Welcome to the 6th PENN Rhinoplasty Course. It is nice to have you all here at our course, which for the first time we are having here in the Chelsea Hotel in Atlantic City. My co-course directors are Dr. Ara Chalian and Dr. Stephen Goldstein, and we would like to welcome you all.
As you know, we have a wonderful guest faculty joining us. Dr. Shan Baker from the University of Michigan, Dr. Stephen Perkins from Indiana, Dr. J. Regan Thomas, the Chairman at the University of Illinois at Chicago, Dr. Ed Williams, who is in private practice in New York, and Dr. Gary Burget from Chicago. We also have the benefit of our Penn faculty, Dr. Tim Greco, Dr. Paul Carniol, and Dr. Scott Bartlett. I want to thank them all for being here, and I want to thank you all, the audience and the participants for coming. I am looking forward to a wonderful two days talking about rhinoplasty.
My first lecture this morning is on the subject of Technical Considerations in Rhinoplasty, Modification of the Nasal Dorsum (Reduction and Augmentation) and Osteotomies. So this is a lecture discussing – in a short amount of allotted time – some technical aspects of rhinoplasty.
I am going to begin by describing my approach for taking down the nasal hump. To briefly summarize my approach: I resect the nasal hump with a scalpel and osteotome. I make fine-tuning adjustments to the profile with a scalpel and a powered rasp. I close the “open roof” by performing osteotomies and repositioning the nasal bones. I re-support the cartilage part of the profile with spreader grafts.
Now, for a little more detail:
I pre-mark the skin with a marker before I do anything else in the surgery, even before I inject any infiltrative anesthesia. I think that helps to set the desired hump reduction, to guide things. Once I have lifted the skin-soft tissue envelope and achieve the appropriate surgical exposure, I like to do the hump reduction in an en bloc or one-piece fashion. I do it that way because it allows me to carefully examine what I have taken out, which helps to achieve a precise result.
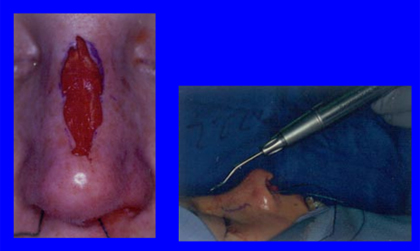
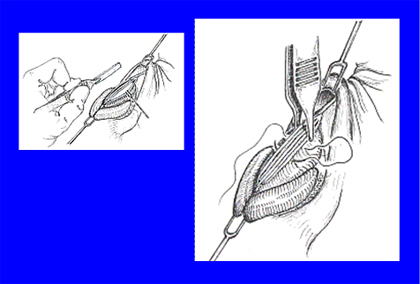
So, using a scalpel I incise or cut (but do not yet remove) the cartilage part of the bump. Once I have incised the cartilage part, I seat the bone knife, the osteotome, at the junction, the bony-cartilaginous junction as shown in this slide (above). Then while I guide the osteotome, my assistant will gently tap, tap; tap, tap, and that will result in the cutting of the bony part too. That accomplishes and completes the initial phase of the hump reduction.
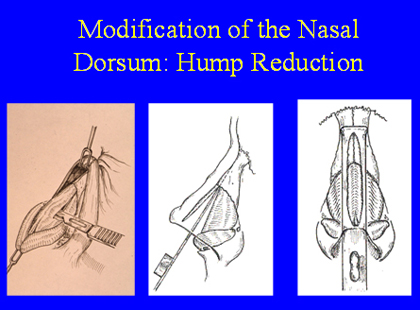
We always calculate to take a hump off that stops short of our desired final result. It is preferable to leave the last 10 percent of the hump reduction to a calibrated, careful scalpel excision for the cartilaginous portion, and a precise powered rasping and smoothing of the bony portion. We’lld iscuss this below.
I like to do the hump reduction this way because I think it is the most precise way to do it. After the initial, en bloc portion of hump reduction, I can look at the patient’s new profile, and also I can examine what I have taken off for any irregularities. This can be a helpful guides as I proceed to the last phase of the hump reduction, the final smoothing of the patient’s nasal profile.


