum. 2mm of the cartilaginous dorsum was sharply excised while tapering it cephalically. Bilateral curved lateral high to low to high osteotomies were performed. Medial osteotomies were not performed because the nasal bones were fully mobile after lateral osteotomies.
Dissection between the medial crura was carried down to but not abutting the anterior nasal spine. The previously resected scar tissue was placed into this pocket as plumping grafts. A columellar strut carved from septal cartilage was secured to 0.25mm thick PDS plate TM to straighten the slightly curved cartilage. This was sandwiched in between the medial crura and secured with a 4-0 plain gut horizontal mattress sutures. To reconstruct the tip, bilateral double domal and intermediate domal sutures were placed using 5-0 polydioxanone horizontal mattress sutures. The upper lateral cartilages were reattached to the septum with horizontal mattress sutures using 5-0 clear polydioxanone initially to the left upper lateral cartilage then septum then to right upper lateral cartilage and back while burying the knot between the septum and the upper lateral cartilages.
A #2 shield graft was carved from septal cartilage and secured to 0.25mm thick PDS plate TM due to the thinness of the septal cartilage. The PDS plate TM was used to prevent the graft from bending. It was fixated to the lower lateral cartilages with 5-0 polydioxanone horizontal mattress sutures. A buttress graft was place cephalically to the shield graft to prevent “bending” and secured with 5-0 polydioxanone horizontal mattress.
The columellar incision was then closed with a 5-0 subcutaneous polydioxanone and the skin was closed with interrupted 6-0 prolene and 5-0 fast gut. 1.2 cc and 0.3 cc of finele diced cartilage were injected with a 1 cc syringe in the supratip region and radix, respectively. Bilateral combined alar batten/rim graft (5x 24mm) where carved from ear cartilage and secured to 0.25mm PDS plate TM. They were placed in the marginal incisions pockets to help strengthen the weak external nasal valve and to soften the transition from the shield graft. To symmetrize the soft tissue triangles, an additional 2 x 5mm shield rim transition grafts were placed abutting the shield graft. Interrupted 5-0 chromic was used to close the marginal incisions.
Bilateral Sheen type I alar resection (cutaneous) were marked (5mm on right and 3mm on left). An 11 blade was used to make the inferior incision extending medially along the alar base. The incision was made in the alar-facial junction. The tissue was excised down to the dilator naris muscle and hemostasis was obtained with bipolar cautery. They were closed with 5-0 vicryl subcutaneous sutures and 6-0 running prolene on the skin.
Photodocumentation was performed. External nasal tape and a splint were then applied on the nasal dorsum. Bilateral Doyle splints (Boston Medical Products, Westborough, Mass.) with the posterior lumen removed and saturated in antibiotic ointment were placed in each side of the nasal cavity and fixated to the vestibular septum using 4-0 nylon.
Post-operative evaluation
The patient underwent extensive cartilage grafting in order to create a softer natural appearing nose. These 4 month post operative photos reaveal an improved nose with resolving edema. The nose will take a total of two years to heal. From the frontal view, her base has been narrowed and the tip has been refined. The double tip defining points are approximately 4mm apart and symmetric. There is a natural curvature of the nose from the medial clubhead of the brow to the nasal base.
She has a strong straight profile with a gentle supra and infratip break. The columella has been extended, and there is improvement in columellar show. The nose was rotated and projected, and her nasolabial angle increased from 85 to 95 degrees.
In regards to her base view, there is improvement of her alar flaring and decrease in the size of her nostrils. Her asymmetric type I sheen alar base reduction improved the symmetry of her base, and there is minimal scarring in the alar facial groove and columella.
References
- American Academy of Facial Plastic and Reconstructive Surgery 2005 Membership Survey: Trends in Facial Plastic Surgery, Feb 2006. http://www.aafprs.org/media/stats_polls/aafprsMedia2006.pdf. Accessed March 3, 2008.
- Theda C. Kontis, M.D., F.A.C.S., and Ira D. Papel, Rhinoplasty on the African-American Nose Aesthetic Plastic Surgery online publication, 2002
- Ofodile FA, and James EA. Anatomy of alar cartilages in blacks. Plast. Reconstr. Surg. 1997;100(3):699-703.
- Kridel R RW, Konior RJ, Shumrick KA, Wright WK WH, et al. Advances in nasal tip surgery: The lateral crural steal. Arch Otolaryngol Head Neck Surg. 1989;115(10):1206-1212.
- Calvert JW, Brenner K, DaCosta-Iyer M, Evans GR, Daniel RK. Histological Analysis of Human Diced Cartilage Grafts. Plast Reconstr Surg, 2006;118(1):230-236.
- Gibson T, and Davis WB. The distortion of autogenous cartilage grafts: Its causes and prevention. Br J Plast Surg,1956;10:257.
- Sheen, JH, and Sheen AP. Aesthetic Rhinoplasty, 2nd Ed. St. Louis: Mosby, 1978:228-229.
- Slupchynsky, Oj, GieniuszArch M. Rhinoplasty for African American Patients; A Retrospective Review of 75 Cases. Facial Plast Surg. 2008;10(4):232-236.
- Roerich RJ, Muzaffar AR. Rhinoplasty in the African-American Patient; Plast Reconstr Surg. 2003 Mar;111(3):1322-1339.
- Haurani, M, Kenneth F, Yang, James J, A Siddiqui. 5-Fluorouracil Treatment of Problematic Scars. Plas. Recon. Surg. 2009 123(1):139-148.