Here’s a patient before and after. You can see on her side view that we did a very significant hump reduction. This is a very happy patient, as you might imagine.
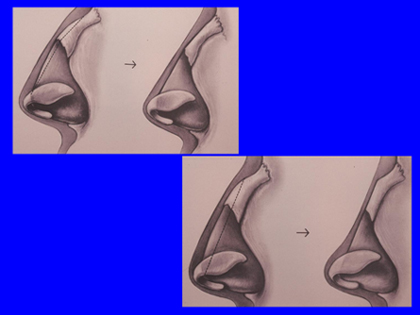
One technical aspect of taking down the hump is that you have to be aware of the difference of the skin thickness along the bridge. Right at the tip, the skin is thicker, and right at the root of the nose between the eyes the skin is thick.
But at the bone-cartilage junction, the skin is very thin. And so you plan an angled excision, you take out a little bit less at that point where the skin is thin. If you take what could be called a straight line excision of the bump (illustrated in the diagram on the lower right in the slide above), then you will get a scooped-out nose, but if you take out more of an angled excision (top right diagram in the slide above), then you will get the desired result, a nice, strong, natural-looking profile.
Now one thing that I have been doing recently is taking down the hump under direct vision. Traditionally it has been done in an endonasal fashion where you don’t watch the hump, but you just do it by feel. I have done that for many years quite successfully, but about 2 years ago Dr Thomas asked me to write a textbook chapter on the subject of “Open versus Closed Rhinoplasty.” In doing some research in preparation of this chapter, I came across an article written by Dr. Wayne Larrabee from Seattle. Dr. Larrabee wrote a chapter entitled “Open Rhinoplasty in the Upper Portion of the Nose”, and I would just direct you to some comments that he made.
The point of this is that if all you are doing is taking down the bump, then maybe you don’t need to do an open rhinoplasty if it is a conservative profile reduction, but if you have the nose open anyway for other technical reasons, then why not look at what you’re doing and do this under direct visualization? So that would be, I think, a teaching point and a take-home point from this lecture.
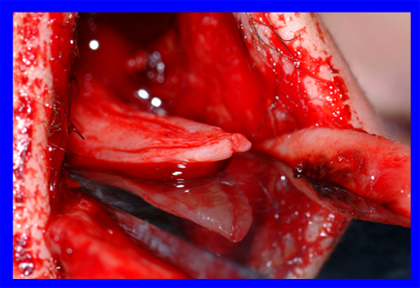
And so I have actually started to do that. And here is what it looks like. You can see exactly where the osteotome is placed, and that can help you in making fine adjustments when undertaking the bony hump reduction.
The right size is an 8-10 mm osteotome, larger is problematic. You can see this being performed in this picture where you can really see what I’m seeing, that I have incised the cartilage and the osteotome is seated right at that bone cartilage junction, and as my assistant gently tap, tap; tap, taps the osteotome, I will see this slowly advance, and I will be able to make little microchanges to the path of my osteotome and complete the desired hump reduction.
And there are good reasons to do that. A very common problem that I see when people come to me from elsewhere for revision rhinoplasty is that too much was taken from the bony part. The part that we are trying to cut with the osteotome, that part is actually thicker and harder than the deeper part of the bone. So if your osteotome is not extremely sharp, there is an increased risk that the bone knife will dive deep and take out too much bone, like this patient here, where they took out too much bone but not enough of the cartilage part of the profile,

So the idea of watching the bony hump reduction, of not only doing it by feel but also by visualization, so that you can see it happening and make adjustments as needed to the trajectory of the osteotome, I think that is a useful thing.
One of the reasons I like to take this out in one piece is that I can look at it, and as you can see on this bump, there is a little piece that did not come out cleanly, and so I will need to reduce that. That will happen sometimes, and that is why we have rasps. Now there is a rasp that I use called a powered rasp. It has a reciprocating speed of approximately 15,000 RPM, and it reciprocates back and forth approximately 2 mm. So it is a very exact, very precise tool.
What that allows me to do is that if I see one little spot where there is a little rough edge or a little place that did not come out cleanly, I can smooth that down under direct vision and very exactly. This is, in my opinion, much superior to a manual rasp, where you are relying on your own hand to move the rasp back and forth. If you think about woodworking as an analogy, if you are going to use a hand sander for manual sanding versus powered sanding, a powered instrument is more exact, and you have a better chance of getting a really great result, and so my preference for equipment for rasping is to use a powered rasp.
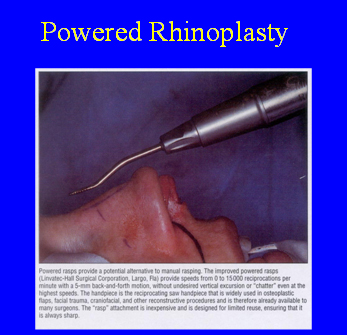
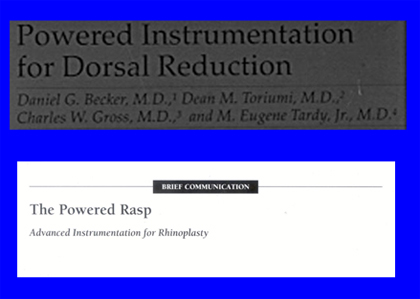
Now, I have done a lot of research and writing about powered instrumentation with my mentors and colleagues, Dr. Dean Toriumi, Dr. Charlie Gross, and Dr. Eugene Tardy.
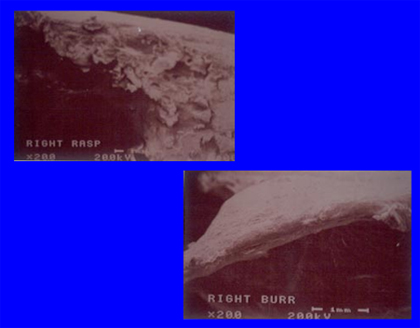
We have tried various different instruments, and we have even looked at the nasal bones of cadavers after rasping with manual instrument and then after using a powered instrument, and you can see how the one is so rough, and the one with the powered instrument is so smooth. It makes sense that that would be true, but also seeing it sometimes is believing it, and so I hope that I can persuade you about that.



There are a lot of different powered instruments including powered burs, but in my opinion, the powered rasp is the most effective. It is the right smoothing tool. If you were going to smooth something in the woodshop, you would use a smoothing back-and-forth motion to sand something down, and that is the right motion to smooth an edge. Here again is a picture of the powered rasp. We use one that is an air-driven one from the operating room wall.


And then here is a patient who has very thin skin, and even before surgery you can see how you can see the bony edges. You are just going to want to be very careful in a patient like this, that you smooth everything down, and so after taking down this hump in the way I have described, we also then will use the powered rasp to finely smooth it, and we really fuss over this area to do everything we can to get it just right. This is a 4-year after surgery result, and I think you can see the nice improvement, and he is certainly quite happy too.
So, to review, when I take a bump down, I don’t aim to take it down to the intended final profile with the first pass of the scalpel and the osteotome. On the contrary, I aim to take down a bit less than that, and then I take it down the rest of the way, little by little, to the final profile. For the bony part, we use the powered rasp, and for the cartilage part, we use a fresh scalpel and just take little slivers of cartilage until we get it just right. We keep the computer imaging pictures of the goal of surgery in the room, so that we rely not just on our memory but the actual pictures that we reviewed with the patient where we have established the desired goal.
Spreader Grafts
Now, when talking about hump reduction, we really should talk about spreader grafts, because the cartilaginous part of the nose needs support after hump reduction. If you don’t put in spreader grafts after hump reduction, then that cartilaginous part of the nose may collapse. Most of you in the audience are of course familiar, but for the medical students who are here, spreader grafts are little cartilage grafts, most often taken from deeper inside the nose, usually from the septum, and they are placed in a space that is in between the septum and the upper lateral cartilage.
Here is a picture, a diagram of these cartilages being sewn into place. We are not making the nose wider with spreader grafts, we are just maintaining the width and strength of the nose. If you don’t do that, then there is a risk that the hump reduction may cause the nose to over-narrow.

Here is a patient who had a very big nose and a big hump taken down, and you really need to re-support this middle area by putting these spreader grafts in place. Which is what we did!
Spreader grafts are a subject worthy of an entire lecture, but I would like to make just one important comment about them here. One of our guests at this meeting, Dr. Steve Perkins, I know that in his lecture he will reiterate the need for spreader grafts when humps are taken down. Dr. Perkins has a 30-year history of performing rhinoplasty. He has been in practice for a long time, and as he will tell you, he used to do, and he has written about in the literature, he used to do rhinoplasty through a closed approach and did not use spreader grafts in these patients. However, he has written and lectured more recently that he saw many of these patients come back with problems; specifically where he needed to go back and put in spreader grafts. He now has switched to placing spreader grafts routinely when the hump is taken down. I think you will agree that someone with 30 years of experience is someone we should listen to. He used to do it the other way, and now he is placing spreader grafts when he takes down the bump. I believe it is best to learn this lesson.


And then, here’s another patient, who had a nasal bump and a twisted nose. We used the spreader grafts for support, and also to help create straightness. After we took down her bump, we also not only created a wonderful profile but also placed a spreader graft just on the left side to balance the nose from the front, and you can see she has a wonderfully straight nose and a beautiful profile. I think you will agree that the spreader grafts did not widen her nose, did not make her nose too wide.
Osteotomies
Another technical element related to hump reduction are osteotomies. After you have taken down the hump, you get what is called an open roof – you can see a diagram of this here. All that means is that you have taken off the top of the roof, so to speak, and so the roof of the nose is open. The surgeon needs to reposition the nasal bones to narrow them a bit, to close the roof of the nose. Otherwise that creates a deformity that is very unpleasing.
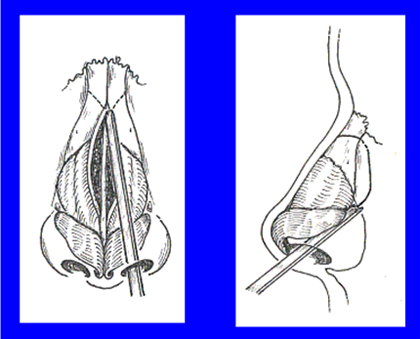
So, to do this, to close the open roof, we will perform osteotomies, or cuts in the nasal bone, to allow repositioning. We usually make two cuts – a bone cut in the middle, which are shown in this first picture and is called a medial osteotomy, and then on the side, which is shown in the second picture above and are called lateral osteotomies.
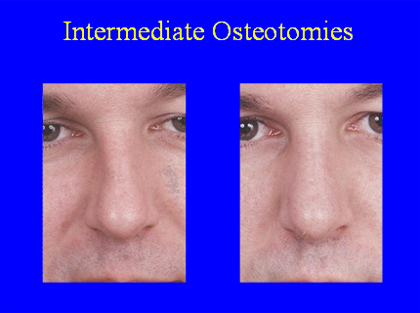
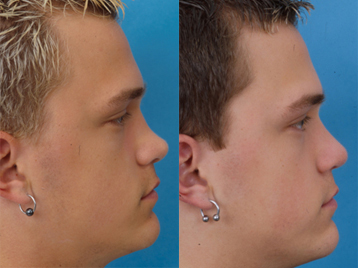
If there is a patient who has a twist of the nose because of an inherent twist of the bone itself, we might need to even make a middle cut which is called an intermediate osteotomy. That was done in this patient here and had a nice straightening result for him.
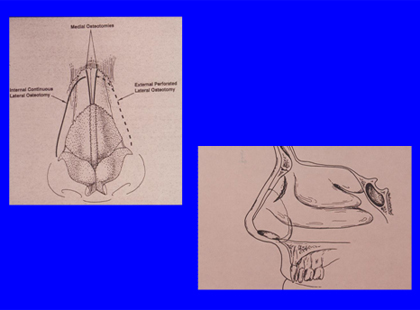
Now there are two ways to make an osteotomy. One is the endonasal, or inside-the-nose approach – that is our preference. Others prefer a percutaneous – or through-the-skin approach. This is used by some surgeons but I believe they are in the minority, especially in the US.
It is important to use an osteotome of the proper size. One that is too large can do substantial damage to the soft tissue. You know, if you use an osteotome that is too big, then you can also damage the soft tissue of the nose. I believe this happens, that some surgeons are using osteotomes that I feel are too large. I have had patients come in and say that they have a friend who had a rhinoplasty, and she was swollen and bruised for weeks. That is simply not what we see in our practice.
Part of that relates to using very meticulous technique, using local anesthesia with epinephrine so that we don’t get a lot of bleeding, but also that comes from using instruments that are not too big, so that they don’t traumatize the soft tissue.
Here is a picture of an osteotome from an operating room elsewhere, and let me tell you, these are big osteotomes! They are approximately 4-5 mm wide and they have a big guard. I would personally never use an osteotome this size in a rhinoplasty. As you cut through the bone, these are going to really injure and cut the tissue and create bleeding and swelling.
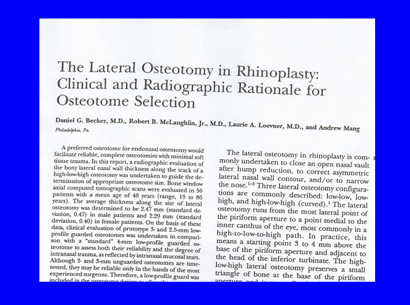
We actually did some research in which we measured the thickness of the bone along the path of the osteotome. We wanted to identify a scientific basis for the selection of an osteotome, to determine an ideal width for an osteotome . As you can see here, our research was published in the journal Plastic and Reconstructive Surgery, and was chosen as a highlighted article for the journal’s YearBook that year. Our research also resulted in a new surgical instrument, offered by Medtronic Corporation, which is coincidentally called the Becker Osteotome. I should disclose that I receive no royalties or payments from the sale of this instrument.
In any case, for this research study we obtained x-rays such as this one, from healthy adult men and adult women, and we measured how thick the bone is along the line of an osteotomy. It turns out that the bone in this area is about 2.5 to 3 mm thick, so an osteotome need not be any wider than that.
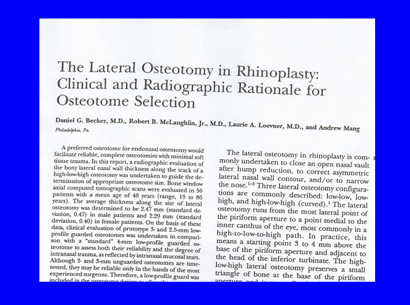
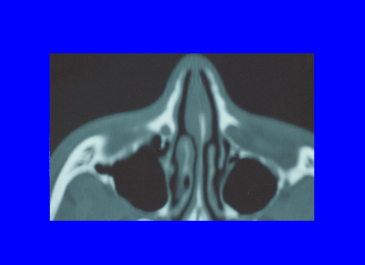
In any case, for this research study we obtained x-rays such as this one, from healthy adult men and adult women, and we measured how thick the bone is along the line of an osteotomy. It turns out that the bone in this area is about 2.5 to 3 mm thick, so an osteotome need not be any wider than that.
The osteotomes you see shown here are – from the right – 2 mm, 2.5, 3 and 4 mm wide. The 2-mm osteotome with a small guard is a little bit too small. You can use a 2-mm osteotome without a guard, but some surgeons find that difficult. A 2.5 or 3-mm osteotome is just right and, a 4 mm osteotome is a bit larger than needed.
As this diagram shows, if you use a 4-mm osteotome, then you will cause tearing of the inner lining 95% of the time. If you use a 3-mm guarded osteotome, then about 30% of the time you will get a little tear of the lining, and if you use a 2.5 mm osteotome, which very successfully cuts the nasal bone (because that is how thick it is), then you only get a little tear 5% of the time.
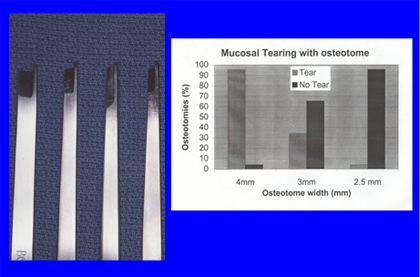
So as I mentioned, we worked with an instrument company to design 2.5 and 3-mm osteotomes with a little guard. That little guard is just so that you can engage the bone and so the osteotome won’t slip off, so it makes it a very reliable instrument and a reliable technique. We find that using these osteotomes, we get really minimal tearing of the tissue, and we also had very minimal bruising and swelling, and the patients continue to be quite pleased.
Now in the last few minutes, we are going to talk about the opposite of taking down the bump; we are going to talk about augmenting the bridge. This is a subject that could encompass an hour, but we only have a few minutes, so we will really just hit the highlights.
There are some people, whether by an injury or from previous surgery or from birth, they have a bridge that is too low for them, and they would like it built up. We like to use cartilage for that, either taken from inside the nose (the septum), or also from behind the ear. For more severe cases we will use rib.
Above are photos of a patient who – after a traumatic injury – had a nose that was too short and also scooped. By building up the bridge, we were able not only to give him a more masculine-appearing profile, but also to cause the tip to get pushed down a little bit and thereby lengthen the nose.
Here is a young lady who had a softball injury (Patient 6), and you can see we created a more feminine-appearing nose for her.


As this diagram shows, if you use a 4-mm osteotome, then you will cause tearing of the inner lining 95% of the time. If you use a 3-mm guarded osteotome, then about 30% of the time you will get a little tear of the lining, and if you use a 2.5 mm osteotome, which very successfully cuts the nasal bone (because that is how thick it is), then you only get a little tear 5% of the time.
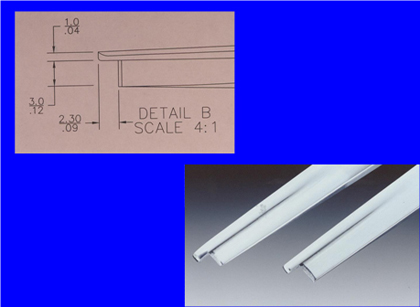
So as I mentioned, we worked with an instrument company to design 2.5 and 3-mm osteotomes with a little guard. That little guard is just so that you can engage the bone and so the osteotome won’t slip off, so it makes it a very reliable instrument and a reliable technique. We find that using these osteotomes, we get really minimal tearing of the tissue, and we also had very minimal bruising and swelling, and the patients continue to be quite pleased.

Now in the last few minutes, we are going to talk about the opposite of taking down the bump; we are going to talk about augmenting the bridge. This is a subject that could encompass an hour, but we only have a few minutes, so we will really just hit the highlights.
There are some people, whether by an injury or from previous surgery or from birth, they have a bridge that is too low for them, and they would like it built up. We like to use cartilage for that, either taken from inside the nose (the septum), or also from behind the ear. For more severe cases we will use rib.
Above are photos of a patient who – after a traumatic injury – had a nose that was too short and also scooped. By building up the bridge, we were able not only to give him a more masculine-appearing profile, but also to cause the tip to get pushed down a little bit and thereby lengthen the nose.

Here is a young lady who had a softball injury, and you can see we created a more feminine-appearing nose for her.

Here’s a woman who had a motor vehicle accident, as I recall, and she had what we call Boxer’s nose deformity, where the middle part of her nose has collapsed. We rebuilt that with a triple-layer graft using a closed approach, and you can see the wonderful profile that we achieved for her.

This is a very delightful woman, delightful patient. She had a problem where her nose completely collapsed, and so this is a very complicated problem that is really a reconstructive surgery, and we used rib cartilage for her, and we really needed to rebuild the entire nose. You can see that we got a pretty nice result for her. She was certainly quite pleased.

And finally, this is a gentleman who suffered a traumatic injury to his nose and then developed a severe infection in his nose after this injury. These two things together caused his nose to collapse, and we also rebuilt his nose with rib. We don’t have time to discuss rib cartilage reconstruction in too much detail now, but basically you rebuild the L-strut of the nose and rebuild an entire structure over the existing nose.
So this is an overview of modification of the bridge – reduction and augmentation – and osteotomies. This is a lot of material to cover in the allotted time, and so this lecture was just an overview. I will certainly discuss the application of these techniques in my other lectures today and tomorrow, and I will certainly look forward to talking to each of you if any of you have any questions. Thank you very much.
